
Reference intervals for cardiometabolic risk factors in China: a national multicenter cross-sectional study on an adult population sample
Highlight box
Key findings
• Age- and sex-specific reference values for the blood lipids of Chinese healthy adults were established by a nationwide population-based study.
What is known and what is new?
• The reference intervals (RIs) of adult blood lipid parameters currently used in China are not derived from the results of research in local populations and have not been adjusted for age and sex.
• We established accurate RIs of blood lipids for Chinese adults by conducting a nationwide population-based study.
What is the implication, and what should change now?
• More importance should be attached on blood lipids management for the control of cardiovascular disease risk.
Introduction
The examination of homocysteine (HCY), blood lipids, and blood glucose (GluG) levels is crucial for the screening, diagnosis, treatment, prevention, and monitoring of cardiovascular disease (CVD), as this causes significant morbidity and mortality in adults (1-3). Accurate reference intervals (RIs) are required to facilitate the interpretation of individual blood lipid laboratory values and the population distributions of risk markers, including triglycerides (TGs), total cholesterol (TC), low density lipoprotein cholesterol (LDLC), high density lipoprotein cholesterol (HDLC), small dense low density lipoprotein cholesterol (sd-LDLC), apolipoprotein A1 (ApoA1), apolipoprotein B (ApoB), lipoprotein A (LpA), apolipoprotein A2 (ApoA2), HCY, and blood GluG (4,5).
Currently, the RIs used in Chinese laboratories are mainly derived from the National Guide to Clinical Laboratory Procedures (fourth edition), and part of the RIs are derived from the manufacturers’ reagent instructions, which are based on the data from populations in Western countries, and in most cases these values are not universally representative due to population difference (6,7). Although each laboratory is encouraged to establish its own RIs (8), only RIs for serum lipids in Chinese children and adolescents have been established in multicenter studies (9,10), while a large-scale study of blood lipid levels in Chinese healthy adults remains lacking. Five recent studies attempted to establish reference values for blood lipid indicators in Chinese adults (11-15). However, these studies were limited by a small sample size, a narrow scope of field, and the age ranges or sex involved. Moreover, none of these five studies evaluated the levels of apolipoproteins, lipoproteins, sd-LDLC, or HCY, which have been reported to be important predictors for CVD (16-19). Furthermore, the blood lipid levels in healthy individuals can be affected by many factors, among which age and sex are important covariates (20). In one study, variations in the normal range of lipid levels according to age and sexual maturation were reported (21). Differences in lipid levels are linked to sex in Chinese adults (15). However, current reference values for lipid levels used in Chinese adults were not derived from research that considered age and sex differences. Additionally, blood lipids levels vary regionally due to dietary, life style, racial, and geographic conditions. Therefore, it is of great significance to establish age- and sex-specific RIs for the blood lipid levels in adults based on the data from a large multicenter RI study.
In this study, we followed the procedure for establishing RIs recommended by the Clinical and Laboratory Standards Institute (CLSI) document C28-A3 (8). A total of 11,333 adults between 18 and 90 years were recruited in seven representative regions, including Shenyang (northeastern China), Beijing (northern China), Changsha (central China), Ningxia (northwestern China), Chengdu (southwestern China), Hangzhou (southern China), and Nanning (southeastern China), in China. The test results were consistent, as all samples were freshly collected and collectively measured in the same laboratory. Multicenter, age-specific, and sex-specific RIs of blood lipids were established. We present this article in accordance with the STROBE reporting checklist (available at https://cdt.amegroups.com/article/view/10.21037/cdt-23-369/rc).
Methods
Study population
This cross-sectional study was conducted in seven cities (northern China: Beijing, Ningxia, and Shenyang; southern China: Changsha, Chengdu, Hangzhou, and Nanning), representing the four corners and central China. From June 2020 to December 2020, a cohort of 11,333 Chinese Han adults aged 18 to 90 years who met the inclusion criteria were recruited from the following seven hospitals: Beijing Anzhen Hospital, Capital Medical University; the Second Xiangya Hospital of Central South University; the People’s Hospital of Liaoning Province; the General Hospital of Ningxia Medical University; the Hospital of Chengdu University of Traditional Chinese Medicine (TCM); Hangzhou First People’s Hospital; and the First Affiliated Hospital of Guangxi University of Chinese Medicine. The participants who visited the health examination center for a routine health check and resided in the respective city for at least 1 year were enrolled into this study. According to 2016 Chinese guidelines for the management of dyslipidaemia in adults (22), dyslipidemia was defined as one or more following abnormal blood lipid concentrations: TC ≥5.20 mmol/L (200 mg/dL), LDLC ≥3.40 mmol/L (130 mg/dL), HDLC <1.00 mmol/L (40 mg/dL), TG ≥1.70 mmol/L (150 mg/dL). Subjects met the following criteria: GluG <7.0 mmol/L, TC <5.2 mmol/L, TG <1.7 mmol/L, HDLC ≥1.0 mmol/L, and LDLC <3.4 mmol/L were included. Patients who meet at least one of the following criteria were excluded: (I) history of severe internal diseases (i.e., coronary heart disease, renal disease, liver disease, diabetes mellitus, hypertension, or inherited metabolic diseases); (II) any surgery within 6 months; (III) having acute clinical symptoms (e.g., fever and sore throat); (IV) taking medications within the last 2 weeks; (V) being hospitalized within 1 month; (VI) being pregnant/lactating/postpartum within 1 year; (VII) having sample collection after a night shift or violent motion; (VIII) body mass index (BMI) ≥28 or <18.5 kg/m2; or (IX) a history or continued use of alcohol, tobacco, or oral contraceptives. According to the age classification standards of the United Nations World Health Organization, people under 44 years old are young aged, 45–59 years old are middle-aged, 60–74 years are younger elderly, 75–90 years are elderly. In order to maintain a consistent 15-year age group distance, age group 30–44 was identified. Because minors are in the physical development stage, many substances in the body are different from the adult level, so the starting point of the first group is not 15 years old, but 18 years old. Therefore, the data were divided into five age groups (18–29, 30–44, 45–59, 60–74, and 75–90 years). Data were analyzed by subgroup according to sex and age. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of Beijing Anzhen Hospital (No. KS2020005) and informed consent was taken from all the patients. All participating hospitals were informed and agreed with this study.
Sample collection
Blood was collected at cubital venous from participants at each of the included hospitals after they had fasted for at least 8 hours. The participants were required to sit quietly for at least 15 minutes before sampling. Samples were drawn using vacuum tubes, and 30 minutes after sampling, the samples were centrifuged at 2,980 × g for 10 minutes at 20 ℃ and stored at −80 ℃. Following this, serum samples were transported at −20 ℃ to the central laboratory of Beijing Anzhen Hospital, Capital Medical University, for analysis. Serum samples of TG, TC, HDLC, LDLC, ApoA1, ApoB, sd-LDLC, LpA, ApoA2, HCY, and GluG were analyzed on the Mindray fully automatic biochemical analyzer chemistry BS2000 system (Mindray Co., Ltd., Shenzhen, China). In all samples, analyses were performed according to manufacturer’s directions and standard laboratory procedures. The internal controls, a measure used for precision calculating, were performed daily [measured by coefficient of variation (CV)]. The range of CV values for all analytes was 1.53–2.51%. Accuracy was calculated from external quality assessment schemes organized by the Chinese National Center for Clinical Laboratories and are expressed as bias (%). The optimal limits for between- and within-day CVs were set as half of the intraindividual biological CV, which was reported in the Westgard website (https://www.westgard.com/). The tests, methodology and within and between run CV statistics had been listed in Table 1.
Table 1
| Analysis | Methodology | Within run precision (1/4 TEa)† | Within-laboratory precision (1/3 TEa) |
|---|---|---|---|
| TG | Glycerokinase peroxidase-peroxidase method | 3.50% | 4.67% |
| TC | CHOD-POD method | 2.25% | 3.00% |
| LDLC | Direct method | 7.50% | 10.0% |
| HDLC | Direct method | 7.50% | 10.0% |
| sd-LDLC | Peroxidase method | 7.50% | 10.0% |
| ApoA1 | Turbidimetry method | 7.50% | 10.0% |
| ApoB | Turbidimetry method | 7.50% | 10.0% |
| LpA | Latex immunoturbidimetry method | 7.50% | 10.0% |
| HCY | Enzymatic assay method | 5.00% | 6.67% |
| GluG | GOD-POD method | 1.75% | 2.33% |
†, between run precision is the same as within run precision. TEa, allowable total erroer; TG, triglyceride; TC, total cholesterol; CHOD-POD, cholesterol oxidase-peroxidase; LDLC, low density lipoprotein cholesterol; HDLC, high density lipoprotein cholesterol; sd-LDLC, small dense low density lipoprotein cholesterol; ApoA1, apolipoprotein A1; ApoB, apolipoprotein B; LpA, lipoprotein a; HCY, homocysteine; GluG, glucose; GOD-POD, glucose oxidase-peroxidase.
Statistical analysis
Statistical analysis was performed using SPSS 19.0 (IBM Corp., Armonk, NY, USA) software for Microsoft Windows. Scatter and distribution plots were used to visually inspect the data; outliers were then removed using the Tukey test as follows: (year 1977) [<P25 − 1.5 × (P75 − P25), >P75 + 1.5 × (P75 − P25), where P meant percentage] (23). Data from individuals with abnormal results outside the respective RIs were removed. The Box-Cox transformation was used for the transformation of the reference population data to an approximate Gaussian distribution. Subsequently, the partition decisions were statistically evaluated using the test developed by Ichihara and Kawai (24), which uses the nested analysis of variance (ANOVA) to separate the variation and determine if each group is sufficiently different statistically to warrant its own grouping. By use of 3-level nested ANOVOA (3N-ANOVA), the magnitudes of the between-city (btw-city), between-sex (btw-sex), and between-age (btw-age) group components of variation were computed. Each component of variation was derived as a variance and then expressed as the standard deviation (SD) using the square root. The relative magnitude of each SD was expressed as the ratio of SD (SDR) over SDRsex, SDRage, and SDRreg for SD based on sex, age, and region, respectively. An SDR >0.3 was regarded as indicating apparent between-subgroup differences following the International Federation of Clinical Chemistry (IFCC)/Committee on Reference Intervals and Decision Limits (C-RIDL) protocol (25). The method using this cutoff has been verified with other methods (26).
The nonparametric rank-based method was used to calculate the RI for partitions. This method is reasonable for sample sizes of ≥120 participants, especially if the analyst wishes to make no assumptions regarding the underlying distribution of the data. RI were computed using the nonparametric method in both sexes and for each 15-year interval of age. Furthermore, by plotting age on the X-axis and test values on the Y-axis, sex and age profiles of reference values for all test items were drawn as 2-dimensional scattergrams. The limits of the lower and upper RI were set as the 2.5th and 97.5th percentiles of the distribution of values, respectively. For each RI, the 90% confidence intervals (CIs) of the lower limit (LL) and upper limit (UL) were calculated using the bootstrap method. A two-sided P value of <0.05 was considered statistically significant.
Results
After data collection, 11,333 individuals were recruited. After removing the outliers and abnormal values, a total of 8,283 participants were enrolled in the final analysis, with 3,593 (43.4%) men and 4,690 (56.6%) women. As shown in Figure 1, 0 outliers were detected in TG; 66 outliers were detected in TC; 161 outliers were detected in LDLC; 156 outliers were detected in HDLC; 574 outliers were detected in sd-LDLC; 600 outliers were detected in GluG; 59 outliers were detected in ApoA1; 200 outliers were detected in ApoB; 691 outliers were detected in LpA; 948 outliers were detected in LpA II; 505 outliers were detected in HCYII. These outliers were excluded from further analysis. Every 15-year span was classified as a group, and each subcenter collected at least 816 samples. The oldest group was from 75 to 90 years old. The participant inclusion flowchart is shown in Figure 1, and the demographic characteristics of the volunteers from the seven regions of China are shown in Table 2.

Table 2
| Sex | Region | Age group (years) | Total | ||||
|---|---|---|---|---|---|---|---|
| 18–29 | 30–44 | 45–59 | 60–74 | 75–90 | |||
| Male | Beijing | 70 | 84 | 72 | 67 | 87 | 380 |
| Changsha | 117 | 121 | 116 | 123 | 129 | 606 | |
| Shenyang | 125 | 125 | 116 | 116 | 118 | 600 | |
| Ningxia | 115 | 165 | 107 | 147 | 126 | 660 | |
| Chengdu | 122 | 147 | 95 | 73 | 79 | 516 | |
| Hangzhou | 81 | 112 | 93 | 72 | 116 | 474 | |
| Nanning | 145 | 81 | 65 | 46 | 20 | 357 | |
| Total | 775 | 835 | 664 | 644 | 675 | 3,593 | |
| Female | Beijing | 124 | 129 | 95 | 85 | 78 | 511 |
| Changsha | 163 | 158 | 127 | 116 | 79 | 643 | |
| Shenyang | 132 | 318 | 199 | 117 | 123 | 889 | |
| Ningxia | 105 | 272 | 141 | 163 | 141 | 822 | |
| Chengdu | 232 | 323 | 112 | 78 | 53 | 798 | |
| Hangzhou | 98 | 171 | 91 | 84 | 124 | 568 | |
| Nanning | 181 | 134 | 61 | 64 | 19 | 459 | |
| Total | 1,035 | 1,505 | 826 | 707 | 617 | 4,690 | |
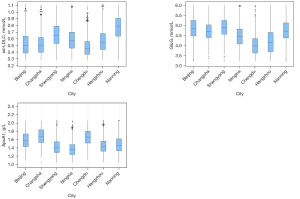
By use of 3N-ANOVA, a primary analysis of sources of possible variation from sex, age, and region was implemented. As judged by SDRsex, apparent sex-related differences (SDRsex >0.3) were observed in two analytes (HDLC and HCY). As judged from the SDRage and SDRreg, we noted apparent age-related differences in two analytes (GluG and HCY) and region-related differences in three analytes (sd-LDLC, GluG, and ApoA1) (Table 3). Figure 2 shows the distributions of the actual test results for three analytes (sd-LDLC, GluG, and ApoA1) grouped by city.
Table 3
| Analysis | Male | Female | Nested ANOVA | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean | SD | n | Mean | SD | SDRsex | SDRage | SDRreg | |||
| TG (mmol/L) | 3,593 | 1.0028 | 0.30418 | 4,690 | 0.9575 | 0.30571 | 0.28 | 0.30 | 0.16 | ||
| TC (mmol/L) | 3,555 | 4.1097 | 0.57184 | 4,662 | 4.2563 | 0.51814 | 0.17 | 0.19 | 0.28 | ||
| LDLC (mmol/L) | 3,504 | 2.3491 | 0.45746 | 4,618 | 2.2822 | 0.43080 | 0.21 | 0.19 | 0.27 | ||
| HDLC (mmol/L) | 3,515 | 1.3361 | 0.20512 | 4,612 | 1.4606 | 0.24628 | 0.40† | 0.09 | 0.17 | ||
| sd-LDLC (mmol/L) | 3,362 | 0.6126 | 0.1923 | 4,347 | 0.5648 | 0.18516 | 0.30 | 0.23 | 0.57† | ||
| GluG (mmol/L) | 3,325 | 4.6103 | 0.62123 | 4,358 | 4.5390 | 0.60464 | 0.13 | 0.39† | 0.72† | ||
| ApoA1 (nmol/L) | 3,613 | 1.4686 | 0.21090 | 4,610 | 1.5518 | 0.22530 | 0.27 | 0.21 | 0.54† | ||
| ApoB (nmol/L) | 3,491 | 0.8067 | 0.15375 | 4,592 | 0.7846 | 0.14639 | 0.18 | 0.21 | 0.18 | ||
| LpA (nmol/L) | 3,271 | 148.9488 | 87.18230 | 4,312 | 156.6862 | 93.73499 | 0.07 | 0.11 | 0.16 | ||
| LpAII (nmol/L) | 3,137 | 18.2128 | 18.16229 | 4,147 | 20.5679 | 20.80129 | 0.08 | 0.11 | 0.08 | ||
| HCYII (μmol/L) | 3,283 | 14.320 | 4.445 | 4,495 | 10.649 | 3.181 | 0.56† | 0.33† | 0.21 | ||
The relative magnitude of each SD was expressed as the SDR over SDRsex, SDRage, and SDRreg for SD based on sex, age, and region, respectively. An SDR >0.3 was regarded as a guide to consider partitioning reference values by the factor. †, indicates those analytes which were judged as requiring separation. ANOVA, analysis of variance; SD, standard deviation; SDR, ratio of SD; TG, triglyceride; TC, total cholesterol; LDLC, low density lipoprotein cholesterol; HDLC, high density lipoprotein cholesterol; sd-LDLC, small dense low density lipoprotein cholesterol; GluG, glucose; ApoA1, apolipoprotein A1; ApoB, apolipoprotein B; LpA, lipoprotein a; HCY, homocysteine.
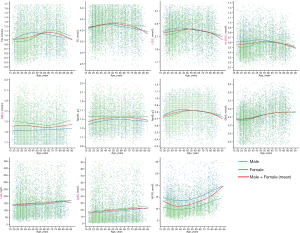
As shown in Figure 3, 2D scattergrams with a trend line of age-related changes of analytes are shown for the visualization of actual differences among the indicators. TG, TC, LDLC, sd-LDLC, ApoB, and GluG have a cross-point between the trend line of females and males. The sharp increase of TG in males appears at the age of 18–44 years, while it occurs in females at the age of 45–65 years. Among adults, TG levels are lower in females than in males (P<0.05), increase with age through age 55 years (to a greater degree in women than in men), and decline in females at 70 years of age (more so in women than in men). TC shows a positive age trend up to the age of 45 years, but no sex-related changes. However, in participants >45 years, the trend line of TC in females is clearly higher than that in males and shows a negative age trend as age increases from this point. The trend lines of LDLC, sd-LDLC, and ApoB in females are clearly lower than those in males up to the age of 45 years, with almost no sex-related changes being apparent as age increases from this point. The trend lines of HDLC and ApoA1 in females are significantly higher than those in males in all age subgroups, whereas HCY significantly higher in males than in females. The trend line of HDLC is relatively stable up to 45 years and increases with age after this point. The concentrations of ApoB gradually increase before 50 years and then decrease. GluG, increases gradually with aging, and small sex-related changes can be observed. For HDLC, ApoA1, LpA, and ApoA2, linear but small age-related changes are discernible. The percentile curves are presented in Figure 4.
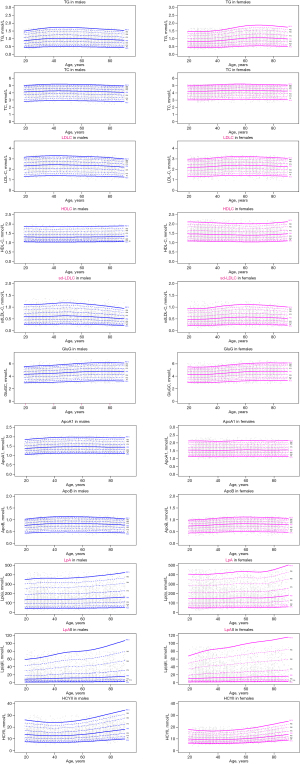
Hospitals participating in the study were regrouped into two geographical regions: southern China and northern China according to their geographical and administrative location. RIs of each analyte derived by nonparametric method with partitioning according to southern China or northern China region, sex (male and female), and age (18–29, 30–44, 45–59, 60–74, and 75–90 years) are summarized in Tables 4,5, respectively. Table 6 details the final results of our study. RIs of lipids, apolipoproteins, lipoproteins, HCY, and GluG were divided by age, sex, and regions.
Table 4
| Analyte | Age (years) | Southern China (Changsha, Chengdu, Hangzhou, and Nanning) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male + female | Male | Female | |||||||||||||
| n | LL (90% CI) | ME (90% CI) | UL (90% CI) | n | LL (90% CI) | ME (90% CI) | UL (90% CI) | n | LL (90% CI) | ME (90% CI) | UL (90% CI) | ||||
| TG (mmol/L) | 18-29 | 1,139 | 0.45 (0.42–0.46) | 0.90 (0.88–0.91) | 1.57 (1.52–1.61) | 465 | 0.49 (0.46–0.61) | 0.97 (0.95–1.00) | 1.61 (1.57–1.64) | 674 | 0.42 (0.41–0.45) | 0.85 (0.83–0.86) | 1.50 (1.47–1.54) | ||
| 30–44 | 1,247 | 0.48 (0.47–0.50) | 0.94 (0.93–0.96) | 1.59 (1.56–1.61) | 461 | 0.51 (0.51–0.58) | 1.05 (1.03–1.08) | 1.62 (1.59–1.65) | 786 | 0.47 (0.45–0.49) | 0.88 (0.86–0.90) | 1.55 (1.50–1.58) | |||
| 45–59 | 760 | 0.52 (0.49–0.54) | 1.03 (1.01–1.04) | 1.62 (1.60–1.64) | 369 | 0.51 (0.47–0.56) | 1.06 (1.03–1.08) | 1.63 (0.61–1.66) | 391 | 0.52 (0.49–0.55) | 1.00 (0.97–1.03) | 1.60 (1.58–1.63) | |||
| 60–74 | 656 | 0.55 (0.53–0.59) | 1.06 (1.04–1.08) | 1.63 (1.61–1.65) | 314 | 0.54 (0.48–0.57) | 1.03 (1.00–1.05) | 1.59 (1.55–1.63) | 342 | 0.61 (00.53–0.649 | 1.09 (1.07–1.12) | 1.65 (1.62–1.66) | |||
| 75–90 | 619 | 0.53 (0.49–0.54) | 1.03 (1.01–1.05) | 1.61 (0.59–1.64) | 344 | 0.52 (0.49–0.54) | 0.98 (0.96–1.01) | 1.62 (1.55–1.66) | 275 | 0.54 (0.49–0.61) | 1.10 (1.07–1.13) | 1.61 (1.60–1.64) | |||
| TC (mmol/L) | 18–29 | 1,137 | 3.11 (3.07–3.17) | 4.22 (4.20–4.25) | 5.11 (5.09–5.13) | 465 | 3.04 (2.98–3.18) | 4.20 (4.16–4.25) | 5.10 (5.06–5.13) | 672 | 3.15 (3.08–3.23) | 4.23 (4.20–4.25) | 5.12 (5.09–5.14) | ||
| 30–44 | 1,246 | 3.21 (3.12–3.28) | 4.31 (4.28–4.33) | 5.10 (5.08–5.13) | 461 | 3.27 (3.14–3.42) | 4.35 (4.31–4.39) | 5.08 (5.05–5.13) | 785 | 3.18 (3.06–3.28) | 4.28 (4.25–4.31) | 5.10 (5.09–5.13) | |||
| 45–59 | 760 | 3.29 (3.18–3.39) | 4.39 (4.37–4.43) | 5.13 (5.12–5.14) | 369 | 3.19 (3.03–3.30) | 4.32 (4.27–4.36) | 5.12 (5.10–5.13) | 391 | 3.45 (3.37–3.57) | 4.47 (4.43–4.51) | 5.14 (5.13–5.16) | |||
| 60–74 | 656 | 3.17 (3.07–3.24) | 4.35 (4.32–4.38) | 5.12 (5.11–5.13) | 314 | 3.01 (2.91–3.20) | 4.29 (4.23–4.34) | 5.12 (5.08–5.15) | 342 | 3.25 (3.19–3.36) | 4.41 (4.36–4.45) | 5.12 (5.10–5.14) | |||
| 75–90 | 618 | 3.05 (2.95–3.14) | 4.24 (4.10–4.27) | 5.11 (5.06–5.13) | 344 | 2.95 (2.80–3.08) | 4.16 (4.11–4.21) | 5.05 (5.00–5.13) | 274 | 3.25 (3.13–3.34) | 4.34 (4.29–4.40) | 5.11 (5.08–5.16) | |||
| LDLC (mmol/L) | 18–29 | 1,139 | 1.35 (1.27–1.42) | 2.24 (2.21–2.26) | 3.13 (3.07–3.16) | 465 | 1.43 (1.27–1.500 | 2.35 (2.31–2.38) | 3.19 (3.14–3.25) | 674 | 1.32 (1.20–1.38) | 2.16 (2.13–2.19) | 3.03 (2.94–3.09) | ||
| 30–44 | 1,247 | 1.41 (1.37–1.45) | 2.29 (2.27–2.31) | 3.11 (3.05–3.13) | 461 | 1.54 (1.46–1.61) | 2.44 (2.40–2.47) | 3.20 (3.10–3.26) | 1505 | 1.39 (1.37–1.44) | 2.25 (2.23–2.27) | 3.03 (3.01–3.08) | |||
| 45–59 | 786 | 1.38 (1.33–1.43) | 2.21 (2.18–2.23) | 3.04 (2.95–3.09) | 369 | 1.38 (1.23–1.55) | 2.39 (2.35–2.43) | 3.19 (3.14–3.24) | 391 | 1.51 (1.39–1.58) | 2.36 (2.33–2.40) | 3.16 (3.12–3.19) | |||
| 60–74 | 653 | 1.39 (1.36–1.49) | 2.35 (2.32–2.38) | 3.19 (3.14–3.24) | 312 | 1.38 (1.34–1.46) | 2.35 (2.31–2.40) | 3.19 (3.13–3.25) | 341 | 1.46 (1.35–1.58) | 2.35 (2.31–2.39) | 3.18 (3.07–3.25) | |||
| 75–90 | 617 | 1.25 (1.15–1.35) | 2.26 (2.22–2.29) | 3.09 (3.05–3.16) | 342 | 1.21 (1.13–1.33) | 2.24 (2.20–2.28) | 3.07 (3.03.3.24) | 275 | 1.35 (1.14–1.41) | 2.28 (2.23–2.32) | 3.10 (3.06–3.150 | |||
| HDLC (mmol/L) | 18–29 | 1,115 | 1.08 (1.07–1.09) | 1.44 (1.43–1.45) | 1.97 (1.94–2.02) | 454 | 1.07 (1.06–1.08) | 1.34 (1.33–1.35) | 1.82 (1.77–1.88) | 661 | 1.10 (1.07–1.12) | 1.51 (1.50–1.53) | 2.03 (1.98–2.08) | ||
| 30–44 | 1,224 | 1.07 (1.06–1.07) | 1.44 (1.43–1.45) | 2.06 (2.00–2.09) | 448 | 1.06 (1.05–1.07) | 1.33 (1.32–1.35) | 1.78 (1.73–1.86) | 776 | 1.07 (1.06–1.09) | 1.50 (1.49–1.52) | 2.10 (2.08–2.13) | |||
| 45–59 | 774 | 1.07 (1.06–1.08) | 1.41 (1.40–1.43) | 1.95 (1.91–2.01) | 357 | 1.06 (1.05–1.07) | 1.34 (1.33–1.36) | 1.82 (1.79–1.88) | 384 | 1.08 (1.07–1.11) | 1.48 (1.46–1.50) | 2.04 (1.99–2.12) | |||
| 60–74 | 646 | 1.06 (1.05–1.08) | 1.42 (1.40–1.43) | 1.92 (1.88–1.99) | 307 | 1.05 (1.05–1.07) | 1.37 (1.35–1.39) | 1.87 (1.84–1.90) | 339 | 1.08 (1.06–1.100 | 1.45 (1.43–1.47) | 2.01 (1.90–2.04) | |||
| 75–90 | 606 | 1.06 (1.06–1.08) | 1.44 (1.43–1.460 | 2.00 (1.97–2.050 | 334 | 1.05 (1.05–1.07) | 1.39 (1.37–1.41) | 1.83 (1.78–1.85) | 272 | 1.08 (1.06–1.10) | 1.51 (1.48–1.53) | 2.07 (2.02–2.15) | |||
| sd-LDLC (mmol/L) | 18–29 | 1,129 | 0.23 (0.21–0.24) | 0.55 (0.53–0.56) | 1.07 (1.05–1.11) | 462 | 0.26 (0.23–0.29) | 0.61 (0.59–0.63) | 1.18 (1.07–1.24) | 667 | 0.22 (0.20–0.23) | 0.50 (0.49–0.51) | 1.01 (0.96–1.06) | ||
| 30–44 | 1,227 | 0.22 (0.21–0.24) | 0.54 (0.53–0.55) | 1.06 (1.04–1.09) | 457 | 0.26 (0.25–0.29) | 0.61 (0.60–0.63) | 1.13 (1.06–1.23) | 770 | 0.21 (0.19–0.22) | 0.50 (0.49–0.52) | 1.03 (0.97–1.07) | |||
| 45–59 | 750 | 0.26 (0.23–0.28) | 0.59 (0.57–0.60) | 1.12 (1.07–1.19) | 366 | 0.26 (0.23–0.30) | 0.63 (0.61–0.65) | 1.19 (1.11–1.28) | 384 | 0.25 (0.21–0.27) | 0.54 (0.53–0.56) | 1.04 (1.01–1.09) | |||
| 60–74 | 650 | 0.23 (0.22–0.25) | 0.59 (0.57–0.60) | 1.09 (1.04–1.14) | 311 | 0.23 (0.20–0.28) | 0.60 (0.58–0.62) | 1.11 (1.01–1.23) | 339 | 0.23 (0.22–0.25) | 0.58 (0.56–0.60) | 1.09 (1.03–1.13) | |||
| 75–90 | 616 | 0.24 (0.21–0.26) | 0.56 (0.55–0.57) | 1.02 (0.96–1.05) | 343 | 0.23 (0.18–0.25) | 0.56 (0.54–0.58) | 1.02 (0.96–1.09) | 373 | 0.25 (0.22–0.30) | 0.56 (0.55–0.58) | 1.00 (0.92–1.03) | |||
| GluG (mmol/L) | 18–29 | 1,137 | 2.91 (2.89–2.94) | 4.18 (4.15–4.21) | 5.42 (5.35–5.51) | 464 | 2.92 (2.87–2.98) | 4.23 (4.18–4.28) | 5.46 (5.32–5.53) | 673 | 2.91 (2.88–2.94) | 4.14 (4.09–4.18) | 5.41 (5.27–5.52) | ||
| 30–44 | 1,246 | 2.95 (2.90–3.00) | 4.14 (4.11–4.17) | 5.61 (5.44–5.72) | 461 | 2.89 (2.97–2.96) | 4.19 (4.13–4.25) | 5.77 (5.56–5.89) | 785 | 2.99 (2.94–3.02) | 4.11 (4.07–4.15) | 5.43 (5.30–5.65) | |||
| 45–59 | 756 | 2.96 (2.91–3.01) | 4.37 (4.33–4.41) | 5.84 (5.73–5.96) | 368 | 2.95 (2.88–3.01) | 4.39 (4.33–4.46) | 5.87 (5.73–6.05) | 388 | 2.96 (2.89–3.06) | 4.35 (4.29–4.40) | 5.80 (5.67–6.07) | |||
| 60–74 | 649 | 3.01 (2.95–3.05) | 4.57 (4.52–4.62) | 6.04 (5.89–6.16) | 310 | 3.03 (2.97–3.18) | 4.59 (4.52–4.66) | 5.95 (5.81–6.24) | 339 | 2.96 (2.88–3.05) | 4.56 (4.48–4.63) | 6.10 (5.9–6.18) | |||
| 75–90 | 617 | 3.02 (2.97–3.10) | 4.66 (4.61–4.71) | 6.03 (5.91–6.16) | 342 | 2.99 (2.92–3.11) | 4.64 (4.58–4.71) | 6.02 (5.88–6.16) | 275 | 3.05 (2.96–3.18) | 4.68 (1.60–4.75) | 6.08 (2.89–6.26) | |||
| ApoA1 (g/L) | 18–29 | 1,135 | 1.15 (1.14–1.18) | 1.56 (1.54–1.57) | 2.09 (2.05–2.14) | 463 | 1.15 (1.14–1.72) | 1.46 (1.44–1.47) | 1.91 (1.83–1.95) | 672 | 1.16 (1.13–1.19) | 1.62 (1.61–1.64) | 2.16 (2.09–2.21) | ||
| 30–44 | 1,238 | 1.20 (1.18–1.21) | 1.60 (1.59–1.61) | 2.11 (2.07–2.16) | 460 | 1.18 (1.17–1.20) | 1.53 (1.51–1.55) | 1.96 (1.91–1.99) | 778 | 1.21 (1.18–1.24) | 1.65 (1.63–1.66) | 2.18 (2.13–2.21) | |||
| 45–59 | 737 | 1.19 (1.17–1.21) | 1.62 (1.61–1.64) | 2.14 (2.10–2.18) | 357 | 1.17 (1.16–1.20) | 1.56 (1.54–1.58) | 2.03 (1.98–2.05) | 380 | 1.23 (1.17–1.28) | 1.68 (1.66–1.70) | 2.19 (2.16–2.21) | |||
| 60–74 | 639 | 1.22 (1.19–1.25) | 1.65 (1.63–1.66) | 2.14 (2.11–2.17) | 306 | 1.19 (1.17–1.24) | 1.60 (1.58–1.62) | 2.02 (2.00–2.04) | 333 | 1.24 (1.21–1.28) | 1.69 (1.67–1.71) | 2.18 (2.16–2.25) | |||
| 75–90 | 613 | 1.19 (1.18–1.22) | 1.59 (1.57–1.60) | 2.07 (2.06–2.12) | 339 | 1.18 (1.14–1.20) | 1.52 (1.50–1.54) | 2.04 (1.98–2.05) | 374 | 1.23 (1.22–1.29) | 1.67 (1.65–1.69) | 2.17 (2.09–2.21) | |||
| ApoB (g/L) | 18–29 | 1,136 | 0.46 (0.43–0.48) | 0.75 (0.75–0.76) | 1.03 (1.01–1.05) | 463 | 0.48 (0.45–0.49) | 0.78 (0.77–0.79) | 1.05 (1.04–1.07) | 673 | 0.45 (0.41–0.47) | 0.74 (1.73–0.75) | 1.00 (0.98–1.01) | ||
| 30–44 | 1,245 | 0.49 (0.48–0.51) | 0.79 (0.78–0.80) | 1.06 (1.04–1.08) | 461 | 0.53 (0.48–0.56) | 0.83 (0.82–0.85) | 1.10 (1.07–1.11) | 784 | 0.48 (0.48–0.50) | 0.77 (0.76–0.78) | 1.02 (1.02–1.06) | |||
| 45–59 | 758 | 0.52 (0.47–0.55) | 0.83 (0.82–0.84) | 1.10 (1.08–1.12) | 368 | 0.50 (0.42–0.56) | 0.84 (0.82–0.85) | 1.11 (1.10–1.12) | 390 | 0.53 (0.47–0.56) | 0.83 (0.81–0.84) | 1.09 (1.16–1.12) | |||
| 60–74 | 654 | 0.50 (0.47–0.53) | 0.83 (0.82–0.84) | 1.09 (1.07–1.10) | 313 | 0.49 (0.40–0.52) | 0.84 (0.82–0.85) | 1.10 (1.07–1.17) | 341 | 0.52 (0.45–0.56) | 0.83 (0.82–0.84) | 1.07 (1.06–1.09) | |||
| 75–90 | 617 | 0.44 (0.43–0.48) | 0.80 (0.79–0.81) | 1.09 (1.07–1.10) | 342 | 0.44 (0.42–0.47) | 0.79 (0.77–0.81) | 1.09 (1.06–1.14) | 275 | 0.46 (0.41–0.52) | 0.81 (0.79–0.82) | 1.09 (1.07–1.11) | |||
| LpA (mg/L) | 18–29 | 1,061 | 33.48 (30.58–38.35) | 145.44 (140.52–150.02) | 408.45 397.36–418.02) | 433 | 32.68 (27.93–38.04) | 141.28 (133.71–148.53) | 402.81 (375.99–414.06) | 673 | 36.24 (28.91–42.43) | 148.32 (141.94–155.15) | 417.37 (398.62–423.82) | ||
| 30–44 | 1,169 | 38.57 (34.15–42.41) | 149.56 (145.26–154.13) | 392.64 (376.78–402.35) | 435 | 31.62 (28.09–37.10) | 138.48 (130.91–145.70) | 370.59 (332.08–388.58) | 734 | 42.82 (40.71–46.43) | 156.13 (149.86–162.44) | 401.88 (385.96–413.73) | |||
| 45–59 | 711 | 39.20 (36.43–43.19) | 148.72 (143.55–153.93) | 377.93 (359.35–399.64) | 336 | 37.95 (30.71–42.48) | 143.78 (136.13–151.29) | 382.00 (345.78–388.54) | 375 | 41.77 (35.25–44.54) | 153.15 (145.74–160.95) | 372.20 (352.20–433.65) | |||
| 60–74 | 583 | 38.67 (32.89–43.91) | 157.43 (151.76–163.25) | 373.62 (357.16–396.36) | 284 | 33.78 (30.75–44.11) | 149.42 (140.86–157.58) | 346.95 (324.32–373.58) | 299 | 40.59 (36.03–52.57) | 165.03 (156.72–173.81) | 391.92 (367.62–414.02) | |||
| 75–90 | 550 | 48.35 (44.01–52.49) | 172.90 (165.52–179.84) | 422.41 (414.49–431.07) | 309 | 48.20 (42.74–53.17) | 164.61 (156.00–173.14) | 414.65 (380.98–418.73) | 241 | 47.58 (41.38–60.66) | 183.52 (172.00–195.21) | 442.14 (420.50–453.59) | |||
| LpAII (nmol/L) | 18–29 | 1,020 | 1.48 (1.36–1.72) | 16.20 (15.23–17.12) | 72.83 (68.90–77.30) | 414 | 1.44 (1.21–1.68) | 14.64 (13.27–15.88) | 68.86 (60.47–70.95) | 606 | 1.50 (1.32–1.92) | 17.26 (16.08–18.61) | 78.84 (72.72–82.94) | ||
| 30–44 | 1,133 | 1.80 (1.67–2.08) | 18.30 (17.38–19.28) | 74.69 (70.36–77.38) | 424 | 1.37 (1.07–1.87) | 16.24 (14.82–17.70) | 70.03 (61.67–75.67) | 709 | 2.11 (1.77–2.36) | 19.53 (18.27–20.81) | 77.01 (71.84–84.12) | |||
| 45–59 | 701 | 1.91 (1.65–2.13) | 18.14 (17.19–19.19) | 70.29 (68.36–75.91) | 333 | 1.65 (1.02–2.08) | 17.03 (15.54–18.55) | 69.20 (62.99–72.15) | 368 | 2.09 (1.77–2.43) | 19.15 (17.56–20.67) | 76.05 (69.27–85.26) | |||
| 60–74 | 585 | 2.32 (2.08–2.60) | 19.74 (18.43–21.14) | 75.97 (71.01–80.82) | 284 | 2.09 (1.73–2.53) | 18.56 (16.83–20.33) | 72.81 (66.37–75.79) | 301 | 2.57 (2.28–3.04) | 20.84 (19.00–22.75) | 81.84 (70.47–86.92) | |||
| 75–90 | 521 | 2.60 (2.21–2.86) | 22.42 (20.83–23.89) | 79.47 (75.94–82.43) | 293 | 2.63 (1.74–2.93) | 20.85 (19.11–22.82) | 73.53 (66.93–77.62) | 228 | 2.54 (2.21–3.11) | 24.43 (22.05–26.91) | 86.20 (79.81–88.21) | |||
| HCYII (μmol/L) | 18–29 | 1,081 | 6.35 (6.09–6.57) | 11.61 (11.40–11.83) | 22.48 (21.22–23.42) | 434 | 7.28 (6.90–7.72) | 13.94 (13.55–14.27) | 27.49 (24.39–28.23) | 647 | 6.08 (5.71–6.42) | 10.05 (9.86–10.24) | 17.05 (16.65–18.22) | ||
| 30–44 | 1,217 | 6.16 (5.91–6.30) | 10.82 (10.63–11.01) | 20.71 (19.93–21.89) | 442 | 6.70 (6.02–7.91) | 13.20 (12.87–13.56) | 25.08 (22.78–26.55) | 775 | 5.95 (5.79–6.25) | 9.47 (9.31–9.62) | 17.32 (15.90–17.53) | |||
| 45–59 | 752 | 6.75 (6.34–7.02) | 11.68 (11.47–11.93) | 21.66 (20.13–23.41) | 359 | 7.63 (6.98–8.01) | 13.43 (13.06–13.79) | 24.50 (23.18–26.02) | 383 | 6.31 (5.90–6.77) | 10.04 (9.84–10.25) | 16.20 (15.41–16.88) | |||
| 60–74 | 639 | 7.28 (7.17–7.49) | 12.64 (12.36–12.90) | 22.67 (21.42–23.05) | 308 | 8.10 (7.80–9.05) | 14.31 (13.90–14.70) | 24.15 (22.92–26.30) | 331 | 7.06 (6.40–7.23) | 11.08 (10.80–11.37) | 18.57 (17.16–19.06) | |||
| 75–90 | 568 | 8.33 (7.99–8.84) | 15.81 (15.47–16.16) | 27.24 (25.87–28.52) | 335 | 8.66 (7.50–9.40) | 17.64 (17.15–18.23) | 28.99 (27.25–29.72) | 233 | 8.05 (7.71–8.81) | 13.18 (12.84–13.51) | 19.41 (18.68–20.20) | |||
LL, lower limit, CI, confidence interval; ME, median; UL, upper limit; TG, triglyceride; TC, total cholesterol; LDLC, low density lipoprotein cholesterol; HDLC, high density lipoprotein cholesterol; sd-LDLC, small dense low density lipoprotein cholesterol; GluG, glucose; ApoA1, apolipoprotein A1; ApoB, apolipoprotein B; LpA, lipoprotein a; HCY, homocysteine.
Table 5
| Analyte | Age (years) | Northern China (Beijing, Shenyang, and Ningxia) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male + female | Male | Female | |||||||||||||
| n | LL (90% CI) | ME (90% CI) | UL (90% CI) | n | LL (90% CI) | ME (90% CI) | UL (90% CI) | n | LL (90% CI) | ME (90% CI) | UL (90% CI) | ||||
| TG (mmol/L) | 18–29 | 671 | 0.43 (0.41–0.45) | 0.92 (0.90–0.94) | 1.59 (1.54–1.62) | 310 | 0.42 (0.39–0.45) | 0.93 (0.90–0.96) | 1.59 (1.49–1.62) | 361 | 0.43 (0.39–0.46) | 0.92 (0.89–0.94) | 1.61 (1.54–1.66) | ||
| 30–44 | 1,093 | 0.44 (0.42–0.45) | 0.93 (0.91–0.94) | 1.58 (0.54–1.61) | 374 | 0.46 (0.44–0.48) | 1.01 (0.98–1.03) | 1.61(1.56–1.65) | 719 | 0.42 (0.39–0.44) | 0.88 (0.87–0.90) | 1.54 (1.49–1.60) | |||
| 45–59 | 730 | 0.47 (0.45–0.51) | 1.00 (0.98–1.02) | 1.62 (1.59–1.65) | 295 | 0.47 (0.43–0.51) | 1.02 (1.00–1.05) | 1.61 (1.57–1.65) | 435 | 0.48 (0.45–0.51) | 0.99 (0.96–1.01) | 1.63 (1.57–1.65) | |||
| 60–74 | 695 | 0.53 (0.50–0.54) | 1.06 (1.05–1.08) | 1.63 (1.60–1.65) | 330 | 0.49 (0.46–0.52) | 1.01 (0.98–1.04) | 1.62(1.58–1.64) | 365 | 0.55 (0.53–0.60) | 1.12 (1.09–1.15) | 1.64 (1.59–1.68) | |||
| 75–90 | 673 | 0.51 (0.48–0.54) | 1.00 (0.98–1.02) | 1.60 (1.58–1.64) | 331 | 0.50 (0.46–0.53) | 0.95 (0.92–0.97) | 1.59 (1.51–1.65) | 342 | 0.55 (0.45–0.59) | 1.05 (1.02–1.07) | 1.62 (1.58–1.67) | |||
| TC (mmol/L) | 18–29 | 670 | 3.06 (2.97–3.12) | 4.10 (4.07–4.13) | 5.03 (4.98–5.05) | 310 | 3.01 (2.84–3.15) | 4.09 (4.04–4.14) | 5.04 (4.99–5.07) | 360 | 3.07 (2.95–3.18) | 4.11 (4.07–4.15) | 5.00 (4.94–5.09) | ||
| 30–44 | 1,093 | 3.11 (3.06–3.15) | 4.17 (4.14–4.19) | 5.05 (5.00–5.08) | 374 | 3.10 (2.89–3.17) | 4.18 (4.13–4.22) | 5.05 (4.99–5.07) | 719 | 3.13 (3.07–3.17) | 4.16 (4.13–4.19) | 5.07 (4.98–5.12) | |||
| 45–59 | 730 | 3.00 (2.93–3.07) | 4.21 (4.18–4.25) | 5.06 (5.03–5.09) | 295 | 2.92 (2.72–3.03) | 4.11 (4.05–4.17) | 5.07 (5.01–5.10) | 435 | 3.11 (2.95–3.30) | 4.28 (4.24–4.32) | 5.06 (5.03–5.10) | |||
| 60–74 | 693 | 2.90 (2.83–2.97) | 4.09 (4.06–4.13) | 5.03 (4.99–5.07) | 329 | 2.83 (2.62–2.94) | 4.00 (3.94–4.06) | 5.04 (4.93–5.11) | 364 | 2.97 (2.87–3.13) | 4.17 (4.13–4.22) | 5.05 (4.99–5.07) | |||
| 75–90 | 662 | 2.76 (2.70–2.86) | 4.04 (4.00–4.07) | 5.00 (4.97–5.05) | 326 | 2.67 (2.56–2.85) | 3.95 (3.90–4.01) | 4.96 (4.90–5.01) | 336 | 2.84 (2.72–2.94) | 4.12 (4.06–4.17) | 5.04 (4.99–5.07) | |||
| LDLC (mmol/L) | 18–29 | 671 | 1.43 (1.39–1.48) | 2.30 (2.27–2.33) | 3.19 (3.11–3.24) | 310 | 1.49 (1.43–1.57) | 2.38 (2.34–2.43) | 3.27 (3.18–3.32) | 361 | 1.40 (1.19–1.44) | 2.23 (2.19–2.27) | 3.04 (2.96–3.12) | ||
| 30–44 | 1,093 | 1.46 (1.39–1.50) | 2.34 (2.32–2.36) | 3.11 (3.08–3.18) | 374 | 1.47 (1.35–1.62) | 2.43 (2.39–2.47) | 3.25 (3.18–3.27) | 719 | 1.45 (1.38–1.50) | 2.29 (2.27–2.32) | 3.03 (3.01–3.09) | |||
| 45–59 | 729 | 1.47 (1.41–1.54) | 2.39 (2.37–2.42) | 3.19 (3.14–3.21) | 294 | 1.36 (1.22–1.53) | 2.38 (2.33–2.43) | 3.21 (3.19–3.29) | 435 | 1.52 (1.45–1.59) | 2.41 (2.37–2.44) | 3.14 (3.09–3.17) | |||
| 60–74 | 692 | 1.26 (1.16–1.34) | 2.29 (2.26–2.32) | 3.16 (3.10–3.17) | 328 | 1.23 (1.12–1.35) | 2.26 (2.21–2.30) | 3.17 (3.12–3.20) | 364 | 1.28 (1.15–1.40) | 2.32 (2.28–2.36) | 3.10 (3.04–3.17) | |||
| 75–90 | 667 | 1.19 (1.14–1.24) | 2.24 (2.21–2.27) | 3.17 (3.11–3.20) | 326 | 1.24 (1.17–1.31) | 2.23 (2.18–2.27) | 3.12 (3.08–3.23) | 341 | 1.15 (1.06–1.22) | 2.25 (2.20–2.30) | 3.19 (3.13–3.20) | |||
| HDLC (mmol/L) | 18–29 | 667 | 1.06 (1.05–1.07) | 1.39 (1.37–1.40) | 1.97 (1.92–1.99) | 309 | 1.05 (1.05–1.06) | 1.31 (1.30–1.33) | 1.80 (1.71–1.87) | 358 | 1.09 (1.07–1.110 | 1.45 (1.43–1.48) | 2.06 (1.98–2.12) | ||
| 30–44 | 1,083 | 1.06 (1.06–1.07) | 1.39 (1.38–1.41) | 1.90 (1.86–1.97) | 368 | 1.06 (1.05–1.060 | 1.31 (1.30–1.33) | 1.83 (1.78–1.880 | 715 | 1.07 (1.06–1.08) | 1.44 (1.42–1.45) | 1.99 (1.89–2.03) | |||
| 45–59 | 722 | 1.06 (1.05–1.07) | 1.39 (1.38–1.41) | 1.98 (1.92–2.02) | 288 | 1.05 (1.05–1.07) | 1.32 (1.30–1.34) | 1.83 (1.79–1.86) | 434 | 1.07 (1.05–1.08) | 1.44 (1.42–1.46) | 2.03 (1.99–2.07) | |||
| 60–74 | 688 | 1.06 (1.06–1.07) | 1.36 (1.34–1.37) | 1.87 (1.85–1.94) | 326 | 1.06 (1.06–1.07) | 1.32 (1.31–1.34) | 1.87 (1.84–1.90) | 362 | 1.06 (1.06–1.08) | 1.39 (1.37–1.41) | 1.94 (1.82–1.97) | |||
| 75–90 | 664 | 1.06 (1.05–1.07) | 1.37 (1.36–1.39) | 1.95 (1.87–2.02) | 324 | 1.05 (1.05–1.06) | 1.31 (1.30–1.33) | 1.81 (1.77–1.86) | 340 | 1.07 (1.06–1.09) | 1.43 (1.41–1.45) | 2.05 (1.98–2.11) | |||
| sd-LDLC (mmol/L) | 18–29 | 669 | 0.26 (0.24–0.28) | 0.57 (0.56–0.59) | 0.98 (0.96–1.06) | 308 | 0.30 (0.28–0.34) | 0.63 (0.61–0.65) | 1.12 (1.01–1.17) | 361 | 0.23 (0.20–0.25) | 0.52 (0.51–0.54) | 0.91 (0.87–0.96) | ||
| 30–44 | 1,090 | 0.25 (0.23–0.26) | 0.59 (0.58–0.60) | 1.06 (1.01–1.07) | 373 | 0.25 (0.24–0.29) | 0.65 (0.63–0.66) | 1.09 (1.06–1.130 | 717 | 0.24 (0.23–0.26) | 0.56 (0.55–0.58) | 1.00 (0.95–1.06) | |||
| 45–59 | 728 | 0.29 (0.26–0.30) | 0.65 (0.64–0.66) | 1.15 (1.09–1.19) | 295 | 0.26 (0.22–0.33) | 0.68 (0.66–0.71) | 1.25 (1.15–1.28) | 433 | 0.29 (0.27–0.32) | 0.63 (0.61–0.640 | 1.08 (1.02–1.10) | |||
| 60–74 | 689 | 0.26 (0.24–0.28) | 0.62 (0.61–0.64) | 1.10 (1.06–1.15) | 328 | 0.26 (0.24–0.29) | 0.62 (0.60–0.64) | 1.11 (1.06–1.16) | 361 | 0.26 (0.19–0.28) | 0.62 (0.60–0.64) | 1.09 (1.03–1.18) | |||
| 75–90 | 673 | 0.25 (0.23–0.26) | 0.58 (0.57–0.59) | 1.07 (1.02–1.12) | 331 | 0.24 (0.23–0.26) | 0.58 (0.56–0.59) | 1.12 (1.04–1.150 | 342 | 0.25 (0.23–0.28) | 0.58 (0.56–0.60) | 1.03 (0.99–1.08) | |||
| GluG (mmol/L) | 18–29 | 671 | 3.65 (3.47–3.75) | 4.62 (4.58–4.65) | 5.62 (5.46–5.78) | 310 | 3..50 (3.37–3.69) | 4.64 (4.59–4.69) | 5.62 (5.40–5.78) | 361 | 3.71 (3.56–3.87) | 4.59 (4.55–4.63) | 5.61 (5.43–6.01) | ||
| 30–44 | 1,089 | 3.55 (3.42–3.65) | 4.63 (4.60–4.66) | 5.79 (5.66–5.86) | 373 | 3.58 (3.36–3.69) | 4.69 (4.64–4.74) | 5.93 (2.67–6.00) | 716 | (3.52 (3.36–3.66)) | 4.59 (4.56–4.63) | 5.71 (5.54–5.82) | |||
| 45–59 | 727 | 3.69 (3.61–3.83) | 4.84 (4.80–4.87) | 6.05 (5.96–6.13) | 294 | 3.73 (3.54–3.90) | 4.88 (4.83–4.94) | 6.06 (5.94–6.14) | 433 | 3.65 (3.57–3.83) | 4.80 (4.75–4.85) | 6.05 (5.93–6.19) | |||
| 60–74 | 690 | 3.23 (3.07–3.40) | 4.85 (4.81–4.90) | 6.18 (6.09–6.28) | 327 | 3.22 (3.02–3.45) | 4.86 (4.79–4.93) | 6.30 (6.13–6.43) | 363 | 3.23 (3.03–3.40) | 4.84 (4.78–4.91) | 6.10 (6.01–6.14) | |||
| 75–90 | 659 | 3.32 (3.06–3.47) | 4.91 (4.86–4.96) | 6.26 (6.14–6.35) | 328 | 3.33 (3.04–3.48) | 4.93 (4.86–5.00) | 6.30 (6.14–6.42) | 341 | 3.29 (2.98–3.50) | 4.89 (4.82–4.95) | 6.18 (6.10–6.34) | |||
| ApoA1 (nmol/L) | 18–29 | 702 | 1.11 (1.09–1.13) | 1.40 (1.38–1.41) | 1.88 (1.84–1.92) | 329 | 1.09 (1.08–1.13) | 1.35 (1.32–1.36) | 1.76 (1.74–1.85) | 373 | 1.11 (1.08–1.15) | 1.46 (1.44–1.48) | 1.95 (1.88–1.98) | ||
| 30–44 | 1,144 | 1.12 (1.10–1.13) | 1.42 (1.41–1.44) | 1.91 (1.88–1.94) | 387 | 1.12 (1.09–1.13) | 1.40 (1.38–1.42) | 1.90 (1.86–1.98) | 757 | 1.13 (1.10–1.14) | 1.44 (1.42–1.47) | 1.91 (1.88–1.94) | |||
| 45–59 | 743 | 1.11 (1.10–1.14) | 1.45 (1.43–1.46) | 1.92 (1.89–1.94) | 303 | 1.10 (1.07–1.14) | 1.40 (1.38–1.43) | 1.87 (1.80–1.89) | 440 | 1.11 (1.10–1.15) | 1.47 (1.45–1.49) | 1.93 (1.91–1.95) | |||
| 60–74 | 713 | 1.08 (1.09–1.13) | 1.45 (1.43–1.46) | 1.90 (1.87–1.92) | 336 | 1.10 (1.09–1.12) | 1.41 (1.38–1.42) | 1.83 (1.78–1.87) | 377 | 1.11 (1.09–1.16) | 1.48 (1.46–1.51) | 1.93 (1.91–1.96) | |||
| 75–90 | 723 | 1.10 (1.08–1.11) | 1.41 (1.40–1.42) | 1.86 (1.82–1.90) | 345 | 1.10 (1.08 –1.11) | 1.36 (1.33–1.38) | 1.79 (1.74–1.85) | 378 | 1.11 (1.08–1.13) | 1.46 (1.43–1.48) | 1.90 (1.85–1.93) | |||
| ApoB (nmol/L) | 18–29 | 667 | 0.48 (0.45–0.49) | 0.76 (0.75–0.77) | 1.05 (1.03–1.07) | 309 | 0.49 (0.45–0.52) | 0.78 (0.77–0.80) | 1.07 (1.05–1.08) | 358 | 0.47 (0.43–0.48) | 0.74 (0.73–0.75) | 1.02 (1.00–1.05) | ||
| 30–44 | 1,092 | 0.49 (0.47–0.50) | 0.79 (0.78–0.80) | 1.07 (1.05–1.08) | 374 | 0.49 (0.48–0.53) | 0.82 (0.81–0.84) | 1.09 (1.07–1.12) | 718 | 0.48 (0.45–0.50) | 0.77 (0.76–0.78) | 1.05 (1.03–1.07) | |||
| 45–59 | 729 | 0.50 (0.47–0.52) | 0.81 (0.80–0.82) | 1.10 (1.08–1.11) | 294 | 0.50 (0.45–0.52) | 0.81 (0.80–0.83) | 1.12 (1.10–1.13) | 435 | 0.50 (0.47–0.53) | 0.81 (0.80–0.82) | 1.08 (1.06–1.09) | |||
| 60–74 | 692 | 0.41 (0.40–0.46) | 0.79 (0.78–0.80) | 1.09 (1.07–1.10) | 328 | 0.40 (0.39–0.46) | 0.78 (0.76–0.80) | 1.09 (1.07–1.10) | 364 | 0.42 (0.38–0.48) | 0.80 (0.78–0.81) | 1.09 (1.05–1.11) | |||
| 75–90 | 667 | 0.41 (0.39–0.42) | 0.77 (0.76–0.78) | 1.09 (1.07–1.11) | 327 | 0.42 (0.38–0.45) | 0.77 (0.75–0.78) | 1.10 (1.05–1.11) | 340 | 0.40 (0.37–0.41) | 0.77 (0.76–0.79) | 1.09 (1.06–1.12) | |||
| LpA (nmol/L) | 18–29 | 624 | 42.36 (41.52–46.21) | 141.14 (135.34–147.07) | 384.08 (352.15–418.50) | 288 | 41.55 (40.15–45.80) | 139.72 (131.36–148.69) | 381.50 (341.93–402.78) | 339 | 45.27 (42.14–48.06) | 142.35 (134.86–150.80) | 409.38 (342.50–442.63) | ||
| 30–44 | 1,039 | 43.25 (42.44–47.10) | 146.91 (142.13–151.21) | 392.44 (371.25–408.23) | 352 | 42.42 (40.24–45.45) | 142.30 (134.45–150.23) | 355.06 (333.93–390.37) | 687 | 45.88 (42.84–49.37) | 149.26 (143.34–155.54) | 403.57 (375.09–423.32) | |||
| 45–59 | 689 | 44.76 (43.06–47.39) | 157.50 (151.70–163.76) | 405.72 (384.55–430.97) | 282 | 45.66 (44.37–52.03) | 149.30 (141.60–157.51) | 385.19 (354.19–406.61) | 407 | 44.40 (40.42–46.94) | 163.18 (154.36–170.93) | 434.45 (395.02–442.36) | |||
| 60–74 | 636 | 49.91 (45.35–54.67) | 155.79 (150.41–161.58) | 394.23 (372.01–411.78) | 301 | 51.08 (44.00–55.43) | 148.74 (140.98–155.63) | 377.98 (342.48–394.53) | 335 | 48.15 (43.04–55.65) | 162.13 (154.04–170.63) | 414.11 (379.25–428.35) | |||
| 75–90 | 614 | 49.82 (44.35–52.14) | 160.37 (154.77–166.06) | 381.52 (367.54–413.09) | 300 | 48.34 (43.32–53.67) | 161.04 (153.28–168.46) | 381.12 (348.52–417.29) | 314 | 50.15 (44.55–53.33) | 159.73 (151.38–168.87) | 388.98 (366.27–425.35) | |||
| LpAII (nmol/L) | 18–29 | 601 | 1.52 (1.18–1.85) | 17.77 (16.46–19.09) | 70.47 (66.93–76.06) | 275 | 1.18 (0.79–1.55) | 15.93 (14.25–17.70) | 68.90 (60.96–77.32) | 326 | 1.88 (1.31–2.23) | 19.32 (17.47–21.04) | 71.48 (67.58–77.47) | ||
| 30–44 | 991 | 1.35 (1.21–1.66) | 18.68 (17.65–19.750 | 76.02 (71.79–79.80) | 338 | 1.19 (0.91–1.50) | 17.12 (15.54–18.54) | 69.15 (61.52–71.82) | 653 | 1.54 (1.27–1.83) | 19.48 (18.18–20.88) | 80.85 (75.92–84.80) | |||
| 45–59 | 647 | 1.71 (1.51–2.30) | 21.52 (20.06–22.77) | 79.73 (75.35–83.40) | 265 | 1.78 (1.30–2.32) | 19.84 (18.00–21.94) | 74.48 (68.40–76.01) | 382 | 1.62 (1.25–2.63) | 22.68 (20.63–2.63) | 84.86 (79.81–89.95) | |||
| 60–74 | 600 | 2012 (1.79–2.68) | 21.06 (19.67–22.42) | 75.24 (72.15–78.09) | 287 | 2.29 (1.64–2.60) | 18.82 (17.19–20.49) | 72.34 (64.80–77.46) | 313 | 2.03 (1.76–3.06) | 23.11 (21.21–25.02) | 78.43 (73.91–82.65) | |||
| 75–90 | 580 | 2.01 (1.56–2.45) | 23.37 (21.80–24.78) | 77.90 (75.48–82.44) | 278 | 1.48 (0.94–2.69) | 22.84 (20.90–24.74) | 75.88 (69.12–77.02) | 302 | 2.07 (1.85–2.56) | 23.86 (21.67–25.89) | 83.95 (76.34–87.49) | |||
| HCYII (μmol/L) | 18–29 | 624 | 6.53 (6.31–6.80) | 11.04 (10.84–11.37) | 23.31 (22.40–24.59) | 275 | 7.88 (777–8.42) | 13.08 (12.74–13.71) | 24.61 (23.49–24.82) | 349 | 6.27 (6.19–6.48) | 9.66 (9.28–9.96) | 19.37 (18.01–19.66) | ||
| 30–44 | 1,077 | 6.72 (6.51–6.86) | 10.12 (9.95–10.32) | 20.68 (20.27–21.41) | 341 | 7.39 (7.16–7.91) | 12.40 (12.02–12.87) | 22.89 (21.81–24.70) | 736 | 6.51 (6.35–6.74) | 9.37 (9.17–9.56) | 18.72 (18.35–19.43) | |||
| 45–59 | 690 | 6.81 (6.72–6.94) | 10.46 (10.19–10.75) | 22.81 (21.25–23.95) | 265 | 8.01 (7.54–8.42) | 12.93 (12.45–13.36) | 24.75 (23.21–25.93) | 425 | 6.73 (6.55–6.82) | 9.36 (9.18–9.62) | 17.97 (17.16–19.45) | |||
| 60–74 | 641 | 7.35 (7.02–7.50) | 12.46 (12.10–12.77) | 24.18 (22.90–24.55) | 301 | 8.26 (7.68–8.83) | 14.33 (13.73–14.92) | 25.05 (24.28–25.91) | 340 | 6.98 (6.76–7.19) | 11.27 (10.89–11.59) | 20.06 (19.13–20.23) | |||
| 75–90 | 586 | 7.89 (7.44–8.15) | 14.03 (13.71–14.44) | 24.82 (24.15–24.99) | 275 | 8.33 (7.88–9.27) | 16.49 (15.28–16.78) | 25.29 (24.84–25.51) | 311 | 7.46 (6.94–7.94) | 12.65 (12.10–13.27) | 20.77 (19.88–23.91) | |||
LL, lower limit, CI, confidence interval; ME, median; UL, upper limit; TG, triglyceride; TC, total cholesterol; LDLC, low density lipoprotein cholesterol; HDLC, high density lipoprotein cholesterol; sd-LDLC, small dense low density lipoprotein cholesterol; GluG, glucose; ApoA1, apolipoprotein A1; ApoB, apolipoprotein B; LpA, lipoprotein a; HCY, homocysteine.
Table 6
| Analyte | Area | Sex | Age (years) | N | LL | UL | ME | RI in reagent package |
|---|---|---|---|---|---|---|---|---|
| TG (mmol/L) | – | M + F | – | 8,283 | 0.48 | 1.60 | 0.98 | 0.55–1.7 |
| TC (mmol/L) | – | M + F | – | 8,265 | 3.04 | 5.09 | 4.22 | 3.38–5.2 |
| LDLC (mmol/L) | – | M + F | – | 8,268 | 1.36 | 3.15 | 2.30 | 0.00–3.37 |
| HDLC (mmol/L) | – | M | – | 3,515 | 1.06 | 1.83 | 1.33 | >1.15 |
| – | F | – | 4,641 | 1.07 | 2.04 | 1.46 | ||
| sd-LDLC (mmol/L) | Northern China | |||||||
| -Shenyang | M + F | – | 1,481 | 0.34 | 1.14 | 0.68 | ||
| -Two other cities | – | 2,368 | 0.24 | 1.00 | 0.55 | |||
| Southern China | ||||||||
| -Nanning | M + F | – | 768 | 0.39 | 1.26 | 0.81 | ||
| -Three other cities | – | 3,604 | 0.23 | 0.93 | 0.51 | |||
| GluG (mmol/L) | Northern China | |||||||
| -Shenyang | M + F | 18–29 | 257 | 3.94 | 5.57 | 4.76 | 3.33–5.55 | |
| 30–44 | 439 | 4.05 | 5.90 | 4.85 | ||||
| 45–59 | 313 | 4.13 | 6.25 | 5.05 | ||||
| 60–74 | 228 | 3.96 | 6.47 | 5.15 | ||||
| 75–90 | 237 | 4.13 | 6.39 | 5.17 | ||||
| -Two other cities | M + F | 18–29 | 414 | 3.46 | 5.77 | 4.52 | ||
| 30–44 | 650 | 3.42 | 5.58 | 4.47 | ||||
| 45–59 | 414 | 3.56 | 5.93 | 4.67 | ||||
| 60–74 | 462 | 3.10 | 6.05 | 4.71 | ||||
| 75–90 | 432 | 3.05 | 6.11 | 4.77 | ||||
| Southern China | ||||||||
| -Nanning | M + F | 18–29 | 324 | 3.09 | 5.84 | 4.60 | – | |
| 30–44 | 241 | 3.61 | 6.01 | 4.75 | – | |||
| 45–59 | 123 | 3.70 | 6.08 | 4.85 | – | |||
| 60–74 | 106 | 3.82 | 6.53 | 5.09 | – | |||
| 75–90 | 38 | 3.03 | – | 4.99 | – | |||
| -Three other cities | M + F | 18–29 | 813 | 2.89 | 5.13 | 4.00 | – | |
| 30–44 | 1,032 | 2.93 | 5.30 | 4.01 | – | |||
| 45–59 | 633 | 2.94 | 5.77 | 4.27 | – | |||
| 60–74 | 543 | 2.97 | 5.85 | 4.47 | – | |||
| 75–90 | 579 | 3.01 | 6.03 | 4.63 | – | |||
| ApoA1 (nmol/L) | Southern China | |||||||
| -Chengdu | M | – | 503 | 1.25 | 2.03 | 1.60 | – | |
| F | – | 758 | 1.32 | 2.20 | 1.74 | – | ||
| -Three other cities | M | – | 1,422 | 1.16 | 1.97 | 1.50 | – | |
| F | – | 1,652 | 1.18 | 2.15 | 1.61 | – | ||
| ApoB (nmol/L) | – | M + F | – | 8,257 | 0.47 | 1.07 | 0.79 | – |
| LpA (nmol/L) | – | M + F | – | 7,679 | 42.43 | 397.15 | 152.23 | – |
| LpAII (nmol/L) | – | M + F | – | 7,379 | 1.76 | 75.64 | 19.31 | – |
| HCYII (μmol/L) | – | M | 18–29 | 694 | 7.65 | 23.50 | 12.92 | – |
| – | 30–44 | 771 | 7.38 | 22.62 | 12.35 | – | ||
| – | 45–59 | 620 | 7.78 | 24.46 | 12.68 | – | ||
| – | 60–74 | 606 | 8.16 | 24.47 | 13.74 | – | ||
| – | 75–90 | 592 | 8.35 | 25.32 | 16.55 | – | ||
| – | F | 18–29 | 984 | 6.43 | 18.18 | 9.57 | – | |
| – | 30–44 | 1,494 | 6.40 | 18.19 | 9.10 | – | ||
| – | 45–59 | 803 | 6.73 | 17.10 | 9.51 | – | ||
| – | 60–74 | 670 | 7.02 | 19.43 | 10.96 | – | ||
| – | 75–90 | 539 | 7.83 | 20.20 | 12.64 | – |
LL, lower limit, UL, upper limit; ME, median; RI, reference interval; TG, triglyceride; M, male; F, female; TC, total cholesterol; LDLC, low density lipoprotein cholesterol; HDLC, high density lipoprotein cholesterol; sd-LDLC, small dense low density lipoprotein cholesterol; GluG, glucose; ApoA1, apolipoprotein A1; ApoB, apolipoprotein B; LpA, lipoprotein a; HCY, homocysteine.
Discussion
This study was the first multicenter study to summarize the nationwide research on RIs of fasting lipids and apolipoproteins for healthy Chinese adults aged 18–90 years in different regions with the same equipment and stringent and consistent criteria. Since the improvement of Chinese living standards, a high-fat energy dense diet and sedentary lifestyle have led to the rapid increase in population with CVD. Blood lipids, apolipoproteins, lipoproteins, HCY, and GluG are the main screening tests for evaluating cardiovascular risk and thus enable early intervention, yet the baseline research for these assays in the general population is limited. Therefore, the establishment of age-specific and sex-specific RIs with high precision in healthy Chinese adults is indeed warranted from the point of view of CVD prevention. The lack of a China-specific RI established by large sample size multicenter study was addressed by our study.
All the data from 8,283 healthy Chinese adults from seven representative cities were analyzed. After partitioning by region, sex, and age, the least number of reference individuals was in the subgroup of male sex and 45–59 years old for HCY in northern China, with 198 individuals. These data probably provide the most accurate and precise RIs with narrow CIs on each of the derived reference limits that are available for the general Chinese population.
3N-ANOVA was used to identify the source of variances and to partition the data for results presentation. The differences in sex and the age were found in HDLC, GluG, and HCYII. Scatter charts further confirm that the level of HCY in male participants was clearly higher than that in female participants, whereas the levels of HDLC and ApoA1 in males were lower than those in females. ApoA1 is a major protein component of high-density lipoprotein (HDL). Numerous studies have identified HDLC and ApoA1 as having a direct protective role against the development of CVD (27,28), suggesting that an elevated level of HDLC and ApoA1 may be inversely related to the incidence of CVD. On the contrary, an elevated level of HCY and GluG has been significantly positively associated with the incidence of CVD (29). Therefore, male sex, elevated HCY levels, and decreased levels of HDLC and ApoA1 maybe may explain why the incidence of CVD is higher in males than in females of reproductive age. Furthermore, the scatter charts also showed that the GluG and HCY level increased gradually with age, which corresponds with the incidence of CVD also increasing gradually with age.
Apparent regional differences were observed in three analytes: sd-LDLC, GluG, and ApoA1. For northern China, the sd-LDLC and GluG levels in Shenyang were significantly higher than those in Ningxia and Beijing. For southern China, sd-LDLC and GluG levels in Nanning were significantly higher than those in the 3 other cities, whereas sd-LDLC and GluG levels in Chengdu were significantly lower than those in the three other cities. The level of ApoA1 in Chengdu was significantly higher than that in the three other cities. To verify this, these assays were classified in the final results of our study by city group (northern China: Shenyang vs. two other cities; southern China: Nanning vs. two other cities and Chengdu vs. three other cities). However, we were not able to identify the reason for the prominent between-city difference in the level of sd-LDLC, GluG, and ApoA1 with the 3N-ANOVA used in this study. Considering that China has a diversity of ethnic groups and cultures, as well as heterogeneity of socioeconomics in different regions, the observed between-city differences may be explained by the difference of genetic background and environmental determinants such as diet, lifestyle, geographic characteristics, local climate, and economic development (30).
A study has shown that a long-standing association exists between elevated TG and TC levels and CVD (31). In females aged 45–55 years old, there is an interesting change in scatter charts, where TG and TC increases rapidly. We also found that for the age group of >55 years, the levels of TG and TC in females were gradually surpassed those in males. This may be related to the decrease in estrogen levels affecting women near this age, which is one of the explanations for the incidence of CVD being very low in women of reproductive age but rising to a significant level in postmenopausal women (32).
Age- and sex-specific RIs of serum lipids among children and adolescents have been reported by several non-Chinese studies (33-38). Studies in Ireland (33), north India (36), and The Netherlands (38) showed higher TC, TG, and LDLC levels but lower HDLC levels compared to our Chinese study. These differences may result from the variability in physical activity, the prevalence of obesity, and distinct diet in these countries (39,40).
There are some limitations in our study. First, a cross-sectional design with an age range confined to 18–90 years old was employed, so we did not perform a longitudinal analysis of individuals. Future studies are necessary to validate the results using longitudinal data and expand the age range to include children and adolescents. Second, we did not recruit participants in rural areas; thus, the proportion of participants living in rural areas may be lower than that of urban residents. Third, only sex and age were considered as influencing factors, and we did not collect information on other possible confounding factors such as BMI, smoking, drinking, dietary habits, and socioeconomic status, which may influence the levels of biochemical markers of blood lipids.
Conclusions
In conclusion, this study is the first multicenter study, to use data from seven representative cities of China with the Mindray fully automatic biochemical analyzer chemistry BS2000 system (Mindray Co., Ltd.), performed to present the RIs of blood lipids for the general population of adults in China. The data collected in this study included RIs for the concentrations of all biochemical markers of blood lipids in adults aged 18–90 years. Sex and age were considered as the main influencing factors. After appropriate validation, these established RIs can be employed by other clinical laboratories in addition to the clinical decision limits (CDLs) recommended by guidelines. Furthermore, these data can be used to enhance clinical diagnosis strategies and health promotion.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://cdt.amegroups.com/article/view/10.21037/cdt-23-369/rc
Data Sharing Statement: Available at https://cdt.amegroups.com/article/view/10.21037/cdt-23-369/dss
Peer Review File: Available at https://cdt.amegroups.com/article/view/10.21037/cdt-23-369/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://cdt.amegroups.com/article/view/10.21037/cdt-23-369/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of Beijing Anzhen Hospital (No. KS2020005) and informed consent was taken from all the patients. All participating hospitals were informed and agreed with this study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Pirillo A, Norata GD. The burden of hypercholesterolemia and ischemic heart disease in an ageing world. Pharmacol Res 2023;193:106814. [Crossref] [PubMed]
- Global Cardiovascular Risk Consortium. Global Effect of Modifiable Risk Factors on Cardiovascular Disease and Mortality. N Engl J Med 2023;389:1273-85. [Crossref] [PubMed]
- Gyldenkerne C, Mortensen MB, Kahlert J, et al. 10-Year Cardiovascular Risk in Patients With Newly Diagnosed Type 2 Diabetes Mellitus. J Am Coll Cardiol 2023;82:1583-94. [Crossref] [PubMed]
- Sun L, Clarke R, Bennett D, et al. Causal associations of blood lipids with risk of ischemic stroke and intracerebral hemorrhage in Chinese adults. Nat Med 2019;25:569-74. [Crossref] [PubMed]
- Li WL, Sang H, Xu X, et al. The correlation study on homocysteine, blood lipids and blood glucose levels in patients with cerebral infarction. Am J Transl Res 2021;13:5659-64. [PubMed]
- Jia K, Zhang C, Huang X, et al. Reference Intervals of Serum Sodium, Potassium, and Chlorine in Chinese Han Population and Comparison of Two ISE Methods. J Clin Lab Anal 2015;29:226-34. [Crossref] [PubMed]
- Mu R, Chen W, Pan B, et al. First definition of reference intervals of liver function tests in China: a large-population-based multi-center study about healthy adults. PLoS One 2013;8:e72916. [Crossref] [PubMed]
- CLSI EP28-A3C. Defining, establishing, and verifying reference intervals in the clinical laboratory. Wayne PAL Clin Lab Stand Inst 2010. Available online: https://clsi.org/standards/
- Liu J, Dai Y, Yuan E, et al. Age-specific and sex-specific reference intervals for non-fasting lipids and apolipoproteins in 7260 healthy Chinese children and adolescents measured with an Olympus AU5400 analyser: a cross-sectional study. BMJ Open 2019;9:e030201. [Crossref] [PubMed]
- Li Y, Ma Y, Luo J, et al. Identifying reference values for serum lipids in Chinese children and adolescents aged 6-17 years old: A national multicenter study. J Clin Lipidol 2021;15:477-87. [Crossref] [PubMed]
- Qin X, Mo C, Zeng Z, et al. Reference intervals for serum lipids in coastal males from Fangchenggang. Clin Lab 2013;59:1289-95. [Crossref] [PubMed]
- He H, Lv R, Li S, et al. Reference intervals and factors contributing to serum glycated albumin levels in West China. Clin Lab 2014;60:119-24. [Crossref] [PubMed]
- Wang Z, Ni X, Gao D, et al. Investigation of the Reference Interval Values of Fasting Plasma Glucose, Blood Pressure, and Blood Lipids in the Longevity People Aged 90 Years Old and Above. Diabetes Metab Syndr Obes 2021;14:3711-8. [Crossref] [PubMed]
- Chen C, Wang X, Tan Y, et al. Reference intervals for serum 1,5-anhydroglucitol of a population with normal glucose tolerance in Jiangsu Province. J Diabetes 2020;12:447-54. [Crossref] [PubMed]
- Gu T, Zhou W, Sun J, et al. Gender and Age Differences in Lipid Profile Among Chinese Adults in Nanjing: a Retrospective Study of Over 230,000 Individuals from 2009 to 2015. Exp Clin Endocrinol Diabetes 2018;126:429-36. [Crossref] [PubMed]
- Martí-Carvajal AJ, Solà I, Lathyris D, et al. Homocysteine-lowering interventions for preventing cardiovascular events. Cochrane Database Syst Rev 2017;8:CD006612. [PubMed]
- Gazi IF, Tsimihodimos V, Tselepis AD, et al. Clinical importance and therapeutic modulation of small dense low-density lipoprotein particles. Expert Opin Biol Ther 2007;7:53-72. [Crossref] [PubMed]
- Bhargava S, de la Puente-Secades S, Schurgers L, et al. Lipids and lipoproteins in cardiovascular diseases: a classification. Trends Endocrinol Metab 2022;33:409-23. [Crossref] [PubMed]
- Walldius G, Jungner I. The apoB/apoA-I ratio: a strong, new risk factor for cardiovascular disease and a target for lipid-lowering therapy--a review of the evidence. J Intern Med 2006;259:493-519. [Crossref] [PubMed]
- Di Cesare F, Luchinat C, Tenori L, et al. Age- and Sex-Dependent Changes of Free Circulating Blood Metabolite and Lipid Abundances, Correlations, and Ratios. J Gerontol A Biol Sci Med Sci 2022;77:918-26. [Crossref] [PubMed]
- Friedman LA, Morrison JA, Daniels SR, et al. Sensitivity and specificity of pediatric lipid determinations for adult lipid status: findings from the Princeton Lipid Research Clinics Prevalence Program Follow-up Study. Pediatrics 2006;118:165-72. [Crossref] [PubMed]
- Joint committee for guideline revision. 2016 Chinese guidelines for the management of dyslipidemia in adults. J Geriatr Cardiol 2018;15:1-29.
- Hoaglin DC, Iglewicz B. Fine-Tuning Some Resistant Rules for Outlier Labeling. J Am Stat Assoc 1987;82:1147-9. [Crossref]
- Ichihara K, Kawai T. Determination of reference intervals for 13 plasma proteins based on IFCC international reference preparation (CRM470) and NCCLS proposed guideline (C28-P, 1992): a strategy for partitioning reference individuals with validation based on multivariate analysis. J Clin Lab Anal 1997;11:117-24. [Crossref] [PubMed]
- Ichihara K. Statistical considerations for harmonization of the global multicenter study on reference values. Clin Chim Acta 2014;432:108-18. [Crossref] [PubMed]
- Ichihara K, Boyd JCIFCC Committee on Reference Intervals and Decision Limits (C-RIDL). An appraisal of statistical procedures used in derivation of reference intervals. Clin Chem Lab Med 2010;48:1537-51. [Crossref] [PubMed]
- Rashid S, Uffelman KD, Barrett PH, et al. Effect of atorvastatin on high-density lipoprotein apolipoprotein A-I production and clearance in the New Zealand white rabbit. Circulation 2002;106:2955-60. [Crossref] [PubMed]
- Barrett TJ, Distel E, Murphy AJ, et al. Apolipoprotein AI) Promotes Atherosclerosis Regression in Diabetic Mice by Suppressing Myelopoiesis and Plaque Inflammation. Circulation 2019;140:1170-84. [Crossref] [PubMed]
- Xanthakis V, Enserro DM, Murabito JM, et al. Ideal cardiovascular health: associations with biomarkers and subclinical disease and impact on incidence of cardiovascular disease in the Framingham Offspring Study. Circulation 2014;130:1676-83. [Crossref] [PubMed]
- Li S, Liu Z, Joseph P, et al. Modifiable risk factors associated with cardiovascular disease and mortality in China: a PURE substudy. Eur Heart J 2022;43:2852-63. [Crossref] [PubMed]
- Nordestgaard BG, Varbo A. Triglycerides and cardiovascular disease. Lancet 2014;384:626-35. [Crossref] [PubMed]
- ESHRE Capri Workshop Group. Hormones and cardiovascular health in women. Hum Reprod Update 2006;12:483-97. [Crossref]
- Hughes D, Crowley J, O'Shea P, et al. Lipid reference values in an Irish population. Ir J Med Sci 2021;190:117-27. [Crossref] [PubMed]
- Malati T, Mahesh MR. Reference intervals for serum total cholesterol, HDL-cholesterol, LDL-cholesterol, triglycerides, Lp (a), apolipoprotein A-I, A-II, B, C-II, C-III, and E in healthy South Indians from Andhra Pradesh. Indian J Clin Biochem 2009;24:343-55. [Crossref] [PubMed]
- Tang Tsana CD, Sadeu Wafeu G, Ama Moor VJ, et al. Validation of lipid profile measurement methods and establishment of reference values in a sub-Saharan African population. Lipids 2022;57:233-40. [Crossref] [PubMed]
- Yadav D, Gupta M, Mishra S, et al. Reference interval for lipid profile in North Indian population from Rajasthan according to various partitioning criteria. Clin Chim Acta 2013;426:145-51. [Crossref] [PubMed]
- Ashavaid TF, Kondkar AA, Todur SP, et al. Lipid, lipoprotein, apolipoprotein and lipoprotein(a) levels: reference intervals in a healthy Indian population. J Atheroscler Thromb 2005;12:251-9. [Crossref] [PubMed]
- Balder JW, de Vries JK, Nolte IM, et al. Lipid and lipoprotein reference values from 133,450 Dutch Lifelines participants: Age- and gender-specific baseline lipid values and percentiles. J Clin Lipidol 2017;11:1055-1064.e6. [Crossref] [PubMed]
- Adair LS, Gordon-Larsen P, Du SF, et al. The emergence of cardiometabolic disease risk in Chinese children and adults: consequences of changes in diet, physical activity and obesity. Obes Rev 2014;15:49-59. [Crossref] [PubMed]
- Huang X, Gong R, Lin J, et al. Effects of lipoprotein lipase gene variations, a high-carbohydrate low-fat diet, and gender on serum lipid profiles in healthy Chinese Han youth. Biosci Trends 2011;5:198-204. [Crossref] [PubMed]


