
Ethnic and sex-based differences in outcomes after out-of-hospital cardiac arrest: a glimpse of the largest municipal healthcare system in the United States
Highlight box
Key findings
• Among patients resuscitated after an out-of-hospital cardiac arrest (OHCA), neither sex nor ethnicity predicted discharge survival.
• No sex differences in end-of-life preferences were found.
• Women had higher cardiac arrest hospital prognosis scores (CAHP) scores than men predicting poor neurological performance after OHCA.
What is known and what is new?
• Data on ethnic and sex-based differences in discharge survival after OHCA have been conflicting.
• Our study findings are distinct as neither sex nor ethnicity predicted discharge survival and no sex differences in end-of-life preferences were found.
What is the implication, and what should change now?
• Since women had higher CAHP scores, underlying etiologies should be investigated in future studies.
• Although a larger study may provide better power for detecting disparities, in this unique population studied, socioeconomic factors and competing comorbidities likely served as bigger drivers for OHCA rather than ethnicity or sex.
Introduction
Out-of-hospital cardiac arrest (OHCA) is defined as a cessation of cardiac mechanical activity that is confirmed by the absence of signs of circulation at an out-of-hospital setting (1). The high mortality and morbidity inherent to cardiac arrests correspond with the significant global healthcare burden imposed by OHCA, wherein discharge survival is <10% and discharge with meaningful functional status <7% (2). This is further complicated by reports of significant ethnic and sex-based disparities in outcomes observed in some retrospective studies (2-5).
Over the years, data on ethnic and sex-based differences in discharge survival and neurological outcomes after OHCA have been conflicting. Some studies have found women to have a higher likelihood of return of spontaneous circulation (ROSC) despite unfavorable factors peri-arrest but a lower likelihood to be discharged alive with good neurological function (3,6-9). In other studies, women have demonstrated a favorable neurological outcome and higher odds of survival compared to men (10-13). Similarly, reports of ethnicity-based disparities in OHCA outcomes have challenged the quality of care and uniformity in healthcare interventions offered to patients (4,14). Among populations that are socioeconomically disadvantaged, underserved, and ethnically diverse, the implications of OHCA can be greater.
The aim of this study was to investigate ethnic and sex-based disparities in patient outcomes after OHCA upon admission to a safety net tertiary hospital within the largest municipal healthcare system in the United States. Within this inner-city patient population, we also sought to evaluate for sex differences in end-of-life preferences and to identify factors that reliably predicted survival to hospital discharge and survival at 1-year after OHCA. We present the following article in accordance with the STROBE reporting checklist (15) (available at https://cdt.amegroups.com/article/view/10.21037/cdt-22-371/rc).
Methods
Study design and patient population
We conducted a retrospective cohort study on data collected from New York City Health + Hospitals/Jacobi, a tertiary public hospital within New York City Health + Hospitals (NYC H + H) system, which is the largest municipal healthcare system in the United States (US) and the largest safety net hospital system in the country (16). Nearly one million individuals seek care within the NYC H + H system each year, of which an overwhelming majority represents the low-income strata and/or ethnically disadvantaged groups, with 32% of care seekers being uninsured, 35% being Medicaid beneficiaries, and 70% being people of color (16). With respect to ethical conduct of the study, it was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and was approved by the regional institutional review board of the Biomedical Research Alliance of New York (IRB#21-12-378-11), with a waiver of informed consent for the retrospective analysis.
Eligibility criteria
Patients >18 years of age who were successfully resuscitated after an OHCA with sustained ROSC between January 2019 and September 2021 and were brought by emergency medical services (EMS) to NYC H+H/Jacobi were included. The study duration was determined based on the duration the electronic medical record system (Epic systems, Verona, WI, USA) was available at our institution, ensuring that no medical records were missed due to a lack of integration with the prior electronic medical record system. We excluded patients who met any one of the following criteria: (I) patients with missing data on gender, age, location of arrest, outcome of resuscitation, and duration of ROSC; (II) patients who failed to achieve ROSC or did not sustain ROSC until admission and transfer of care to the receiving hospital; and (III) patients who suffered in-hospital cardiac arrest.
Data sources
Study data were obtained from electronic medical records (Epic systems, Verona, WI, USA) by using relevant international classification of diseases diagnostic codes and search terms. Data were fully password-protected and anonymized before extraction. Search algorithm used is included in the Appendix 1.
Data extraction
Patient charts were reviewed, and data were extracted from EMS response sheets based on standardized Utstein definitions by investigators SN, AK, SM, and HN blind to one another, and cross-checked for accuracy and congruency by a fifth investigator, RT (1) Data were abstracted for patient characteristics, event characteristics, and outcomes of the arrest (1). Study definitions for variables extracted are provided in the Appendix 1. Baseline patient characteristics included age, sex, and ethnic background. OHCA event characteristics and outcomes included location of arrest, if it was witnessed, administration of bystander cardiopulmonary resuscitation (CPR), EMS reflex time in minutes, presence of an initial shockable rhythm, epinephrine dose in milligrams, duration of resuscitation in minutes, performance of a 12-lead electrocardiogram (EKG), and presence of ST-segment elevation on the initial EKG. Data abstracted from hospital course included arterial pH on first lab draw, administration of targeted temperature management (TTM), performance of coronary angiography, and do not resuscitate (DNR) orders and withdrawal of life-sustaining therapy (WLST) orders given after admission to the hospital. The cardiac arrest hospital prognosis (CAHP) score was calculated for each study subject and survival at 1-year after discharge was recorded when applicable (1,17,18). For patients who lacked follow-up data at 1-year after discharge, phone calls were made to number(s) provided in the patient chart or to the long-term care facility/nursing homes to which the patients were discharged from their index hospital admission to determine survival at 1-year. The CAHP score was used to help predict an unfavorable or poor neurological outcome, defined by cerebral performance category (CPC) 3 (severe disability), 4 (vegetative state), or 5 (death) at the time of discharge. The risk of poor neurological outcome was predicted to be low with scores <150, moderate for 150–200, and high if >200 (17,18).
Statistical synthesis and analysis
Data were processed and analyzed anonymously to maintain patient confidentiality. Normally distributed data are presented as mean (standard deviation) (SD) and non-normal data as median [interquartile range (IQR)]. Categorical data are presented as frequency (percentage of the total). Categorical variables were compared with a χ2 or Fisher exact test and described using odds ratios (ORs) and 95% CIs. The Mann-Whitney or Student’s t-test was used to evaluate continuous variables, with a P value of less than 0.05 to represent the statistical significance threshold. Logistic regression was performed for two primary outcomes: predictors of survival at hospital discharge and survival to one year post discharge. Variables included into the logistic regression were selected based on pre-existing literature data as well as baseline characteristics that were likely to confound our results. There was no need for advanced variable selection models as the overall number of variables was within reasonable range (stepwise approach was attempted producing very similar results to ones of the final statistical analysis). Kaplan-Meier curves were used as a non-parametric method for survival analysis and Log-rank test was performed to compare the two arms with a censoring time at 1 year. All statistical analysis was performed using STATA/IC 16.1.
Results
Patient characteristics
Out of the 648 patients screened, 154 patients were successfully resuscitated after an OHCA, met the predefined eligibility criteria, and were included in the final analysis. An Utstein style flowchart of out-of-hospital cardiac arrests brought to the hospital by EMS is detailed in Figure 1. Patient selection process, including number of patients excluded with reasons for exclusion is detailed in Figure S1. Characteristics of included patients and event characteristics are detailed in Table 1. The social vulnerability index of the census tract to which each patient included in this study belonged is presented in Figure 2. The median social vulnerability index was “High” at 0.876. In our study population, 74 (48.1%) were women and 80 (51.9%) were men. Women were significantly older with a mean age of 69.8 years (SD:14.9) compared to men 64.2 years (18.4); P=0.04. A total of 39.2% of women and 35% of men were Black or African American, 37.8% of women and 12.5% of men were Latino/Hispanic, 12% of women and 15% of men were white, 2.7% of women and 3.8% of men were Asian, and 6.8% and 33.8% of women and men, respectively identified as another ethnicity.
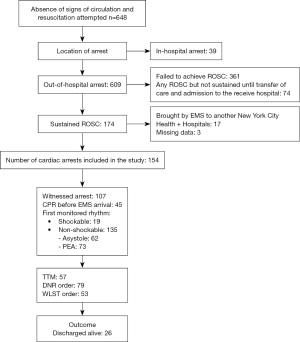
Table 1
| Variables | Sex | P value | |
|---|---|---|---|
| Women (n=74) | Men (n=80) | ||
| Age (years), mean (standard deviation) | 69.8 (14.9) | 64.2 (18.4) | 0.04 |
| Ethnicity, n (%) | |||
| White | 9/74 (12.2) | 12/80 (15.0) | 0.65 |
| Asian | 2/74 (2.7) | 3/80 (3.8) | 0.72 |
| African American | 29/74 (39.2) | 28/80 (35.0) | 0.71 |
| Hispanic/Latino | 28/74 (37.8) | 10/80 (12.5) | 0.004 |
| Other | 5/74 (6.8) | 27/80 (33.8) | <0.001 |
| Location of arrest, n (%) | |||
| Place of residence | 39/74 (52.7) | 43/80 (53.8) | 0.90 |
| Public location | 8/74 (10.8) | 11/80 (13.8) | 0.62 |
| Other | 27/74 (36.5) | 26/80 (32.5) | 0.90 |
| Witnessed, n (%) | 48/74 (64.9) | 59/80 (73.8) | 0.23 |
| Bystander CPR, n (%) | 18/74 (24.3) | 27/80 (33.8) | 0.19 |
| EMS response time (minutes), median (IQR) | 8 (6–11) | 10 (6–14) | 0.38 |
| Initial shockable rhythm, n (%) | 8/74 (10.8) | 11/80 (13.8) | 0.58 |
| Defibrillation, n (%) | 18/74 (10.8) | 28/80 (35.0) | 0.15 |
| ST-elevation, n (%) | 9/74 (12.2) | 4/80 (5.0) | 0.11 |
| Resuscitation duration (minutes), median (IQR) | 28.5 (14.25–35.75) | 17 (14.25–40) | 0.70 |
| In-hospital parameters and outcomes, n (%) | |||
| Arterial Ph, median (IQR) | 7.16 (7.06–7.30) | 7.17 (7.02–7.32) | 0.48 |
| CAHP score, median (IQR) | 237 (207–262) | 167 (175–244) | 0.02 |
| TTM | 28/74 (37.8) | 29/80 (36.3) | 0.84 |
| CAG | 2/74 (2.7) | 2/80 (2.5) | 0.94 |
| DNR order | 37/74 (50.0) | 42/80 (52.5) | 0.76 |
| WLST order | 28/74 (37.8) | 25/80 (31.3) | 0.39 |
| Discharge survival | 11/74 (14.9) | 15/80 (18.8) | 0.45 |
CPR, cardiopulmonary resuscitation; IQR, interquartile range; EMS, emergency medical services; CAHP, cardiac arrest hospital prognosis score; TTM, targeted temperature management; CAG, coronary angiography; DNR, do not resuscitate; WLST, withdrawal of life-sustaining therapy.
Overall, distribution for location of arrest was largely similar among women and men, with nearly half of each group suffering a cardiac arrest in a place of residence (52.7% of women and 53.8% of men; (P=0.90) and 10.8% of women and 13.8% of men (P=0.62) found in a public location at the time of the arrest. Frequency of witnessed arrest (64.9% women vs. 73.8% men; P=0.23), median (IQR) duration of EMS reflex time {8 [6–11] min in women vs. 10 [6–14] min in men; P=0.38}, presence of an initial shockable rhythm (10.8% women vs. 13.8% men; P=0.58), presence of ST-segment elevation (12% women vs. 5% men; P=0.11), arterial pH [median (IQR): 7.16 (7.06–7.30) in women vs. 7.17 (7.02–7.32) in men; P=0.48], median duration of resuscitation [median (IQR): 28.5 (14.25–35.75) min in women vs. 17 (14.25–40) min in men; P=0.70] were similar in women and men. Also, there were no significant sex-differences in rates of defibrillation (10.8% women vs. 35% men; P=0.15), administration of bystander CPR (24.3% women vs. 33.8% men; P=0.19, targeted temperature management (37.8% women vs. 36.3% men; P=0.84) and rates of urgent coronary angiography between the sexes (2.5% women vs. 2.7% men; P=0.94). Other rhythms observed were pulseless electrical activity (PEA) secondary to hypoxia from respiratory failure in 22.9% (31/135), PEA from unclear etiology in 8.9% (12/135), metabolic acidosis and hyperkalemia secondary to missed hemodialysis in 2.2% (3/135), myocardial infarction in 14.3% (5/135 patients), sepsis in 8.15% (11/135), opioid use in 6.7% (9/135), polysubstance intoxication in 1.5% (2/135), asystole from hypoxia in 17.8% (24/135), asphyxia from hanging in 0.7% (1/135), unclear etiology in 17/135, myocardial infarction in 2/135, crack cocaine in 2.2% (3/135), barbiturate ingestion in 0.7% (1/135), polysubstance use in 2.96% (4/135), carbon monoxide poisoning from burns in 0.7% (1/135), hypovolemia from bleeding in 0.7% (1/135), acidosis from missed hemodialysis in 5.18% (7/135), traumatic in 0.7% (1/135).
Clinical outcomes
The rate of survival to hospital discharge was similar between women and men [(11/74) 14.9% in women vs. (15/80) 18.8% in men; P=0.45] after successful resuscitation from an OHCA. Of the 26 patients who survived to hospital discharge, on one-year follow-up, 22 were alive and 4 were lost to follow-up. Kaplan-Meier curve for survival to hospital discharge is presented in Figure 3. Despite similar discharge survival rates, women had significantly higher CAHP scores compared to men [median (IQR): 237 (207–262) in women vs. 167 (175–244) in men; P=0.02] and therefore carried a higher risk of poor neurological outcome at the time of hospital discharge. Graphical representation of sex differences in CAHP scores is presented in Figure 4. After admission to the hospital, women and men received DNR (50% of women vs. 52.5% of men; P=0.76) and WLST orders (37.8% of women vs. 31.3% of men; P=0.39) at similar rates (Table 1).
Amongst Hispanics/Latinos, more women suffered an OHCA compared to men (women: 28//74 vs. men: 10/80; P=0.004) and when ethnicity was categorized as “other,” more men suffered an OHCA. However, on multivariable analysis, ethnic background [odds ratio (OR): 0.80; 95% confidence interval (CI): 0.58–1.12; P=0.19] and sex (OR: 0.84; 95% CI: 0.30–2.36; P=0.74) were not found to be significant predictors of survival to hospital discharge (Table S1). Age was found to be a significant independent predictor; wherein younger age was associated with a higher likelihood of discharge survival (OR: 0.96; 95% CI: 0.93–0.99; P=0.01). Similarly, presence of an initial shockable rhythm was predictive of discharge survival (OR: 7.12; 95% CI: 1.52–33.3; P=0.01).
On long-term follow-up, both age (OR: 0.93–099; P=0.04) and initial shockable rhythm (OR: 7.26; 95% CI: 1.57–33.5; P=0.01) persisted as significant independent predictors of survival at one-year after hospital discharge (Table S2).
Discussion
The present study evaluated ethnic and sex-based differences in outcomes in 154 patients successfully resuscitated from an OHCA and brought to our hospital. Our study findings can be summarized as follows: (I) ethnic background and sex were not found to be predictors of survival to hospital discharge; (II) women had significantly higher CAHP scores compared to men after successful resuscitation from an OHCA; (III) no significant differences in end-of-life care preferences were found between women and men; and (IV) age and initial shockable rhythm independently predicted survival to hospital discharge and survival at one-year after discharge. The novelty of this study lies in this unique patient population originating from a large metropolitan city and admitted to a tertiary care public hospital, wherein ethnic background and sex did not predict discharge survival unlike previously published reports (3,6-9). It is likely that socioeconomic factors served as bigger drivers for OHCA outcomes rather than ethnic background and sex.
The results of our study evaluating ethnic and sex-based differences in outcomes after OHCA are significantly different compared to previously published reports. In a retrospective study, Mody et al. examined gender-based differences in outcomes after OHCA in 4,875 participants enrolled from two large trials. Survival to hospital discharge was significantly lower in women (22.5% in women versus 36.3% in men, P<0.001; adjusted OR: 0.78; 95% CI: 0.66–0.93; P=0.005) and women tended to have worse neurological outcomes compared to men (survival with good neurological function at the time of hospital discharge: 29.6% in women versus 38.9% in men, P=0.002) (3). In another retrospective analysis of 1,667 patients from the International Cardiac Arrest registry, Karlsson et al. found male gender to be significantly associated with a higher discharge survival after OHCA (OR 1.34; 95% CI: 1.01–1.78) but not with a better neurological outcome (OR 1.24; 95% CI: 0.92–1.67) (5). Additionally, in a meta-analysis conducted by Lei et al. evaluating sex differences in survival after OHCA, women had a lower likelihood of both discharge survival (OR 0.73, 95% CI: 0.62–0.86) and favorable neurological outcomes (OR 0.62, 95% CI: 0.47–0.83) compared to males (8). In respect to ethnic differences, Moeller et al. in their analysis of patients from the CARES (Cardiac Arrest to Enhance Survival) registry found Black individuals to have a significantly lower discharge survival compared to White individuals after successful resuscitation from OHCA (4). Similarly, Becker et al., in their retrospective analysis of 6,451 patients found the Black community to have a significant lower adjusted survival rate after nontraumatic OHCA compared to Whites (14).
The significant ethnic and sex-based disparity in outcomes after OHCA observed in the above-mentioned studies compared to ours can be explained by several factors. First, the study populations in these reports were relatively larger. Although, we did not find a sex difference in discharge survival after OHCA, our study shared a similar theme, wherein women had significantly higher CAHP scores predicting a worse neurological outcome compared to men. Second, based out of The Bronx, New York, our patient population differed from the study populations used in these registry-based studies. Additionally, The Bronx represents an area of underserved and socio-economically disadvantaged patients, irrespective of ethnicity (19,20). Placed low on the socioeconomic rung compared to other regions in the US, The Bronx ranks last among all 62 counties of New York state in health outcomes, quality of life, and important health and socioeconomic factors (21). Although prior studies have shown disparities between Black and White individuals and attributed it to differences in underlying health pre-arrest, and care received prior to the arrival of EMS such as lower rates of bystander CPR among Blacks and delays in notifying EMS personnel, it is possible that our overall study population might have been subjected to one or more of these factors due to which a difference between ethnicities was not detected (22). Therefore, it is likely that within this unique patient population, socioeconomic factors including a lack of routine access to timely healthcare, and a significant burden of competing comorbidities could have served as bigger drivers for OHCA outcomes instead of ethnic background or sex. Additionally, being registry-based reports, these studies could have been influenced by registration bias. Accessible and affordable healthcare, including timely monitoring and management of cardiovascular risk factors in the ambulatory setting can help facilitate risk reduction in this socioeconomically disadvantaged population and improve OHCA outcomes. Additionally, educating the community on recognizing cardiac arrest, promptly calling EMS, care that can be provided prior to the arrival of EMS, including bystander CPR can further improve outcomes after OHCA.
Our study found no significant sex differences in end-of-life care preferences. Mody et al. found women to receive a significantly higher proportion of DNR and WLST orders (32.8% versus 29.8%; P=0.03) compared to men (3). Similarly, Perman et al. found female survivors to have a higher likelihood than men to receive DNR orders within the first 24 hours of in-hospital treatment (23.4% of women versus 19.3% of men; P<0.01) after OHCA (23). In our study population, the socio-demographic constitution of patients, geographic location, availability of next of kin, goals of care discussions conducted by providers, and social determinants of health could have been influenced a lack of sex differences in end-of-life care preferences.
We found age and initial shockable rhythm to be independent predictors of survival to hospital discharge but did not find significant sex-differences in rates of bystander CPR, presence of initial shockable rhythm, rates of defibrillation, and discharge survival. Our finding is in line with previously published reports. Karlsson et al. in their multicenter registry-based study, with centers in Sweden and United Kingdom found age and initial shockable rhythm to be significant predictors of discharge survival after OHCA in their study population (5). Similarly, Wissenberg et al. in their nationwide study from Denmark identified age per 10 additional years and initial shockable rhythm as significant predictors of 30-day survival after OHCA (24). Yet, in another study conducted by Wissenberg et al. in 19,372 patients from the Danish Cardiac Arrest Registry, female sex was significantly associated with survival in patients with an initial shockable rhythm (OR: 1.31; 95% CI: 1.07–1.59). However, among those with a non-shockable rhythm, no sex-differences in survival were observed after adjusting for patient characteristics. The investigators also found to men to have a significantly higher likelihood of having a cardiac arrest out-of-home (29.4% men vs. 18.7% women; P<0.001), receive bystander CPR (32.9% men vs. 25.9% women; P<0.001), and importantly have a shockable rhythm (32.6% men vs. 17.2% women; P<0.001) (25). Similarly, in a study from Netherlands, Blom et al. found women to receive bystander CPR less frequently compared to men, (72.7% men vs. 67.9% women; P<0.001), even when OHCA was witnessed and to have a lower likelihood of an initial shockable rhythm (men 52.7% vs. 33.7% women; P<0.001) (26). Women also suffered a significantly lower likelihood of discharge survival compared to men in this study (OR: 0.49; 95% CI: 0.40–0.60; P=0.03). In comparison to these previously published studies, our study not only identified age and initial shockable rhythm as predictors of discharge survival, but also found significant association on long-term follow-up, 1-year after discharge.
Strengths and limitations
There are several strengths and limitations to this study. Importantly, this study analyzed the epidemiologic characteristics and evaluated ethnic and sex disparities in outcomes after OHCA among patients transferred to a safety net tertiary hospital within the largest municipal healthcare system in the US. One of the key strengths is the study population which represents underserved and economically disadvantaged minorities, on whom data are usually underreported and underrepresented in clinical and population science research. Our study findings are novel as they are distinct from those of registry-based studies and provoke exploration of other sociodemographic determinants of health besides ethnic background, sex, and age. Despite these strengths, considering the small sample size, we recognize that the study could have been underpowered to detect significant ethnic and sex-based differences in outcomes after OHCA. Additionally, being a single-center study, our findings cannot be easily generalized. Data on comorbidities were not available, the lack of which could have influenced the study findings. Although this was a real-world study, the retrospective design utilizing electronic medical records fares suboptimal to a prospective design that would allow for a more accurate follow-up assessment.
Conclusions
Among patients resuscitated after an OHCA, neither sex nor ethnic background predicted discharge survival, and there were no sex differences in end-of-life preferences. Notably, women had higher CAHP scores than men predicting poor neurological performance after OHCA. Although a more extensive study may provide better power for detecting these disparities, it is possible that given the unique population studied, socioeconomic factors and significant burden of competing comorbidities served as bigger drivers for OHCA rather than ethnic background or sex.
Acknowledgments
The abstract was presented at the American College of Cardiology Conference on April 2, 2022.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://cdt.amegroups.com/article/view/10.21037/cdt-22-371/rc
Data Sharing Statement: Available at https://cdt.amegroups.com/article/view/10.21037/cdt-22-371/dss
Peer Review File: Available at https://cdt.amegroups.com/article/view/10.21037/cdt-22-371/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://cdt.amegroups.com/article/view/10.21037/cdt-22-371/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Biomedical Research Alliance of New York Institutional Review Board (BRANY IRB) (IRB # 21-12-378-11) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Jacobs I, Nadkarni V, Bahr J, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa). Circulation 2004;110:3385-97. [Crossref] [PubMed]
- Tsao CW, Aday AW, Almarzooq ZI, et al. Heart Disease and Stroke Statistics-2022 Update: A Report From the American Heart Association. Circulation 2022;145:e153-639. [Crossref] [PubMed]
- Mody P, Pandey A, Slutsky AS, et al. Gender-Based Differences in Outcomes Among Resuscitated Patients With Out-of-Hospital Cardiac Arrest. Circulation 2021;143:641-9. [Crossref] [PubMed]
- Moeller S, Hansen CM, Kragholm K, et al. Race Differences in Interventions and Survival After Out-of-Hospital Cardiac Arrest in North Carolina, 2010 to 2014. J Am Heart Assoc 2021;10:e019082. [Crossref] [PubMed]
- Karlsson V, Dankiewicz J, Nielsen N, et al. Association of gender to outcome after out-of-hospital cardiac arrest--a report from the International Cardiac Arrest Registry. Crit Care 2015;19:182. [Crossref] [PubMed]
- Kim LK, Looser P, Swaminathan RV, et al. Sex-Based Disparities in Incidence, Treatment, and Outcomes of Cardiac Arrest in the United States, 2003-2012. J Am Heart Assoc 2016;5:e003704. [Crossref] [PubMed]
- Agarwal S, Presciutti A, Verma J, et al. Women have worse cognitive, functional, and psychiatric outcomes at hospital discharge after cardiac arrest. Resuscitation 2018;125:12-5. [Crossref] [PubMed]
- Lei H, Hu J, Liu L, et al. Sex differences in survival after out-of-hospital cardiac arrest: a meta-analysis. Crit Care 2020;24:613. [Crossref] [PubMed]
- Parikh PB, Hassan L, Qadeer A, et al. Association between sex and mortality in adults with in-hospital and out-of-hospital cardiac arrest: A systematic review and meta-analysis. Resuscitation 2020;155:119-24. [Crossref] [PubMed]
- Johnson MA, Haukoos JS, Larabee TM, et al. Females of childbearing age have a survival benefit after out-of-hospital cardiac arrest. Resuscitation 2013;84:639-44. [Crossref] [PubMed]
- Kitamura T, Iwami T, Nichol G, et al. Reduction in incidence and fatality of out-of-hospital cardiac arrest in females of the reproductive age. Eur Heart J 2010;31:1365-72. [Crossref] [PubMed]
- Kotini-Shah P, Del Rios M, Khosla S, et al. Sex differences in outcomes for out-of-hospital cardiac arrest in the United States. Resuscitation 2021;163:6-13. [Crossref] [PubMed]
- Feng D, Li C, Yang X, et al. Gender differences and survival after an out-of-hospital cardiac arrest: a systematic review and meta-analysis. Intern Emerg Med 2021;16:765-75. [Crossref] [PubMed]
- Becker LB, Han BH, Meyer PM, et al. Racial differences in the incidence of cardiac arrest and subsequent survival. The CPR Chicago Project. N Engl J Med 1993;329:600-6. [Crossref] [PubMed]
- Cuschieri S. The STROBE guidelines. Saudi J Anaesth 2019;13:S31-4. [Crossref] [PubMed]
- Kalyanaraman Marcello R, Dolle J, Grami S, et al. Characteristics and outcomes of COVID-19 patients in New York City's public hospital system. PLoS One 2020;15:e0243027. [Crossref] [PubMed]
- Maupain C, Bougouin W, Lamhaut L, et al. The CAHP (Cardiac Arrest Hospital Prognosis) score: a tool for risk stratification after out-of-hospital cardiac arrest. Eur Heart J 2016;37:3222-8. [Crossref] [PubMed]
- Bougouin W, Dumas F, Karam N, et al. Should We Perform an Immediate Coronary Angiogram in All Patients After Cardiac Arrest?: Insights From a Large French Registry. JACC Cardiovasc Interv 2018;11:249-56. [Crossref] [PubMed]
- Gonzalez Millan ML RO J, Sarnoff C, Martins S. Billings-Burford. Diahann Bronx Opioid Epidemic needs assessment Columbia University School of International and Public Affairs, 2018.
- Unintentional Drug Poisoning (Overdose) Deaths Quarter 1, 2021, New York City. 2021.
- Givens M, Gennuso K, Jovaag A, et al. 2019 County Health Rankings Key Findings Report. 2019.
- Wilde ET, Robbins LS, Pressley JC. Racial differences in out-of-hospital cardiac arrest survival and treatment. Emerg Med J 2012;29:415-9. [Crossref] [PubMed]
- Perman SM, Siry BJ, Ginde AA, et al. Sex Differences in "Do Not Attempt Resuscitation" Orders After Out-of-Hospital Cardiac Arrest and the Relationship to Critical Hospital Interventions. Clin Ther 2019;41:1029-37. [Crossref] [PubMed]
- Wissenberg M, Lippert FK, Folke F, et al. Association of national initiatives to improve cardiac arrest management with rates of bystander intervention and patient survival after out-of-hospital cardiac arrest. JAMA 2013;310:1377-84. [Crossref] [PubMed]
- Wissenberg M, Hansen CM, Folke F, et al. Survival after out-of-hospital cardiac arrest in relation to sex: a nationwide registry-based study. Resuscitation 2014;85:1212-8. [Crossref] [PubMed]
- Blom MT, Oving I, Berdowski J, et al. Women have lower chances than men to be resuscitated and survive out-of-hospital cardiac arrest. Eur Heart J 2019;40:3824-34. [Crossref] [PubMed]





