
IgG4-related disease involving coronary and pulmonary arteries: a case report and literature review
Highlight box
Key findings
• IgG4-related artery disease can involve both coronary and pulmonary arteries.
What is known and what is new?
• IgG4-related artery diseases often involve the abdominal aorta and thoracic aorta, followed by the ascending aorta, coronary artery and renal artery. The pulmonary arteries are less involved, even simultaneous involvement of pulmonary artery and coronary artery is rarer.
• We report a case of a 55-year-old woman with IgG4-related disease simultaneously involving the coronary and pulmonary arteries, and review the domestic literature on IgG4-related artery disease involving coronary/pulmonary arteries, in order to improve people’s understanding of IgG4-related artery disease.
What is the implication, and what should change now?
• This case suggests a possibility of IgG4-related artery disease in patients with clinical symptoms including palpitation, chest discomfort and/or other cardiovascular involvements, which improves people’s diagnostic understanding of IgG4-related artery disease.
Introduction
IgG4-related disease (IgG4-RD) is an inflammation-mediated autoimmune disease accompanied by elevated serum IgG4 levels and is involved in almost every organ system (1). IgG4-RD is characterized by diffuse lymphoplasmacytic infiltrates and the presence of abundant IgG4-positive plasma cells within extensive fibrosis, frequently associated with tumorous swelling and elevated serum IgG4 concentrations (2). IgG4-RD can involve multiple organ systems, involving the arterial system is called IgG4-related artery disease. IgG4-related artery diseases often involve the abdominal aorta and thoracic aorta, followed by the ascending aorta, coronary artery, and renal artery (3). The pulmonary artery, mesenteric artery, and carotid artery are less involved, and even the skin, fundus, and other small arteries can be involved. We report the case of a 55-year-old woman with IgG4-RD simultaneously involving the coronary and pulmonary arteries, which is rarely seen clinically. In addition, we also summarized the relevant literature on IgG4-RD involving coronary or pulmonary artery in China in the past 10 years, and found that compared with the male patient, this case was the first female patient with both coronary artery and pulmonary artery involvement. We present this case in accordance with the CARE reporting checklist (available at https://cdt.amegroups.com/article/view/10.21037/cdt-23-215/rc).
Case presentation
A 55-year-old female patient with nothing unusual in past history came to Shandong Provincial Hospital with “palpitations after activity for one and a half years” on October 15th, 2022. A year and a half prior, the patient had palpitations accompanied by dyspnea and fatigue after activity, and the symptoms were relieved after treatment with nitroglycerin, propranolol and other drugs in a local hospital. Five months prior, the patient’s palpitation symptoms worsened. Her cardiac ultrasound examination showed the following: (I) cardiac insufficiency (left and right coronary artery involvement); (II) involvement of the ascending aorta, pulmonary artery and its branches; (III) secondary pulmonary stenosis; and (IV) mild aortic regurgitation.
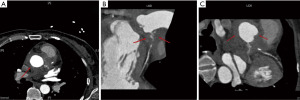
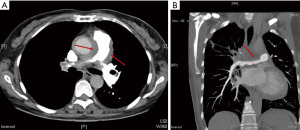
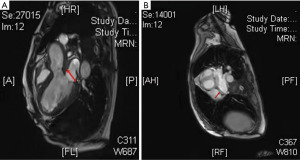
She was admitted to Shandong Provincial Hospital for further diagnosis and treatment. The patient had no fever during the course of the disease. The routine blood test showed white blood cell (WBC) 7.51×109/L, hemoglobin (Hb) 91 g/L, blood platelet (PLT) 390×109/L, eosinophilic granulocyte (EO) 0.01×109/L. The results showed that C-reactive protein (CRP) was 26.16 mg/L (normal range of 0–8 mg/L), erythrocyte sedimentation rate (ESR) was 104 mm/h (normal range of 0–20 mm/h), interleukin 6 (IL-6) was 9.34 pg/mL (normal range of 0–7 pg/mL); BNP was 1,197.00 pg/mL (normal range of <300 pg/mL), IgG4 was 12,800 mg/L (normal range of 30–1,350 mg/L); her antinuclear antibody (ANA) was positive with the titer of 1:100, while anti-dsDNA, anti-SSA, anti-SSB, anti-Sm, anti-U1RNP and ANCA antibodies were negative. Ultrasound of the salivary glands, including the parotid and submandibular glands showed no obvious abnormalities. Ultrasound of superficial lymph nodes did not show any clearly abnormal enlarged lymph nodes. Chest computed tomography (CT) showed the widening of pulmonary artery and thickening of the pulmonary trunk, left and right pulmonary arteries and ascending aorta wall, which indicated that further clinical and aortic computed tomography angiography (CTA) examinations were recommended. There was no abnormality on abdominal CT. Cardiac ultrasound showed the following: (I) left ventricular ejection fraction (LVEF) was 35%; (II) the aortic root and the ascending aorta were surrounded by medium echoic substances with diffuse infiltration, with thickness ranging from 1.30 to 1.56 cm; (III) the opening of the left coronary artery was significantly narrowed, and the left main trunk, anterior descending branch and proximal circumflex branch were wrapped and squeezed, which showed that the echo of the artery wall was enhanced, and the cavity was narrow. The main pulmonary artery and the left and right pulmonary arteries were infiltrated and wrapped by medium/low echoic substances, leading to stenosis of the left and right pulmonary arteries, mainly the right pulmonary artery. Coronary CTA showed mild stenosis of the proximal segment and moderate stenosis of the mid-distal lumen in the right coronary artery, mild stenosis at the beginning of the right posterior descending branch, soft tissue density lesions in the aortic root and left coronary artery, and severe stenosis of multiple lumens in the left main trunk, anterior descending branch and left lateral branch, which are consistent with IgG4-associated arteritis (see Figure 1). Pulmonary artery CTA showed: (I) uneven thickness of the wall and lumen in the pulmonary artery, with the first consideration of IgG4-associated arteritis; and (II) the ascending aorta and aortic arch were altered. Therefore, an aortic CTA examination was performed as a necessity to distinguish vasculitis from intermural hematoma (Figure 2). Contrast-enhanced cardiac magnetic resonance imaging (MRI) revealed that abnormal signals in and around the main and pulmonary artery walls, and a small amount of pericardial effusion (see Figure 3). According to the 2019 ACR/EULAR International Classification Standard for IgG4-RD (4), the patient was diagnosed with possible IgG4-RD and cardiac insufficiency. Then, prednisone at 40 mg/day was given, with myocardial nutrition and metabolic improvement treatment. The clinical symptoms of the patient were relieved without any adverse events. One month later, the level of serum IgG4 was decreased to 5,450 mg/L. On May 12th, 2023, the level of serum IgG4 was decreased to 4,380 mg/L, and echocardiography showed the LVEF was increased to 48%, and the surrounding wrapping of the ascending aorta, the main pulmonary artery and the left and right pulmonary arteries were reduced, with thickness dropping to 1.2 cm. A longer follow-up is planned, which includes the evaluation of clinical symptoms, serum IgG4, cardiac ultrasonography and artery CT.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
IgG4-RD is a set of chronic progressive autoimmune diseases related to IgG4 lymphocytes, characterized by elevated serum IgG4 levels and infiltration of IgG4 plasma cells in affected tissues with an unclear pathogenesis. IgG4-RD can involve many systems, such as the lacrimal glands, salivary glands, pancreas, retroperitoneum, gastrointestinal tract, liver and gallbladder, lung, kidney, central nervous system, and cardiovascular system (5). IgG4 disease involving the arterial system is called IgG4-related artery disease. In 2008, Kasashima et al. (6) regarded IgG4-associated inflammatory abdominal aortic aneurysm as a special manifestation of IgG4-RD involving the large blood vessels. With the increasing clinical studies on IgG4-associated artery diseases in recent years, some scholars believe that IgG4-RD can also be one of the potential causes of major vascular diseases.
IgG4-RDs involving coronary arteries or pulmonary arteries are relatively rare clinically, while simultaneous involvement of both arteries is even rarer, usually with severe clinical symptoms and poor prognosis. The case here we report is the first female patient of IgG4-RD with simultaneous involvement of coronary and pulmonary arteries. The imaging findings of coronary artery and pulmonary artery CTA were consistent with the typical IgG4 imaging features reported previously, including diffuse wall thickening, stenosis and aneurysm (7) (see Figures 1,2). In this case, we found no other involved system and there was no evidence of pathological biopsy, so the diagnosis of this case was not definite. This patient was diagnosed with possible IgG4-RD according to the proposed clinical diagnostic criteria for IgG4-related periarteritis/retroperitoneal lesions (8).
According to literature reports (9), IgG4-related artery diseases often involve the abdominal aorta and thoracic aorta, followed by the ascending aorta, coronary artery and renal artery. The pulmonary artery, mesenteric artery and carotid artery are less involved, and there are even reports of the skin, fundus and other small arteries being involved (10). Although the awareness of IgG4-related artery disease has been increasing in recent years, clinical cases are still rarely reported in China. According to the literature on IgG4-RD involving arteries published in China in the past 10 years, there were a total of 11 cases involving coronary arteries (11-16), mostly of cases in elderly males (8 cases), and the clinical manifestations were mainly chest discomfort, chest tightness and chest pain, while there was only one 51-year-old female case who had involvement of the pulmonary artery (17) (Table 1). No cases involving both the coronary artery and pulmonary artery have been reported in China. In this case, a 55-year-old female patient had both coronary arteries and pulmonary arteries involved, with cardiovascular system involvement as the main manifestation, which is rarer clinically.
Table 1
| Case | Gender | Age of onset, years | Symptoms | IgG4 (g/L) | Affected part of artery | Other affected parts and concomitant disease |
|---|---|---|---|---|---|---|
| 1 | Female | 65 | No symptom | 10.7 | PL of RCA, the proximal and middle segment of LAD, proximal segment of LCX | IgG4-related lymph nodes diseases (neck, mediastinum, hilus pulmonis), moderately differentiated adenocarcinoma of the colon |
| 2–3 | Male | 54 | Paroxysmal chest pain | 17.18 | Middle segment of LAD, proximal segment of RCA | – |
| Female | 58 | Chest distress | 10.32 | Mid-distal segment of the LAD, proximal segment of the RCA | – | |
| 4 | Male | 79 | Occasional chest distress | 17.9 | Proximal and middle segment of the LAD, diagonal branch | Retroperitoneal fibrosis |
| 5 | Male | 58 | Retrosternal discomfort | 8.7 | LAD, LCX, RCA | Autoimmune pancreatitis and cholangitis |
| 6–10 | Male: 4; female: 1 | 62–79 | Chest discomfort in 4 cases, chest distress and chest pain in 3 cases | 21.2–39.2 | LAD of 5 cases, diagonal branch of 1 case, LCX of 2 cases, RCX of 2 cases | 1 case with IgG4-related kidney disease, 3 cases with IgG4-related pancreatitis, and 1 case with IgG4-related orbital inflammation |
| 11 | Male | 62 | Palpitation, chest distress | 9.54 | LM, LAD, LCX, RCA | Mediastinal lymph nodes |
| 12 | Female | 51 | Intermittent chest distress | 8.14 | MPA (right outflow tract to the opening of the RPA) | – |
IgG4-RD, IgG4-related disease; PL, posterior branches of the left ventricle; RCA, right main coronary artery; LAD, left anterior descending branch; LCX, left circumflex branch; LM, left main coronary artery; MPA, main pulmonary artery; RPA, right pulmonary artery.
According to literature reports (18,19), the incidence of IgG4 involving coronary arteries is not high, mostly in elderly male patients with atypical clinical symptoms, such as angina pectoris, myocardial infarction and other characteristic manifestations of myocardial ischemia. However, the symptoms are relatively serious, and can even lead to sudden cardiac death (20), and the prognosis is poor. There are relatively few clinical reports on IgG4 involvement of the pulmonary artery, most of which are manifested as a peri-pulmonary artery mass, pulmonary artery stenosis and/or dilatation, which can lead to pulmonary hypertension in severe cases, including dyspnea after activity, cough, wheezing and other symptoms, and these symptoms need to be differentiated from pulmonary embolism or malignant tumor clinically (21,22).
As we know it, IgG4-related artery disease is often combined with involvement of other organs (23), but there are also a small number of cases that are only limited to arteries. Foreign literature has reported that approximately about 23.9% of patients have isolated coronary arteritis (9). In Table 1, 3/12 patients had only coronary or pulmonary artery involvement.
The histopathologic characteristics of IgG4-related artery disease are chronic inflammatory reactions formed by infiltration of IgG4-positive plasma cells, which may gradually infiltrate the intima inward and the perivascular tissues outward, causing a series of compression symptoms (14). Histopathological biopsy is an important diagnostic basis for IgG4-associated artery disease, but due to the arterial involvement, the difficulty and risk of biopsy are increased. Therefore, pathological tissues obtained during surgical treatment are more clinically common (24,25).
Imaging examinations are important methods for the finding and diagnosis of IgG4-related artery disease, especially CT angiography (26-28), and IgG4-related artery disease is characterized by involvement of single or multiple vessels, segmental thickening around the vessels, and formation of a soft tissue density focus, known as the “Mistletoe sign”. In recent years, it has been reported that positron emission tomography-CT (PET-CT) contributes to identifying affected organs and guiding biopsy, and the images suggest increased fluorodeoxyglucose (FDG) uptake in thickened arterial walls (29,30). In addition, cardiac MRI examination can identify myocardial involvement, fibrosis and other characteristics. The myocardial MRI in this case showed left ventricular enlargement, increased muscle trabeculae, and diffuse reduction of myocardial motion amplitude in all segments of the left ventricle, especially the front wall, suggesting cardiac insufficiency. Therefore, myocardial MRI is also helpful for the differential diagnosis and disease assessment of IgG4-RD.
The diagnosis of IgG4-RD is mainly based on the 2019 ACR/EULAR International Classification Standard. The diagnosis of IgG4-related artery disease requires a combination of clinical findings, imaging, and biopsy results. This patient had coronary artery involvement, and identification of coronary atherosclerosis is necessary: both may show coronary stenosis and elevated inflammatory indicators, but coronary atherosclerosis does not form aneurysms, and IgG4 levels and biopsy results can be used as the main basis for identification. In addition, differential diagnosis of IgG4-RD with giant cell arteritis and Takayasu arteritis is needed: the latter two mainly affect the thoracic aorta and primary branches of the aorta, especially the subclavian artery. Pathologically, IgG4-associated vasculitis is less likely to involve the outer membrane, whereas giant cell arteritis usually involves severe thickening of the outer membrane due to the role of inflammatory mediators.
Glucocorticoids are still preferred for the treatment of IgG4-related arterial diseases, and the therapeutic effects in most cases are significant. After treatment, the serum level of IgG4 can be significantly decreased, and the clinical symptoms can be improved. For some patients with refractory IgG4-RD, rituximab treatment has been reported (31). In addition, surgical treatment, including percutaneous coronary intervention, coronary artery bypass grafting, and resection of inflammatory pseudotumors, can be performed for patients with severe disease who have failed glucocorticoid treatment (7,32).
Conclusions
IgG4-RD can also be one of the potential causes of major vascular diseases. Therefore, patients with clinical cardiovascular symptoms should consider the possibility of IgG4-related artery disease. Early diagnosis and treatment are crucial for IgG4-related artery diseases. Early detection and treatment before organ function is affected as far as much possible can significantly improve the prognosis and quality of life of patients.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://cdt.amegroups.com/article/view/10.21037/cdt-23-215/rc
Peer Review File: Available at https://cdt.amegroups.com/article/view/10.21037/cdt-23-215/prf
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://cdt.amegroups.com/article/view/10.21037/cdt-23-215/coif). The authors have no conflicts of interest to declare.
Ethical Statement:
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Lanzillotta M, Mancuso G, Della-Torre E. Advances in the diagnosis and management of IgG4 related disease. BMJ 2020;369:m1067. [Crossref] [PubMed]
- Kamisawa T, Zen Y, Pillai S, et al. IgG4-related disease. Lancet 2015;385:1460-71. [Crossref] [PubMed]
- Perugino CA, Wallace ZS, Meyersohn N, et al. Large vessel involvement by IgG4-related disease. Medicine (Baltimore) 2016;95:e3344. [Crossref] [PubMed]
- Wallace ZS, Naden RP, Chari S, et al. The 2019 American College of Rheumatology/European League Against Rheumatism Classification Criteria for IgG4-Related Disease. Arthritis Rheumatol 2020;72:7-19. [Crossref] [PubMed]
- Liu H, Yang P, Xiao W, et al. Interpreting of "The 2019 American College of Rheumatology/European League Against Rheumatism classification criteria for IgG4-related disease". Chin J Allergy Clin Immunol 2020;13:447-53.
- Kasashima S, Zen Y, Kawashima A, et al. Inflammatory abdominal aortic aneurysm: Close relationship to IgG4-related periaortitis. Am J Surg Pathol 2008;32:197-204. [Crossref] [PubMed]
- Akiyama M, Kaneko Y, Takeuchi T. Characteristics and prognosis of IgG4-related periaortitis/periarteritis: A systematic literature review. Autoimmun Rev 2019;18:102354. [Crossref] [PubMed]
- Mizushima I, Kasashima S, Fujinaga Y, et al. Clinical and Pathological Characteristics of IgG4-Related Periaortitis/Periarteritis and Retroperitoneal Fibrosis Diagnosed Based on Experts' Diagnosis. Ann Vasc Dis 2019;12:460-72. [Crossref] [PubMed]
- Mizushima I, Kasashima S, Fujinaga Y, et al. IgG4-related periaortitis/periarteritis: An under-recognized condition that is potentially life-threatening. Mod Rheumatol 2019;29:240-50. [Crossref] [PubMed]
- López-Navarro N, Gallego-Dominguez E, Vargas-Nevado A, et al. Granuloma faciale associated with IgG4-related disease. Clin Exp Dermatol 2017;42:799-800. [Crossref] [PubMed]
- Zhao H, Wang J, Xu S, et al. One case of IgG4-related para-coronary aneurysm with 18F-FDG PET/CT imaging. Chin J Nucl Med Mol Imaging 2021;41:557.
- Sun Y, Hou J, Xu K, et al. Coronary artery involvement in IgG4-related disease: two cases report. Chin J Radiol 2020;54:155-6.
- Lv S, Yu X, Han L, et al. One case of coronary artery involvement in IgG4-related disease. Natl Med J China 2019;99:1427-9.
- Yang F, Zhao H. Coronary artery involvement in IgG4-related disease detected by computed tomography: a case report. Chin Circ J 2019;34:402-3.
- Han W, Liu H, He X, et al. Value of MDCT imaging in diagnosis of coronary artery lesions caused by IgG4-related diseases. Chin J Geriatr Heart Brain Vessel Dis 2021;23:452-4.
- Miao L, Dai R. A case of IgG4-related coronary vasculitis. Chin Circ J 2020;35:936-8.
- Zhou H, Zhang W, Huang J. IgG4-related disease involving pulmonary artery by ultrasonography: a case report. Clin J Ultrasonogr 2019;23:545-6.
- Peng L, Zhang P, Li J, et al. IgG4-related aortitis/periaortitis and periarteritis: a distinct spectrum of IgG4-related disease. Arthritis Res Ther 2020;22:103. [Crossref] [PubMed]
- Chen J, Zhang P, Ye H, et al. Clinical features and outcomes of IgG4-related idiopathic orbital inflammatory disease: from a large southern China-based cohort. Eye (Lond) 2021;35:1248-55. [Crossref] [PubMed]
- Patel NR, Anzalone ML, Buja LM, et al. Sudden cardiac death due to coronary artery involvement by IgG4-related disease: a rare, serious complication of a rare disease. Arch Pathol Lab Med 2014;138:833-6. [Crossref] [PubMed]
- Deng H, Zhao S, Yue Y, et al. IgG4-related disease of pulmonary artery causing pulmonary hypertension. Medicine (Baltimore) 2018;97:e10698. [Crossref] [PubMed]
- Katz G, Hedgire SH, Stone JR, et al. IgG4-related disease as a variable-vessel vasculitis: A case series of 13 patients with medium-sized coronary artery involvement. Semin Arthritis Rheum 2023;60:152184. [Crossref] [PubMed]
- Ito T, Fukui S, Kanie T, et al. Immunoglobulin G4-related coronary periarteritis: a systematic literature review with a case series. Clin Rheumatol 2022;41:2281-95. [Crossref] [PubMed]
- Nakamura T, Goryo Y, Isojima T, et al. Immunoglobulin G4-related masses surrounding coronary arteries: a case report. Eur Heart J Case Rep 2021;5:ytab055. [Crossref] [PubMed]
- Ishizaka N. IgG4-related disease underlying the pathogenesis of coronary artery disease. Clin Chim Acta 2013;415:220-5. [Crossref] [PubMed]
- Fathala A. Multimodalities Imaging of Immunoglobulin 4-related Cardiovascular Disorders. Curr Cardiol Rev 2019;15:224-9. [Crossref] [PubMed]
- Rokutanda R, Nishihata Y, Okada M. IgG4-related Pericoronary Arteritis. J Rheumatol 2017;44:1509-10. [Crossref] [PubMed]
- de la Fuente J, Bird J. Coronary Arteritis in IgG4-Related Disease. N Engl J Med 2019;380:2156. [Crossref] [PubMed]
- Fragoulis GE, Evangelatos G, Tektonidou MG. Vasculitis beyond aortitis in IgG4-related disease (IgG4-RD): case report and review of the literature. Clin Rheumatol 2021;40:1167-73. [Crossref] [PubMed]
- Dondi F, Albano D, Bellini P, et al. 18F-fluorodeoxyglucose PET and PET/computed tomography for the evaluation of immunoglobulin G4-related disease: a systematic review. Nucl Med Commun 2022;43:638-45. [Crossref] [PubMed]
- Delgado-García G, Sánchez-Salazar S, Rendón-Ramírez E, et al. Myocardial ischemia as presenting manifestation of IgG4-related disease: a case-based review. Clin Rheumatol 2016;35:2857-64. [Crossref] [PubMed]
- Komiya Y, Soejima M, Tezuka D, et al. Early Detection and Intervention of Coronary Artery Involvement in Immunoglobulin G4-related Disease. Intern Med 2018;57:617-22. [Crossref] [PubMed]


