Cardiothoracic surgical experience in Ghana
Introduction
Most countries in Africa are beleaguered with many challenging health problems of predominantly infectious etiology. The expenditure in the control and treatment of most of these diseases takes a great toll on the struggling economies of these countries. The predominance of such communicable diseases reduces the priority assigned to non-communicable diseases in developing economies. Yet, cardiovascular disease is on the ascendancy in many developing countries and healthcare priorities need to be re-evaluated in the light of the current cardiovascular disease epidemic. Cardiovascular diseases may be congenital or acquired and often lead to significant morbidity and mortality without appropriate treatment.
Congenital heart diseases (CHD) worldwide affect 1.0% to 1.2% of all live births. In Ghana, the estimated burden of CHD is in the region of 372 per million of the population (1). The high fertility rate in much of sub-Saharan Africa leads to a disproportionate number of children born with CHD in this part of the world. Many of such children have no geographical or financial access to surgical treatment: in Ghana where the facility for treatment was available, only 20% of parents of children less than 15 years old requiring surgery for CHD were able to finance the operation within 12 months of diagnosis (2). The majority of these children may never find help and die from CHD complications. In some cases, financial hurdles turn such children into inoperable victims of CHD.
The adoption of ‘western’ lifestyles by many developing countries has brought in its wake acquired cardiovascular diseases which hitherto were not national health concerns. Consequently, cardiovascular diseases, notably hypertension and its complications, have become the number one cause of morbidity and mortality in adults in Ghana. Traditionally associated with developed countries, some 80% of all cardiovascular deaths now occur in low and middle-income countries (3). The additional burden of these cardiovascular diseases and other non-communicable diseases has worsened the already poor economies of these countries.
Several developing countries therefore are experiencing a double burden of disease. Where the facility for surgical treatment is not available, mortality resulting from this double burden of disease is significant. In Ghana, there is only one tertiary center for cardiothoracic pathology serving a population of 25 million people. Although grossly inadequate, the country’s fortunes are far better than most in sub-Saharan Africa where such a facility is non-existent. This report highlights the history of cardiothoracic surgery in Ghana, the spectrum and outcomes of treatment, and the challenges of sustaining a high level cardiothoracic program in a resource-poor setting.
History of cardiothoracic surgery in Ghana
The era of surgery without cardiopulmonary bypass (CPB)
Cardiothoracic surgery began in Ghana in the early 1960s at the Korle-Bu Teaching Hospital in Accra. Professor Charles Easmon, a general surgeon head of the Surgery Department, was the first to perform a closed mitral commissurotomy in the country. This was the first cardiothoracic operation performed in Ghana. In 1964, he became the first to perform an open-heart procedure in the country using surface cooling to achieve hypothermia. He used this approach to successfully close an atrial septal defect (ASD) in the first patient. The same approach was utilized in the second patient in an attempt to close a supposedly similar interatrial communication but the patient did not survive the operation and died shortly in the recovery room; the diagnosis had been wrong. The resulting criticism after the failed procedure was apparently harsh, being centered on the surgeon’s devotion of scarce resources to the pursuit of open heart surgery. Subsequently, lack of funding and political upheavals in the country virtually brought the open heart program to a standstill.
In the late 1960s, two cardiothoracic surgeons, Drs. Bannerjee and Mendes, ran a cardiothoracic unit, performed mostly thoracic operations and pericardiectomies. From 1972–1975, Dr. Lade Wosornu, a general surgeon, performed oesophagectomies, pleural decortications, and thoracoplasties. Also in the early 1970s, Professor ED Yeboah, a urologist with thoracic surgery experience, performed ligations for patent ductus arteriosus (PDA). From 1975–1980, Dr. Seth Bekoe a cardiothoracic surgeon trained in Italy, performed coarctation repairs, ligation of PDAs and construction of Blalock-Taussig shunts. Dr. MP Fitz-Williams, another cardiothoracic surgeon performed some operations until 1990.
The era of cardiac surgery with CPB
In January, 1989, Dr. Frimpong-Boateng returned to Ghana after his training in general, cardiothoracic and vascular surgery in Hannover, Germany. He built a team, and founded the present National Cardiothoracic Centre. The initial funding and support was by the Ghana government and the German government. The German government provided most of the initial equipment and sponsored some medical personnel from Germany (anaesthetist, nurses, perfusionist, cardiologist) who stayed for two to ten years, helped and trained Ghanaians. The Ghana government was very supportive; paid salaries of all workers except those sponsored by the German government.
Dr. Frimpong-Boateng was the first in Ghana to use the heart lung machine to replace the mitral valve in 1992. The NCTC is a dedicated center with a 30-bed ward, 2 operating theatres, a six bed intensive care unit, a six bed high dependency unit, a dedicated laboratory, cardiac catheterization, radiology, echocardiography services and a renal dialysis unit. A core team of seven cardiothoracic surgeons trained by the founder is assisted by anaesthetists, cardiologists, cardiovascular perfusionists, dedicated cardiovascular nurses, technologists and other staff to run the center.
The NCTC has served as a surgical hub for patients from the whole West Africa sub-region, receiving regular referrals from Nigeria, the Gambia, Sierra Leone, Liberia, and Togo (2). The center has witnessed a sustained growth over the years evidenced by the increasing number of out-patient and surgical patients. In 2008, out-patient attendance was 210 per week and surgical volume was 464 annually (2). In 2015, 250 out-patient attendances per week were registered and surgical volume was 635. The services at the NCTC have saved the country substantial foreign exchange with significant economic impact. The country’s foreign exchange is no longer spent sponsoring a few privileged individuals for heart surgery abroad. From the beginning, the government of Ghana gave a semi-autonomous status to the center, an important factor in the long term sustainability of the cardiac program. The center depends on internally generated funds to buy consumables and equipments and also embark on projects that are necessary to sustain the cardiovascular and the thoracic surgery program. We have a director who is the administrative and the clinical head. There are consultants in charge of thoracic, pediatric cardiac and adult cardiac and vascular surgery. Daily morning meetings are held to discuss patients before and after surgery. Management meetings which are attended by all consultants and unit heads come on quarterly to plan and find solution to recurrent and new challenges of the unit.
Spectrum of cardiovascular surgery
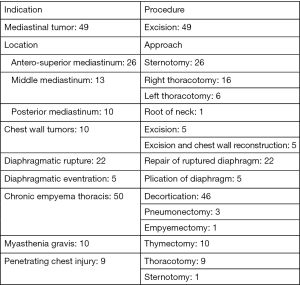
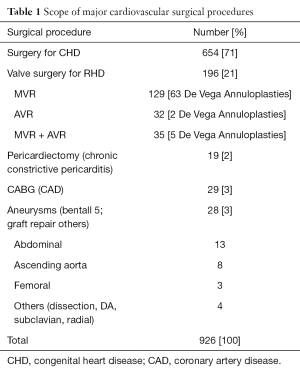
From 2002 to 2011, 2,314 surgical operations were performed at the NCTC; 1,775 (76.7%) cardiovascular operations and 539 (23.3%) thoracic operations. Surgery for CHD, rheumatic heart disease, chronic constrictive pericarditis, and aneurysms of the aorta and its abdominal branches were the major cardiovascular procedures performed (Table 1).
Full table
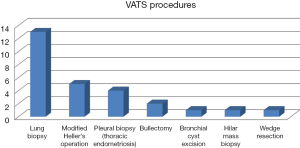
Surgery for CHD was the most common group of procedures performed (Table 1), with the creation of the modified Blalock-Taussig shunt (MBTS) for cyanotic CHD with reduced pulmonary blood flow being the commonest (Table 2).
Full table
The congenital heart population undergoing surgery during this period had a median age of 5 years (3 months to 70 years). During this period of our experience, patients with tetralogy of Fallot (TOF) were managed in a staged approach; a MBTS was followed 12–24 months later by total intra-cardiac repair. Six of 83 (7%) patients with TOF underwent primary repair during this period. Financial difficulty has been a significant limitation in obtaining surgical care for these patients. Most patients are unable to afford open heart surgery; as a result, palliation often becomes the default option. From 2011, this approach has evolved with more patients undergoing primary repair of TOF so that between 2013 and 2015, 20 of 45 (44%) TOF patients were repaired primarily. However, once symptomatic relief is obtained, a significant number of patients default on follow up until symptoms recur with growth of the child and the shunt becomes occluded or its flow becomes inadequate to sustain pulmonary blood flow.
Rheumatic heart disease has been the major indication for valve surgery. Most patients with rheumatic heart disease present late with advanced stages of valve pathology. Financial difficulty further delays surgery in a patient already severely compromised by advanced rheumatic heart disease. The choice between valve repair and valve replacement is complicated by fibrotic and calcified valve leaflets and the almost certain likelihood that should such a patient require a reoperation for failed repair, financial limitations would be prohibitive and lead to the patient’s demise. We have tended therefore to replace such valves with bi-leaflet mechanical valves, committing the patient to lifelong anticoagulation. Contrary to what is generally believed, we have shown fairly good compliance with anticoagulation in West African patients with results comparable to standards acceptable worldwide (4). In the past, we used biological valves in a few patients who returned within 3–5 years with failed prostheses and died waiting to fund a reoperation (5). Valve surgery in these patients may be isolated mitral or aortic valve replacement, double valve replacement involving aortic and mitral valves or any of these with tricuspid De Vega annuloplasty (Table 1). We have gained significant experience with the modified De Vega annuloplasty for repair of inorganic tricuspid valve regurgitation with encouraging results (6). Repair of the tricuspid valve with annuloplasty ring was used in only a few patients with unfavorable valve profile.
Chronic pericardial constriction was the predominant indication for pericardiectomy; tuberculosis accounted for 63.3% of the etiology of pericardial constriction (7). We perform this procedure through a median sternotomy with the heart lung machine on standby though we have not had to employ CPB in this procedure.
As in much of sub-Saharan Africa, coronary artery disease (CAD) is relatively uncommon and its epidemiology remains enigmatic because of a lack of reliable data and adequate diagnostic capabilities. Our surgical data would seem to support the notion that CAD is not as common as the other cardiovascular pathologies presenting for surgery: we performed coronary artery bypass grafting in only 29 patients during the study period. However, on the basis of the increasing prominence of the risk factors of CAD in Ghana, its prevalence is projected to increase in the coming decades.
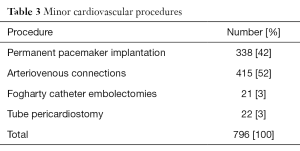
Implantation of permanent pacemakers and surgical creation of arteriovenous connections for hemodialysis were among the dominant minor procedures performed (Table 3).
Full table
The indication for the majority of the pacemakers implanted was complete heart block 277 (82.7%) of 335 cases. Also included were replacement of exhausted pulse generators in 29 (8.7%) cases, and sick sinus syndrome 18 (5.4%) among others.
Spectrum of thoracic surgical disease
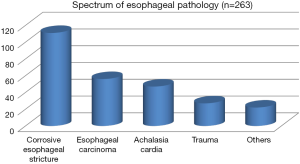
Esophageal operations dominate thoracic surgical practice in our setting. The spectrum of esophageal pathology presenting for surgery is shown in Figure 1. Corrosive esophageal injury leading to multiple strictures of the upper gastrointestinal tract is the leading cause of morbidity among thoracic surgical patients (Figure 1). Commonly, the corrosive agent is soda lime solution used in the domestic manufacture of soap. Soda lime solution is colorless and odorless and unsuspecting children mistake the bottled solution for water. In the study period, 111 patients with corrosive esophageal stricture underwent bypass of the stricture using a colon segment pedicled on the left colic artery and tunneled to the neck using the retrosternal route.
In our setting, patients with esophageal carcinoma present late; surgical intervention is often an attempt to palliate dysphagia. Of the 56 patients with esophageal carcinoma, retrosternal colon bypass was performed for 25 (44.6%) patients with advanced esophageal carcinoma. In 30 (53.6%) patients, esophagectomy (Ivor Lewis) was performed and one (1.8%) patient benefited from Orringers procedure.
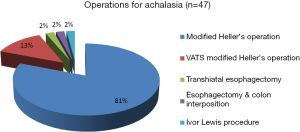
Achalasia was seen in 47 patients who were managed as shown in Figure 2.
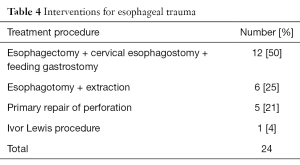
Twenty four patients suffered trauma to the esophagus. These included 14 cases of esophageal perforation and 10 cases of impacted foreign bodies (8 of which were impacted dentures). These patients underwent the procedures shown in Table 4.
Full table
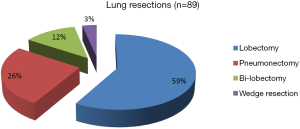
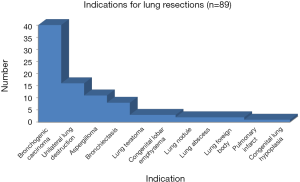
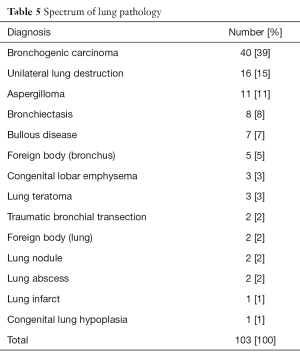
Bronchogenic carcinoma is relatively rare in our setting but constitutes the main indication for patients seeking consultation for pulmonary symptoms of surgical significance (Table 5). Unlike what is seen in western societies, a history of smoking is uncommon in these patients. Different forms of lung resection were required in these patients as shown in Figure 3.
Full table
Bronchogenic carcinoma tops the list of indications for lung resection (Figure 4). Progressively destructive infections leading to varying manifestations of unilateral destroyed lung are the next common indication for lung resection. Commonly, a tuberculous etiology is responsible.
There were 7 patients with chronic obstructive lung disease who underwent bullectomy for bullous disease of the lungs. Bronchial surgical interventions were undertaken in 7 patients; 5 patients with impacted foreign body who had failed bronchoscopic extraction and two patients with traumatic bronchial transection. Bronchotomy and foreign body extraction was performed for the 5 patients with impacted foreign bodies and repair of transection carried out in the two affected patients.
The other thoracic procedures undertaken are shown in Figure 5.
Video-assisted thoracoscopic surgery (VATS)
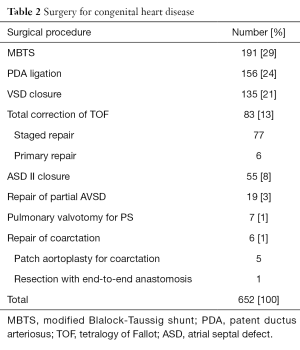
We started our VATS program in 2008. The same financial issues confronting patients in the sub-region has limited the number of patients able to access this modality of treatment. Our experience with VATS is summarized Figure 6.
Outcomes of surgical procedures
The patients reviewed here have been reported on earlier in several publications (6-12); the outcomes of some are briefly presented here. Surgical outcomes at the National Cardiothoracic Center published in peer reviewed journals are comparable internationally and have improved over the years.
Between 1991 and 2000, hospital mortality for mechanical valve replacement was 9.9% with actuarial survival of 85% at 5 years (5). Results of left heart mechanical valve replacement in children <18 years were reviewed at the Center in 2011. The outcomes have demonstrated a reduction in hospital mortality to 5.3% and actuarial survival improved to 94% at 15 years (4). Surgery for CHD formed the majority of major cardiovascular procedures done over the period. Surgery in adolescents and adults with congenitally malformed hearts made up 23% of all congenital heart surgeries performed at the Center between 1993 and 2008 (8). Hospital mortality was 3% for this patient population and this was similar to the results for CHD in children. Permanent complete heart block and junctional ectopic tachycardia are complications following congenital heart surgery. Our institutional review of all patients who had intracardiac repair of CHDs from 1993 to 2008 demonstrated an overall risk of complete heart block of 2.5% (6 of 242 patients) (9). The incidence of junctional ectopic tachycardia was 3.8% among 184 children who underwent CPB for repair of CHD between 2006 and 2010 (10). In a study to determine the outcome of surgical intervention in children born with conotruncal anomalies, hospital mortality was 0% for palliation and 4% for repair (11).
There was no hospital mortality after pericardiectomy for chronic constrictive pericarditis among 11 patients who underwent the procedure between 2000 and 2005 (7). Among 64 patients who underwent modified De Vega annuloplasty for inorganic tricuspid valve regurgitation and followed up for an average of 61.3 months, 64.1% of the patients had no postoperative tricuspid regurgitation, 28.5% had grade 1 regurgitation, and 9.4% grade 2 regurgitation. Hospital mortality was 4.7% (6).
There was no procedure related mortality was observed among 355 patients undergoing permanent pacemaker implantation between 1992 and 2009. Twenty five patients (7.0%) developed complications, the commonest being lead-electrode dislodgement (4.8%) (12).
Between 1994 and 2009, 16 patients (11 males and 5 females) presenting with esophageal perforations underwent surgical intervention. Six patients (37.5%) presented within 24 h of their injury and 10 (62.5%) presented after 24 h. Thoracotomy and intrathoracic primary repair was possible in five (31.2%) cases. Esophagectomy, cervical esophagostomy and feeding gastrostomy were carried out in 11 (68.8%). One patient (6.2%) died after oesophagectomy from overwhelming sepsis (13).
In a four year review of 603 patients admitted in the intensive care unit at the NCTC after surgery, the average length of stay of all patients within the period was 2.05 days (range, 1–14 days) (14). After open heart surgery, most patients are discharged from hospital 8 to 12 days post-operatively. They are reviewed two weeks after discharge from hospital then six weeks, three months, six months and annually thereafter. Patients put on warfarin for anticoagulation after valve replacement with mechanical valve are reviewed more frequently to control the INR. The post-operative hospital stay of patients who underwent thoracic surgery and the protocol for post-operative review are similar to patients who had heart surgery. We have not critically looked at the percentage of patients generally lost to follow up under each category of patients operated. However, patients who underwent heart surgery and had valve replacement with mechanical valve and put on warfarin are seldom lost to follow up.
Challenges in the practice of cardiothoracic surgery in Ghana
The most significant challenge faced by the cardiothoracic surgery program in Ghana is funding of patient care, expanding the existing infrastructure and improving on the standard of care. The cost of heart surgery is beyond the reach of more than 90% of our patients. This has directly and indirectly affected the growth of the cardiothoracic program.
The cost range for open heart surgery is between six thousand US dollars for closure of ventricular septal defect to ten thousand US dollars for double valve replacement surgery. For vascular and thoracic surgical cases, the cost range is between two hundred and fifty US dollars for the construction of Brescia-Cimino arteriovenous fistulae and three thousand US dollars for patients who undergo lung resection. Most patients have to solicit for funds from non-governmental organizations and other philanthropists. This situation delays the institution of prompt treatment and several patients have died while on surgical waiting lists. The Ghana Heart Foundation defrays some of the cost for Ghanaian patients requiring open heart surgery (2). The economic situation is intimately tied to the ability of patients to pay for heart surgery. A stable political environment and economic growth promotes the growth cardiovascular surgery. Ghana has enjoyed a stable political climate and a reasonable economic growth over the years and this has contributed immensely to the sustainability of our program.
Early diagnosis and referral to the only Center in the country located in the southernmost reaches of the country is a challenge for most patients in the northern sectors of the country. The diagnostic capabilities for cardiothoracic pathology outside the main teaching hospitals in the country are limited. There is the need for urgent expansion of the existing infrastructure in other parts of the country. Improving the current infrastructure and manpower will increase geographical access to cardiothoracic services. Financial access to healthcare is currently facilitated mainly by philanthropists and out-of-pocket payments, a situation that ought to change to in order the improve health outcomes. The existing national health insurance scheme currently does not extend to cardiothoracic surgical care because of the cost burden. This is a significant disadvantage for many patients and a pressing challenge to the growth of cardiothoracic surgical practice in Ghana.
Cardiothoracic surgical research
The practice of cardiothoracic surgery in Ghana thrives on emulating worldwide standards. Research provides the data and outcomes that inform practice; the Center has undertaken several research projects culminating in peer reviewed publications in local and international journals.
Sternocleidomastoid myocutaneous esophagoplasty
In 1994, Frimpong-Boateng described four cases of short segment benign strictures involving the cervical esophagus following failed esophageal dilatation (15). The innovative sternocleidomastoid myocutaneous flap was used as a patch to widen the stenotic esophageal segment in these cases. There was no operative death and no leakage of the repair. After 0.5–6.0 years follow up there was no recurrence of the stricture.
CPB in sickle cell anemia without exchange transfusion
Our group is one of the few in the world that has reported successful CPB in sickle cell disease without perioperative exchange transfusion. In a matched pair analysis of patients who underwent hypothermic CPB without exchange transfusion, we demonstrated that perioperative exchange transfusion was not essential for a good outcome in sickle cell patients undergoing CPB (16); a simple transfusion regimen to replace blood loss was found to be safe in sickle cell hemoglobin SS patients. Blood transfusion requirement for hemoglobin SC and hemoglobin AS patients undergoing CPB were similar to those of matched hemoglobin AA controls. Our results also demonstrated that the use of systemic hypothermia during CPB does not increase sickle-cell-related complications and cold crystalloid cardioplegia and topical hypothermia provide safe myocardial protection without the need for more sophisticated measures (16).
This approach to CPB among sickle cell patients is similar in both the Ghanaian and Ivorian experiences (17): both teams emphasize the avoidance of hypoxia, hypovolemia, dehydration, and acidosis in the perioperative period and do not consider perioperative exchange transfusion to be essential. Also, both teams have shown that systemic hypothermia, aortic cross clamping, and cold cardioplegia could be used safely in sickle cell patients undergoing CPB. The difference between the two experiences lie in the number and spectrum of patients reported. The Ivorian experience involved 15 patients (13 Hb AS, 1 Hb SC, and 1 Hb Sβ-thalassemia) while the Ghanaian experience involved 33 patients (21 Hb AS, 7 Hb SS, and 5 Hb SC). Because it involved a broader patient spectrum, the Ghanaian experience could demonstrate important differences in response to CPB between HbSS patients on one hand and HbSC/HbAS patients on the other hand: (I) blood transfusion requirement for HbSS patients undergoing CPB was significantly higher than those of HbSC and Hb AS patients; (II) instead of exchange transfusion, a simple transfusion regimen to replace perioperative blood loss was adequate even in HbSS patients and; (III) blood transfusion requirements for HbSC and HbAS patients undergoing CPB were similar to those of matched HbAA controls.
Trachea stabilization with autologous costal cartilage in acquired tracheomalacia
Post-operative tracheomalacia is a life threatening condition with challenging management. We reported in 2001 the successful management of this condition using autologous costal cartilage to support the tracheal wall (18).
CPB in Jehovah’s witnesses
The need to avoid blood transfusion of heterologous blood in Jehovah’s Witnesses presenting for open heart surgery prompted us to adopt innovative methods based on pre-operative administration of nutritional supplements, oral iron therapy, erythropoietin, antimalarial treatment, and the modification of the extracorporeal bypass circuit to allow successful CPB in these patients (19).
Colopharyngoplasty for intractable pharyngoesophageal strictures
Surgical management of caustic strictures of the upper digestive tract poses difficult challenges because reconstruction above the cricopharyngeal junction interferes with the mechanisms of swallowing and respiration. We recently reported our experience and surgical technique of colopharyngeal reconstruction of the challenging subset of patients with severe diffuse pharyngoesophageal caustic strictures accompanied by upper airway obstruction (20). We showed good results with the establishment of digestive tract continuity using a suprahyoid anastomotic technique. Rehabilitative training for deglutition was a universal requirement in the postoperative period to establish near-normal swallowing.
Colon bypass with a colon-flap augmentation pharyngoesophagoplasty (CFAP)
Extensive caustic stricture of the upper aerodigestive system is a severe injury with limited surgical options. We adopted augmentation of the cicatrized upper aerodigestive tract with colon in selected cases that still has some lumen in the hypopharynx connecting the pharynx. Three selected patients with severe stenotic pharyngo esophageal stricture were operated on using this procedure. Our technique of colon bypass with a CFAP has been described elsewhere (21). Post-operative recovery was uneventful in all cases and all started drinking and eating by the 10th day.
Strictly posterior thoracotomy (SPOT): a minimal-access approach for construction of the MBTS in West Africa
In resource poor settings, the MBTS is often performed for symptomatic relief of Fallot’s tetralogy. We adopted the SPOT, a minimal access technique for the construction of the MBTS (22). The approach represents a safe and cosmetically superior alternative to the standard posterolateral thoracotomy, the scar being imperceptible to the patient. The excellent cosmetic appeal and preservation of body image makes this approach particularly attractive.
Conclusions
Surgery for CHD is the commonest among the major cardiovascular procedures performed in Ghana. Esophageal surgery is constitutes the bulk of thoracic surgery practice. Pacemaker implantation and surgical construction of arteriovenous connections for hemodialysis are among the commonest procedures performed under local anesthesia. Outcomes of surgery for these conditions are comparable to those reported in the international literature. Cardiothoracic surgery practice in Ghana faces the formidable challenges of funding patient care and continued shortage of infrastructure and manpower inputs. In the light of these challenges, the achievements of Ghana’s National Cardiothoracic Center (Figure 7) are remarkable but pale in comparison to the enormity of the healthcare challenges posed by a population of 25 million people served by a single tertiary center for cardiothoracic pathology. This anomaly in healthcare provision shall remain and probably worsen unless the country and its leaders recognize the priority of cardiovascular disease in the emerging landscape of the double burden of disease currently confronting most developing nations.

Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Hoffman JIe. The global burden of congenital heart disease. Cardiovasc J Afr 2013;24:141-5. [Crossref] [PubMed]
- Edwin F, Tettey M, Aniteye E, et al. The development of cardiac surgery in West Africa--the case of Ghana. Pan Afr Med J 2011;9:15. [Crossref] [PubMed]
- Marshall SJ. Developing countries face double burden of disease. Bull World Health Organ 2004;82:556. [PubMed]
- Edwin F, Aniteye E, Tettey MM, et al. Outcome of left heart mechanical valve replacement in West African children--a 15-year retrospective study. J Cardiothorac Surg 2011;6:57. [Crossref] [PubMed]
- Frimpong-Boateng K. Valve replacement surgery at the Korle Bu Teaching Hospital. A review. Ghana Med J 2002;36:145-8.
- Tettey M, Sereboe L, Edwin F. Modified De Vega annuloplasty for functional tricuspid valve regurgitation. Afr Ann Thorac Cardiovasc Surg 2009;4:14-8.
- Tettey M, Sereboe L, Aniteye E, et al. Surgical management of constrictive pericarditis. Ghana Med J 2007;41:190-3. [PubMed]
- Edwin F, Sereboe LA, Tettey MM, et al. Experience from a single centre concerning the surgical spectrum and outcome of adolescents and adults with congenitally malformed hearts in West Africa. Cardiol Young 2010;20:159-64. [Crossref] [PubMed]
- Edwin F, Aniteye E, Tettey M, et al. Permanent complete heart block following surgical correction of congenital heart disease. Ghana Med J 2010;44:109-14. [PubMed]
- Entsua-Mensah K, Aniteye E, Sereboe LA, et al. Junctional ectopic tachycardia following repair of congenital heart defects-experience in multimodal management from a West African Centre. Pan Afr Med J 2012;12:18. [PubMed]
- Edwin F, Entsua-Mensah K, Sereboe L, et al. Conotruncal heart defect repair in Sub-Saharan Africa: Remarkable outcomes despite poor access to treatment. World J Pediatr Congenit Heart Surg 2016;7:592-9. In Press. [Crossref] [PubMed]
- Tamatey MN, Sereboe LA, Tettey MM, et al. Permanent pacemaker implantation in Accra. An 18 year review. Afr Ann Thorac Cardiovasc Surg 2012;7:47-50.
- Tettey M, Edwin F, Aniteye E, et al. Management of intrathoracic oesophageal perforation: analysis of 16 cases. Trop Doct 2011;41:201-3. [Crossref] [PubMed]
- Tettey M, Aniteye E, Sereboe L, et al. Intensive care unit readmission after cardiac and thoracic surgery. Interact Cardiovasc Thorac Surg 2006;1:13-6.
- Frimpong-Boateng K. Sternocleidomastoid myocutaneous esophagoplasty. Eur J Cardiothorac Surg 1994;8:660-2. [Crossref] [PubMed]
- Edwin F, Aniteye E, Tettey M, et al. Hypothermic cardiopulmonary bypass without exchange transfusion in sickle-cell patients: a matched-pair analysis. Interact Cardiovasc Thorac Surg 2014;19:771-6. [Crossref] [PubMed]
- Métras D, Coulibaly AO, Ouattara K, et al. Open-heart surgery in sickle-cell haemoglobinopathies: report of 15 cases. Thorax 1982;37:486-91. [Crossref] [PubMed]
- Frimpong-Boateng K, Aniteye E. Trachea stabilisation with autologous costal cartilage in acquired tracheomalacia: report of two cases. East Afr Med J 2001;78:330-1. [Crossref] [PubMed]
- Frimpong-Boateng K, Aniteye E, Sereboe LA, et al. Cardiopulmonary bypass in Jehovah's Witnesses. West Afr J Med 2003;22:92-4. [PubMed]
- Tettey M, Edwin F, Aniteye E, et al. Colopharyngoplasty for intractable caustic pharyngoesophageal strictures in an indigenous African community--adverse impact of concomitant tracheostomy on outcome. Interact Cardiovasc Thorac Surg 2011;12:213-7. [Crossref] [PubMed]
- Tettey M, Edwin F, Aniteye E. Colon bypass with a colon-flap augmentation pharyngoesophagoplasty. Pan Afr Med J 2015;21:275. [Crossref] [PubMed]
- Edwin F, Gyan B, Adzamli I, et al. Strictly-posterior thoracotomy: a minimal-access approach for construction of the modified Blalock-Taussig shunt in West African children. Pan Afr Med J 2014;17:106. [Crossref] [PubMed]