Pulmonary vascular anatomy & anatomical variants
IntroductionOther Section
- Introduction
- Pulmonary arterial system
- Right pulmonary artery
- Left pulmonary artery
- Pulmonary capillary bed
- Pulmonary veins
- Bronchial arteries
- Applied anatomy
- Conclusions
- Acknowledgements
- Footnote
- References
The primary pulmonary circulation comprising of the pulmonary arterial tree, extensive capillary bed and pulmonary venous tree, connected in series is a low pressure, high capacitance system which provides large surface area for gas exchange. The bronchial circulation which provides nutrients to the lungs is a low capacitance, high pressure system and normally does not participate in blood oxygenation.
Pulmonary arterial systemOther Section
- Introduction
- Pulmonary arterial system
- Right pulmonary artery
- Left pulmonary artery
- Pulmonary capillary bed
- Pulmonary veins
- Bronchial arteries
- Applied anatomy
- Conclusions
- Acknowledgements
- Footnote
- References
The main pulmonary artery arises from the right ventricular outflow tract and courses posteriorly and superiorly to the left of and posterior to the aorta (1). Below the aortic arch, it bifurcates into right and left main pulmonary arteries at the level of the carina. The right and left pulmonary arteries divide into 2 lobar branches each, and subsequently into segmental and sub segmental branches. Segmental and sub segmental pulmonary arteries generally parallel segmental and sub segmental bronchi and are named according to the bronchopulmonary segments that they feed (Figure 1).
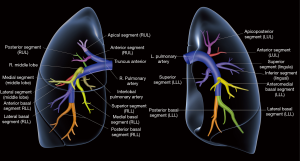
The bronchopulmonary segment is a functionally and anatomically discrete portion of lung supplied by its own segmental bronchus and artery. The right lung has 3 lobes divided into 10 segments: the right upper lobe has apical, posterior and anterior segments, middle lobe has medial and lateral segments and the lower lobe has superior (apical) and 4 basal segments (anterior, medial, posterior and lateral). The left lung has 8 segments with the left upper lobe apical and posterior segments supplied by a common segmental bronchus and the left lower lobe anterior and medial segments supplied by a common segmental bronchus; the left upper lobe has apicoposterior and anterior segments, lingula has superior and inferior segments and the lower lobe has superior (apical) and 3 basal segments (anteromedial, posterior and lateral) (2).
The root of the lungs where the pulmonary arteries and bronchi enter and pulmonary veins leave the lungs, is referred to as the pulmonary hilum. The relationship of the pulmonary artery, main stem bronchus, and pulmonary veins at the hilum is well defined and constant (3). The left hilum is higher than the right in 97% of individuals. There is however great variation in the segmental and sub segmental arterial pattern. In 1959, Cory & Valentine documented variant arterial anatomy in 524 lungs or lobes at pulmonary resection, noting 14 variations in the right upper lobe, 5 variations in the right middle lobe, 6 variations in the right lower lobe, 29 variations in the left upper lobe and 4 variations in the left lower lobe (4).
Right pulmonary arteryOther Section
- Introduction
- Pulmonary arterial system
- Right pulmonary artery
- Left pulmonary artery
- Pulmonary capillary bed
- Pulmonary veins
- Bronchial arteries
- Applied anatomy
- Conclusions
- Acknowledgements
- Footnote
- References
The right pulmonary artery is within the pericardium for more than three-fourths of its length and runs horizontally to the right behind the ascending aorta and superior vena cava. As it leaves the pericardium, it lies anterior and inferior to the right main stem bronchus. After the origin of its first branch, the truncus anterior, the interlobar pulmonary artery runs inferiorly between the bronchus intermedius posteriorly and the superior pulmonary vein anteriorly. It turns posteriorly behind the origin of the middle lobe bronchus, continues as the common basal trunk and terminates in branches to the basal segments. The truncus anterior supplies the right upper lobe; and the interlobar artery, which runs in the interlobar fissure, supplies the right middle and right lower lobes.
Segmental arteries of right upper lobe
In the most common arterial pattern there is a single, high anterior trunk or truncus anterior supplying the apical and anterior segments and a single ascending branch supplying the posterior segment. Other common variants include trifurcation of the truncus anterior to supply the apical, anterior and posterior segments and 2 separate branches to the posterior segment. Occasionally there may be segmental supply to the upper lobe from the middle lobe or superior segmental right lower lobe artery.
Segmental arteries of right middle lobe
The middle lobe segmental arteries arise from the anteromedial aspect of the right interlobar artery as it courses anterior to the bronchus intermedius. There may be separate or common origin of the arteries to the medial and lateral segments of the middle lobe.
Segmental arteries of right lower lobe
Typically, the superior segment of the right lower lobe receives one segmental artery, arising posteriorly from the interlobar artery, following which the common basal trunk divides into 2 terminal branches which subsequently divide to supply the medial basal, posterior basal, lateral basal and anterior basal segments. In up to 70% of cases, the second branch of right lower lobar artery is the medial basal branch. Occasionally there may be 2 separate branches to the apical segment.
Left pulmonary arteryOther Section
- Introduction
- Pulmonary arterial system
- Right pulmonary artery
- Left pulmonary artery
- Pulmonary capillary bed
- Pulmonary veins
- Bronchial arteries
- Applied anatomy
- Conclusions
- Acknowledgements
- Footnote
- References
The left pulmonary artery passes inferiorly and posteriorly and exits the pericardium below the aortic arch at the ligamentum arteriosum. It arches over and behind the left mainstem bronchus and curves around three-fourths of the circumference of the left upper lobe bronchus. The left main pulmonary artery has a long extra pericardial length before giving off its first branch. It continues as the common basal trunk and terminates in branches to the basal segments.
Segmental arteries of left upper lobe
Anatomic variations on the left are far more common than on the right. Number of pulmonary arterial branches to the left upper lobe vary from 2 to 7. Most commonly, the apicoposterior and anterior segments receive blood supply from an apicoanterior trunk. In some cases, the arteries for apical, anterior and posterior segments originate separately. In 80% of cases, lingula is supplied by one branch of the pulmonary artery, which gives off arteries for superior and inferior segments.
Segmental arteries of left lower lobe
In most cases, there is a single superior segmental artery after which the pulmonary artery is referred to as “basal part”. It then divides into two terminal divisions which branch into segmental and subsegmental branches supplying the antero-medial, posterior and lateral basal segments.
Pulmonary capillary bedOther Section
- Introduction
- Pulmonary arterial system
- Right pulmonary artery
- Left pulmonary artery
- Pulmonary capillary bed
- Pulmonary veins
- Bronchial arteries
- Applied anatomy
- Conclusions
- Acknowledgements
- Footnote
- References
The pulmonary arterial tree subdivides rapidly and branches into pulmonary capillaries, which form a dense web in the alveolar wall, increasing the maximum surface area available for gas-exchange. In addition to pulmonary arterial branches running alongside a bronchus there are “supernumerary” arteries which leave the axial branches at irregular but frequent intervals to enter the lung parenchyma, resulting in the pulmonary arterial tree having many more branches than the bronchial tree (5,6). Due to thin walls and smaller amount of smooth muscle, the pulmonary capillaries are more distensible and compressible than systemic vessels and offer much less resistance to blood flow. Following gas exchange in the capillary beds oxygenated blood is returned to the heart by pulmonary veins.
Pulmonary veinsOther Section
- Introduction
- Pulmonary arterial system
- Right pulmonary artery
- Left pulmonary artery
- Pulmonary capillary bed
- Pulmonary veins
- Bronchial arteries
- Applied anatomy
- Conclusions
- Acknowledgements
- Footnote
- References
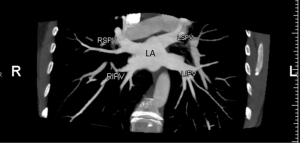
Typically, there are four pulmonary veins with superior and inferior pulmonary veins on either side, draining into the left atrium (7). The distal segments of the pulmonary veins are intrapericardial. The right superior vein drains the right upper lobe and right middle lobe, right inferior vein drains the right lower lobe; left superior vein drains the left upper lobe and lingula and left inferior vein drains the left lower lobe.
They enter the mediastinum below and anterior to the pulmonary arteries. The ostia of the inferior pulmonary veins are more posterior and medial than those of the superior pulmonary veins, and the ostia of the left pulmonary veins are located higher than those of the right pulmonary veins.
In both hilae the superior pulmonary vein is the most anterior structure and the inferior pulmonary vein is the most inferior structure. The parenchymal pulmonary vein branches, run within interlobular septa and do not parallel the segmental or sub segmental pulmonary artery branches and bronchi.
There may be anomalous drainage into the left atrium or systemic veins. On the left side there may be convergence of the left pulmonary veins into a short or long common trunk that drains into the left atrium. Anatomic variants on the right side are less common and include accessory veins such as accessory right middle or upper pulmonary veins draining independently into the left atrium (Figures 2-4).
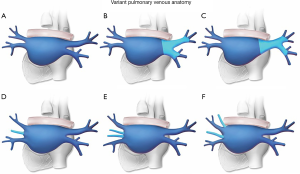

Partial anomalous pulmonary venous return (PAPVR) into a systemic vein produces a left to right shunt. On the right side an anomalous pulmonary vein may drain into the superior vena cava, azygos vein, coronary sinus, or inferior vena cava. In left-sided PAPVR left upper lobe pulmonary veins form a vertical vein that joins the left brachiocephalic vein or the coronary sinus.
Bronchial arteriesOther Section
- Introduction
- Pulmonary arterial system
- Right pulmonary artery
- Left pulmonary artery
- Pulmonary capillary bed
- Pulmonary veins
- Bronchial arteries
- Applied anatomy
- Conclusions
- Acknowledgements
- Footnote
- References
Most commonly, there are 3 bronchial arteries, 2 on the left side and 1 on the right side arising from the anterolateral aspect of the descending aorta or from intercostal arteries located within 2 to 3 cm distal to the left subclavian artery. They form a rich anastomotic network with the pulmonary arterial circulation at the level of the lobar or segmental bronchi. A substantial portion of bronchial venous blood enters the pulmonary veins (1).
Applied anatomyOther Section
- Introduction
- Pulmonary arterial system
- Right pulmonary artery
- Left pulmonary artery
- Pulmonary capillary bed
- Pulmonary veins
- Bronchial arteries
- Applied anatomy
- Conclusions
- Acknowledgements
- Footnote
- References
Computed tomography (CT) anatomy
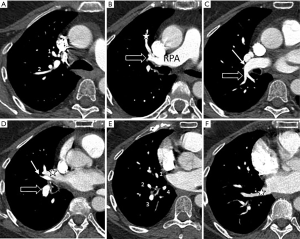
CT pulmonary angiography (CTPA) is recommended by the American College of Radiology (8) for the evaluation of patients with suspected pulmonary embolism due its high sensitivity and specificity, easy accessibility after hours, and its ability to offer alternative diagnoses.
Pulmonary arteries typically follow their respective segmental and sub segmental bronchi and it is important to identify branches to the 10 right and 8 left bronchopulmonary segments, looking for variations in anatomy, particularly in the upper lobes. Keep in mind that the branches to the middle lobe and lingula arise from the anterior aspect of the interlobar artery whereas the branch to the superior segment of the lower lobes arises from the posterior aspect of the interlobar artery. Figures 5,6 demonstrate pulmonary arterial anatomy on cross-sectional imaging.

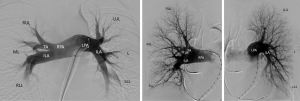
IR anatomy
Catheter-based pulmonary angiography is indicated for evaluation and treatment of various congenital and acquired diseases, such as pulmonary arteriovenous malformations (PAVMs), pulmonary artery stenosis and aneurysm, pulmonary vein stenosis, anomalous pulmonary venous return, and pulmonary artery neoplasm. Knowledge of pulmonary vascular anatomy is imperative for complete and accurate assessment of these studies. Figure 7 demonstrate pulmonary arterial anatomy on flush and selective right and left pulmonary arteriograms.
ConclusionsOther Section
- Introduction
- Pulmonary arterial system
- Right pulmonary artery
- Left pulmonary artery
- Pulmonary capillary bed
- Pulmonary veins
- Bronchial arteries
- Applied anatomy
- Conclusions
- Acknowledgements
- Footnote
- References
Knowledge of pulmonary vascular anatomy on cross-sectional and angiographic images is essential for diagnosis and treatment of various conditions such as pulmonary thromboembolism and pulmonary arterio-venous malformations.
AcknowledgementsOther Section
- Introduction
- Pulmonary arterial system
- Right pulmonary artery
- Left pulmonary artery
- Pulmonary capillary bed
- Pulmonary veins
- Bronchial arteries
- Applied anatomy
- Conclusions
- Acknowledgements
- Footnote
- References
Erin Moore, MA, Medical Illustrator, Sr. Graphic Designer, University of Texas Southwestern Medical Center, Dallas, Texas.
FootnoteOther Section
- Introduction
- Pulmonary arterial system
- Right pulmonary artery
- Left pulmonary artery
- Pulmonary capillary bed
- Pulmonary veins
- Bronchial arteries
- Applied anatomy
- Conclusions
- Acknowledgements
- Footnote
- References
Conflicts of Interest: The authors have no conflicts of interest to declare.
ReferencesOther Section
- Introduction
- Pulmonary arterial system
- Right pulmonary artery
- Left pulmonary artery
- Pulmonary capillary bed
- Pulmonary veins
- Bronchial arteries
- Applied anatomy
- Conclusions
- Acknowledgements
- Footnote
- References
- Frechette E, Deslauriers J. Surgical anatomy of the bronchial tree and pulmonary artery. Semin Thorac Cardiovasc Surg 2006;18:77-84. [Crossref] [PubMed]
- Sealy WC, Connally SR, Dalton ML. Naming the bronchopulmonary segments and the development of pulmonary surgery. Ann Thorac Surg 1993;55:184-8. [Crossref] [PubMed]
- Warren WH, Milloy FJ. Pulmonary vascular system and pulmonary hilum. Thorac Surg Clin 2007;17:601-17. [Crossref] [PubMed]
- Cory RA, Valentine EJ. Varying patterns of the lobar branches of the pulmonary tree. Thorax 1959;14:267-80. [Crossref] [PubMed]
- Gil J. The normal lung circulation. State of the art. Chest 1988;93:80S-2S. [PubMed]
- Elliott FM, Reid L. Some New Facts About the Pulmonary Artery and Its Branching Pattern. Clin Radiol 1965;16:193-8. [Crossref] [PubMed]
- Porres DV, Morenza OP, Pallisa E, et al. Learning from the pulmonary veins. Radiographics 2013;33:999-1022. [Crossref] [PubMed]
- Expert Panels on Cardiac and Thoracic Imaging, Kirsch J, Brown RKJ, et al. ACR Appropriateness Criteria(R) Acute Chest Pain-Suspected Pulmonary Embolism. J Am Coll Radiol 2017;14:S2-12. [Crossref] [PubMed]


