Right ventricular failure predicted from right bundle branch block: cardiac magnetic resonance imaging validation
Introduction
Despite advances in treatments, heart failure continues to have a 5-year mortality of 50% which is worse than that of many cancers (1). Although left ventricular (LV) systolic dysfunction has been widely studied, the emphasis on RV systolic dysfunction has been limited despite known association with adverse outcomes (2-4). As electrocardiographic parameters for RV dysfunction still remain largely unknown, echocardiography remains the first line study to evaluate for right ventricular (RV) dysfunction. Echocardiographic assessment of RV function comes with several limitations. The quantification of volume and mass by echocardiography relies on geometrical assumptions that do not apply to ventricles undergoing cardiac remodeling (5,6). This is not the case for cardiac magnetic resonance imaging (CMRI) where geometrical assumptions do not apply and the results are known to be more accurate and reproducible (7-9). This makes CMRI the reference standard in assessing RV function. Studies have established its superiority over the more readily available echocardiography (10). The availability of CMR, however, remains limited to certain institutions largely due to the need for higher technical expertise and cost effectiveness.
Left bundle branch block (LBBB), by altering the sequence of LV depolarization, has been noted to be associated with both LV systolic and diastolic dysfunction (11,12). Right bundle branch block (RBBB), however, has not been proven to be associated with RV dysfunction. A previous study hypothesized R’ duration to be independently association with systolic dysfunction by using echocardiography (13). We here try to go one step forward by studying electrocardiographic RBBB features and analyze their association with RV systolic dysfunction using CMRI.
Methods
A total of 995 patients between the ages 30 to 90 years underwent CMR over a period of 3 years at New York Methodist hospital. Patients with known congenital heart disease, paced rhythm, primary pulmonary hypertension and prior valve surgeries were excluded as these conditions have been known to be independently associated with RV systolic dysfunction. Although patients with coronary artery disease and LV systolic dysfunction were not excluded, we compared their incidences between the two groups. After application of exclusion criteria, twelve lead ECGs of included patients were reviewed for the presence of RBBB. MUSE editor software (General Electrical Company, Fairfield, CT, USA) is used to measure the ECG parameters (closest to 0.02 sec). Software generated ECG readings were analyzed by same investigator blinded to CMR results. AVL AHA/ACCF/HRS recommendations for interpretation of ECG were strictly followed to define a complete RBBB. All of these were needed to be satisfied for us to define it as complete RBBB (14).
- QRS duration >120 msec (all our patients were >18 years of age);
- rsr’, rsR’ or rSR’ pattern in V1 or V2;
- Duration of S wave > duration of R wave or greater than 40 msec in leads I and V6.
If a pure dominant R wave was present with or without a notch in V1, the requirement of normal R peak time in V5 and V6 but >50 msec in V1 was required to designate it as a complete RBBB.
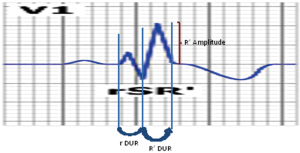
The ECGs of the included patients were reviewed for the following parameters. QRS duration, R and R’ duration and amplitude were obtained from precordial lead V1; and S duration and amplitude were obtained from lead I (Figure 1).
Measurement of RV systolic parameters including ejection fraction (EF), stroke volume, RV end systolic volume (RVESV), RV end diastolic volume (RVEDV) and RV mass were obtained in all the subjects using a 1.5 Tesla Siemens Avanto CMR scanner. Short-axis steady-state free precession (SSFP) images covering the RV from the tricuspid valve to the RV apex were obtained for the evaluation of RV function. Two, three and four chamber SSFP images were also acquired. The CMR parameters of the cine SSFP sequence were as follows: bandwidth 125 kHz, flip angle 45, TR/TE 3.7/1.6 ms, field of view 32 cm, image matrix 256 × 192, and slice thickness 8 mm. RV volumes were calculated by manually tracing the endocardium in successive short axis views during end systole and diastole. Papillary muscles were excluded during calculation of RV volume and included during calculation of RV mass. End systolic and diastolic volumes parameters were indexed to body surface area as well (15). LV parameters were also calculated. Patient clinical and demographics features were obtained from the patient on day of the procedure and via the hospital electronic medical record.
Statistics
Continuous data was reported as mean ± SD. Two sample t-tests were used to assess the differences in continuous variables, Fischer’s exact test or chi square tests were used to assess the difference in discrete variables. Rank correlations and scatter diagrams between individual CMR parameters and ECG parameters were done using medcalc for windows, version 12.5 (medcalc software, Olstead, Belgium). Sensitivity, specificity and area under the curve (AUC) were calculated using analysis of the receiver operating characteristic (ROC) curve. Different threshold values that suggest the best sensitivity and specificity were selected on the interactive dot diaphragm on ROC curve using the medcalc software.
Results
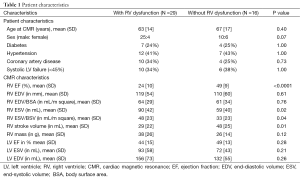
A total of 995 consecutive patients underwent CMRI over 3-year period at our institution. Patients were referred to our CMRI center for the assessment of LV function (40%), viability (25%), valvular disease (25%) or cardiac masses (10%). About 945 out of 995 patients met the inclusion criteria. Closest ECGs from the date of CMRI were reviewed for presence of RBBB. A total of 45 patients (4.7%) were identified to have completed RBBB by standard definition. The higher proportion of RBBB in our population than generation population (4.7% vs. ≈1%) was expected considering the patients who underwent CMRI were being evaluated for cardiac pathologies. CMRI results from these patients were evaluated. RVEF <40% was defined as RV systolic dysfunction. RVEF >40% acted as a control group. About 29 out of 45 patients (64%) were found to have RV dysfunction (mean EF 24±10) and 16 patients (36%) with normal EF acted as control (mean EF 48±8). Clinical and demographic features of the subjects are included in Table 1.
Full table
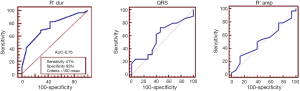
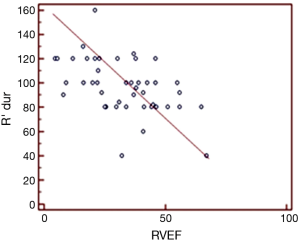
Statistically significant difference was not found in the incidences of any of the baseline characteristics. Three patients in the RV dysfunction group were on anti-arrhythmic medication but none of them were on class 1 agents. Mean age was 63±14 and 67±17 respectively for the subjects with and without RV systolic dysfunction. Mean RV EF calculated by CMR was 24±10 and 49±9 in patients with and without RV dysfunction, respectively. RV dysfunction group was noted to have larger RVESV as compared with control group (P=0.02) which supports the Frank-Starling law. RV stroke volume was noted to be smaller in RV dysfunction group, as expected. RV end diastolic volume, LV EF, LV end systolic and LV end diastolic volumes were not noted to be statistically significantly different. ECG comparisons in both the groups are summarized in Table 2. QRS duration and R’ duration in lead V1 and S wave duration in I/AVL were higher in the RV dysfunction group compared to that with no RV dysfunction, however only R’ duration was statistically significant (103±22 vs. 84±18, P<0.05). The sensitivity and specificity of ECG parameters in RBBB in predicting RV systolic dysfunction is represented in Figure 2. R’ duration greater than 100 msec predicted RV systolic dysfunction (Figure 3) with specificity of 93% and sensitivity of 41% (AUC on ROC curve of 0.761 and P≤0.001). R’ duration was also found to have inverse correlation with RV EF r=−0.49, P=0.0007).

Full table
Discussion
Increased RV pressures and volumes in RV dysfunction can cause myocardial stretching which in turn can lead to stress on the right bundle and purkinje network (13). This can lead to conduction delay across the path of the right bundle branch causing RBBB. In our study, we saw increased end systolic RV volumes in the RV dysfunction group which resulted in delay in the latter part of right bundle branch leading to prolonged R’ duration.
RV dysfunction is implicated in clinical deterioration and cardiovascular mortality (16-18). Echocardiography is the most commonly used tool for assessment of RV dysfunction. However, echocardiographic calculations are limited by geometrical assumptions. Though echocardiographic parameters like tricuspid annular plane systolic excursion, FAC (fractional area change), MPI (myocardial performance index) are useful in assessing RV function, they are known to be technically challenging and incomplete (19,20).
CMRI is recognized as the most accurate way to assess RV function. However, the equipment, long study period, high level of technical knowledge requirement and lack of remuneration prevents the use of CMRI in everyday practice (21). A lot of our patients who undergo CMRI are referred from other institutions due to its unavailability at other institutions. Hence, the importance of defining ECG criteria for RV systolic function can’t be undermined due to its wider application.
Prolonged QRS duration in the presence of LBBB has been known to be predictor for poor LV systolic function (22). This, however, could not be stated for prolonged QRS in RBBB (23). The association of QRS duration in RBBB with RV dysfunction was previously reported mostly in congenital heart disease (24-26). A previous study, in its novel approach, used echocardiography to define ECG criteria for RV dysfunction (13). However, it was limited by small sample size and the limitations of two dimensional echocardiography as mentioned above. We validated some of their findings by using CMRI and went further by comparing different CMRI characteristics like RVESV, RVEDV, RV stroke volume and that could help us in determining the mechanism of action which could possibly lead to these ECG changes. We found R’duration >100 msec to be highly sensitive for RV dysfunction in our study. Also, we saw a statistically significant inverse correlation between R’ duration and RVEF.
Limitations: the major limitation of the study is the small sample size. This is largely due to the difficult task of finding patients who undergo CMRI and have co-existant complete RBBB. The prevalence of complete RBBB in the general population is low (27). The incidence of RBBB in our patient population was 4.7%. To achieve a bigger sample size, a prospective model is required where patients with RBBB undergo CMR to evaluate for RV systolic dysfunction. This will be a challenging task to accomplish.
Although R’ duration was found to be highly specific, the low sensitivity for RV dysfunction limits its use as a screening tool. Also, the retrospective design and the fact that this is a single center study are other limiting factors in the design of this study.
Conclusions
We here found prolonged R’ duration in lead V1 to have a highly specific inverse correlation to RV systolic function. This gives further weight to the hypothesis that RV systolic dysfunction by leading to increased RVESV can alter the morphology of myocardium by myocardial stretching and affect the conduction system of the right bundle branch. Hence, we conclude that the evaluation for RV systolic dysfunction should begin with a simple ECG. If prolonged R’ duration is seen in lead V1 on an ECG, it should prompt further evaluation with echocardiography and CMR if clinically indicated.
In an environment where healthcare costs are a big concern, we propose a simple and a cost-saving approach for predicting RV systolic function by using an easily measurable ECG parameter.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The research was approved by Institutional Review Board and has been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
References
- Braunwald E. Heart failure. JACC Heart Fail 2013;1:1-20. [Crossref] [PubMed]
- Kjaergaard J, Akkan D, Iversen KK, et al. Right ventricular dysfunction as an independent predictor of short- and long-term mortality in patients with heart failure. Eur J Heart Fail 2007;9:610-6. [Crossref] [PubMed]
- Anavekar NS, Skali H, Bourgoun M, et al. Usefulness of right ventricular fractional area change to predict death, heart failure, and stroke following myocardial infarction (from the VALIANT ECHO Study). Am J Cardiol 2008;101:607-12. [Crossref] [PubMed]
- de Groote P, Millaire A, Foucher-Hossein C, et al. Right ventricular ejection fraction is an independent predictor of survival in patients with moderate heart failure. J Am Coll Cardiol 1998;32:948-54. [Crossref] [PubMed]
- Kronik G, Slany J, Mösslacher H. Comparative value of eight M-mode echocardiographic formulas for determining left ventricular stroke volume. A correlative study with thermodilution and left ventricular single-plane cineangiography. Circulation 1979;60:1308-16. [Crossref] [PubMed]
- Teichholz LE, Kreulen T, Herman MV, et al. Problems in echocardiographic volume determinations: echocardiographic-angiographic correlations in the presence of absence of asynergy. Am J Cardiol 1976;37:7-11. [Crossref] [PubMed]
- Doherty NE 3rd, Seelos KC, Suzuki J, et al. Application of cine nuclear magnetic resonance imaging for sequential evaluation of response to angiotensin-converting enzyme inhibitor therapy in dilated cardiomyopathy. J Am Coll Cardiol 1992;19:1294-302. [Crossref] [PubMed]
- Longmore DB, Klipstein RH, Underwood SR, et al. Dimensional accuracy of magnetic resonance in studies of the heart. Lancet 1985;1:1360-2. [Crossref] [PubMed]
- Higgins CB. Which standard has the gold? J Am Coll Cardiol 1992;19:1608-9. [Crossref] [PubMed]
- Grothues F, Smith GC, Moon JC, et al. Comparison of interstudy reproducibility of cardiovascular magnetic resonance with two-dimensional echocardiography in normal subjects and in patients with heart failure or left ventricular hypertrophy. Am J Cardiol 2002;90:29-34. [Crossref] [PubMed]
- Xiao HB, Lee CH, Gibson DG. Effect of left bundle branch block on diastolic function in dilated cardiomyopathy. Br Heart J 1991;66:443-7. [Crossref] [PubMed]
- Tabuchi H, Kawai N, Sawayama T. Estimation of left ventricular systolic function based on the electrocardiograms in cases with left bundle branch block. J Cardiol 1998;31:23-30. [PubMed]
- Adams JC, Nelson MR, Chandrasekaran K, et al. Novel ECG criteria for right ventricular systolic dysfunction in patients with right bundle branch block. Int J Cardiol 2013;167:1385-9. [Crossref] [PubMed]
- Surawicz B, Childers R, Deal BJ, et al. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: part III: intraventricular conduction disturbances: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society. Endorsed by the International Society for Computerized Electrocardiology. J Am Coll Cardiol 2009;53:976-81. [Crossref] [PubMed]
- Maceira AM, Prasad SK, Khan M, et al. Reference right ventricular systolic and diastolic function normalized to age, gender and body surface area from steady-state free precession cardiovascular magnetic resonance. Eur Heart J 2006;27:2879-88. [Crossref] [PubMed]
- Shah PK, Maddahi J, Staniloff HM, et al. Variable spectrum and prognostic implications of left and right ventricular ejection fractions in patients with and without clinical heart failure after acute myocardial infarction. Am J Cardiol 1986;58:387-93. [Crossref] [PubMed]
- Juillière Y, Barbier G, Feldmann L, et al. Additional predictive value of both left and right ventricular ejection fractions on long-term survival in idiopathic dilated cardiomyopathy. Eur Heart J 1997;18:276-80. [Crossref] [PubMed]
- Ghio S, Gavazzi A, Campana C, et al. Independent and additive prognostic value of right ventricular systolic function and pulmonary artery pressure in patients with chronic heart failure. J Am Coll Cardiol 2001;37:183-8. [Crossref] [PubMed]
- Kaul S, Tei C, Hopkins JM, et al. Assessment of right ventricular function using two-dimensional echocardiography. Am Heart J 1984;107:526-31. [Crossref] [PubMed]
- Miller D, Farah MG, Liner A, et al. The relation between quantitative right ventricular ejection fraction and indices of tricuspid annular motion and myocardial performance. J Am Soc Echocardiogr 2004;17:443-7. [Crossref] [PubMed]
- Hergan K, Globits S, Schuchlenz H, et al. Clinical relevance and indications for cardiac magnetic resonance imaging 2013: an interdisciplinary expert statement. Rofo 2013;185:209-18. [PubMed]
- Das MK, Cheriparambil K, Bedi A, et al. Prolonged QRS duration (QRS >/=170 ms) and left axis deviation in the presence of left bundle branch block: A marker of poor left ventricular systolic function? Am Heart J 2001;142:756-9. [Crossref] [PubMed]
- Uyguanco ER, Mirandi A, Qureshi G, et al. Prolongation of QRS duration and axis deviation in the right bundle branch block are not markers for left ventricular systolic dysfunction. Int J Angiol 2010;19:e83-5. [Crossref] [PubMed]
- Gatzoulis MA, Till JA, Somerville J, et al. Mechanoelectrical Interaction in Tetralogy of Fallot. QRS Prolongation Relates to Right Ventricular Size and Predicts Malignant Ventricular Arrhythmias and Sudden Death. Circulation 1995;92:231-7. [Crossref] [PubMed]
- Egidy Assenza G, Valente AM, Geva T, et al. QRS duration and QRS fractionation on surface electrocardiogram are markers of right ventricular dysfunction and atrialization in patients with Ebstein anomaly. Eur Heart J 2013;34:191-200. [Crossref] [PubMed]
- Book WM, Parks WJ, Hopkins KL, et al. Electrocardiographic predictors of right ventricular volume measured by magnetic resonance imaging late after total repair of tetralogy of Fallot. Clin Cardiol 1999;22:740-6. [Crossref] [PubMed]
- Bussink BE, Holst AG, Jespersen L, et al. Right bundle branch block: prevalence, risk factors, and outcome in the general population: results from the Copenhagen City Heart Study. Eur Heart J 2013;34:138-46. [Crossref] [PubMed]


