
Hybrid total arterial minimally invasive off-pump coronary revascularization and percutaneous coronary intervention strategy for multivessel coronary artery disease: a cohort study with a median 11-year follow-up
Highlight box
Key findings
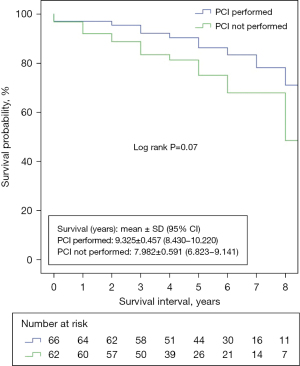
• Only 50.7% of the sample received the intended percutaneous coronary intervention (PCI) treatment. This rate was significantly lower in the cohort with chronic coronary artery disease, at just 39.1%. The total major adverse cardiac and cerebral events (MACCE) rate was 36.7% over a median follow-up period of 11 years. The survival rates at 3 and 5 years were 92% and 85%, respectively. Patients who did not receive the intended PCI had a mean survival rate of 6.8–9.1 years, whereas those who completed the intended hybrid treatment had a better mean survival rate of 8.4–10.2 years.
What is known and what is new?
• Hybrid coronary revascularization (HCR) is often referred to as a fusion of minimally invasive direct coronary artery bypass and PCI techniques. The existing body of research focuses mostly on the comparison of outcomes between HCR and coronary artery bypass grafting (CABG) or PCI, with the majority of studies showing comparable survival in mid- and long-term follow-up for HCR and CABG. However, HCR is associated with a higher MACCE rate, mostly due to repeat revascularization.
• Our research encompasses patients who have undergone single or multiple bypass minimally invasive off pump total arterial revascularization, combined with PCI. Our goal was to authenticate the pragmatic obstacles that emerge throughout the execution of an HCR methodology.
What is the implication, and what should change now?
• After coronary bypass surgery, the attention going forward needs to be devoted toward the organization of the PCI step in the treatment process.
Introduction
In developed nations, coronary artery disease (CAD) continues to be the primary cause of morbidity and mortality, notwithstanding on-going advancements in prevention and treatment. In the past three decades, the optimal strategy for coronary artery revascularization has been the subject of intense debate and investigation. Long-term prognosis is most favourable for patients undergoing total arterial myocardial revascularization who have significant stenotic CAD (1). Particularly in the case of predictive coronary vessels, such as the main stem and proximal left anterior descending (LAD) artery, the implementation of arterial coronary bypass over percutaneous coronary intervention (PCI) results in a survival advantage for the patient (2). Complete sternotomy, on the other hand, is the greatest burden for the patients.
The debate concerning the superior therapeutic approach is still on going. Cardiac surgeons must prioritise the superior long-term outcomes offered by high-quality grafts and reduce invasiveness, notwithstanding the rapid advancements in PCI and drug-eluting stents. A therapeutic alternative, hybrid coronary revascularization (HCR), which combines coronary artery bypass grafting (CABG) and PCI, is indicated for specific patients diagnosed with multivessel CAD (MV CAD). HCR consists of minimally invasive direct coronary artery bypass (MIDCAB) or minimally invasive multivessel CABG (MICS-CABG) in conjunction with PCI. These procedures are performed in a staged fashion, with simultaneous hybrid approaches being less common.
CABG with minimally invasive techniques is a swiftly expanding field (3). Preventing repeated revascularization and achieving graft patency rates comparable to conventional CABG are the principal objectives (3). The secondary objective is to decrease the degree of invasiveness, which is linked to decreased surgical pain and postoperative distress. This, in turn, enables a quicker recovery to regular social life (3). Consequently, an important contemporary challenge in cardiac surgery is the enhancement of the patient’s quality of life in addition to increasing life expectancy.
The extant body of research primarily concentrates on the comparison of outcomes between HCR and CABG or PCI. Furthermore, HCR is defined primarily as MIDCAB and PCI. Given the various criteria for HCR identified in the current body of literature, as well as several hybrid revascularization techniques, our primary goal was to analyse the characteristics and track the development of HCR patients operated on in our centre (Robert Bosch Hospital) over both short and long periods of time. Additionally, we aimed to authenticate the real-life obstacles associated with implementing an HCR approach. We present this article in accordance with the STROBE reporting checklist (available at https://cdt.amegroups.com/article/view/10.21037/cdt-23-413/rc).
Methods
Patients and study design
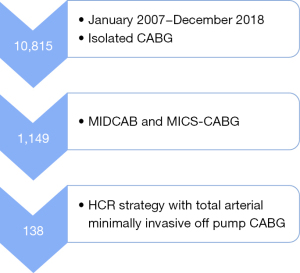
From January 2007 to December 2018, a retrospective data analysis of the isolated CABG procedures performed at Robert Bosch Hospital was conducted. We identified 1,149 patients who underwent minimally invasive off-pump CABG surgery by excluding sternotomy CABG. Those with multivessel CAD who were to undergo an HCR strategy in conjunction with total arterial MICS-CABG or MIDCAB were identified from this group. The HCR strategy was delineated by two distinct approaches: “the reverse hybrid approach”, which involved PCI stenting prior to minimally invasive CABG, typically in the case of acute coronary syndrome (4), and first surgery followed by PCI stenting of the non-surgically treated territory, which constituted “the hybrid approach” (4). Ultimately, 138 patients were identified based on these criteria; of these, 97 underwent MIDCAB and 41 underwent MICS-CABG (Figure 1). Data on demographics, clinical characteristics and adverse events were meticulously recorded and examined. In addition, the European System for Cardiac Operative Risk Evaluation score I additive (EuroSCORE I) additive and SYNergy between PCI with TAXUS and Cardiac Surgery (SYNTAX) Score I were determined for each patient.
The primary endpoints were the rate of major adverse cardiac and cerebral events (MACCE) during follow-up, as well as the survival rate in mid- and long-term follow-up. All-cause mortality, myocardial infarction, recurrent revascularization via PCI or CABG, stroke, or transient ischemic attack were all included in the MACCE definition. Follow-up data was collected through correspondence or by telephone interviews with study participants or with their referring cardiologists or general practitioners, in cases where the person could not be contacted. The survey consisted of inquiries regarding following hospitalisations, neurological events and repeat revascularization either by intervention or by surgery. If relevant, information regarding the precise date and underlying cause of death were also gathered.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the ethics board of the Medical University Tübingen (ethics registration No. 777/2021B02) and informed consent was taken from all the patients.
Surgical management
Standard procedure entails a 6 cm left anterior thoracotomy in the fifth intercostal space or the inframammary fold, which facilitates access to the LAD. Following the transition to single lung ventilation, the procedure of harvesting the left internal thoracic artery (LITA) was executed under direct vision utilising conventional surgical instruments. In order to prepare the LITA graft for bypass, systemic heparinization and internal administration of papaverine solution were performed. When more than one coronary anastomosis is required for individuals with MV CAD, anterolateral access to the heart becomes substantially more difficult. The second arterial graft used was an endoscopically obtained radial artery. The LITA was utilised in MICS-CABG to revascularize the LAD and diagonal branch, while the radial artery via a T-graft from the LITA bypass supplied the lateral and/or dorsal myocardial territories. A coronary shunt was employed to minimise the strong coronary backflow and prevent myocardial ischemia. A blower/mister was utilised in all cases to control leftover bleeding and to facilitate visualisation of the coronary artery anastomosis. In all cases, an intraoperative ultrasonic flow measurement was undertaken to validate the bypass outcome. A catheter for intercostal nerve blockade was inserted in order to alleviate postoperative pain. Following surgery, 500 mg of aspirin is administered to each patient. Most patients were extubated before leaving the operating room.
Statistical analysis
The categorical variables are presented as absolute and percentages and all continuous variables are presented as mean ± standard deviation. Data that were absent were omitted from the analysis. All tests were two-tailored, with differences considered statistically significant if the P value was less than 0.05. No test for normality distribution was carried out. Using the Kaplan-Meier curve, we estimated the patients’ survival rates. To determine the differences between the groups, the log-rank test was used. To analyse data, we employed the statistic program SPSS version 28.0 for Windows (SPSS Inc., Chicago, IL, USA).
Results
Preoperative data
The study’s patients had a high mean EuroSCORE I of 7.6±10.2. A total of 79 individuals (57.2%) had three vessel disease (VD). There were 27 urgent surgeries (19.6%). In the three months preceding surgery, 53 (38.4%) patients had an acute myocardial infarction, and 50 (36.2%) of them had the culprit lesion treated with a PCI, leaving the remaining vessel(s) to be operated on.
A subsequent analysis was conducted in which patients undergoing emergent surgeries or who had experienced myocardial infarction within the three months prior to the procedure were excluded. This subset was categorised as having “chronic coronary artery disease”. Sixty-nine patients made up this subpopulation. The EuroSCORE I additive was found to be lower than that of the entire cohort, and a lower proportion of patients (36.2% vs. 24.6%) had undergone PCI treatment prior to surgery. Conversely, the proportion of patients who reported a positive history of stroke was greater (6.5 % vs. 10.1%).
The SYNTAX Score I was computed for the complete cohort. Tertiles are used to classify the SYNTAX Score: low (<16), intermediate [16–22], and high (>22). The mean SYNTAX Score of the patients comprising our study group was 22.9±9.4. The mean SYNTAX Score for the subgroup presenting with chronic CAD was marginally reduced to 22.2±9.3. Table 1 provides an overview of the demographic and baseline characteristics of both the entire cohort and the chronic CAD subgroup.
Table 1
| Variables | All (n=138) | Chronic CAD (n=69) |
|---|---|---|
| Age (years) | 69.6±11.2 | 68.8±11.3 |
| Male gender | 109 (79.0) | 57 (82.6) |
| BMI (kg/m2) | 27.1±4.2 | 27.4±4.6 |
| EuroSCORE I additive | 7.6±10.2 | 5.9±8.0 |
| SYNTAX Score I | 22.9±9.4 | 22.2±9.3 |
| COPD | 13 (9.4) | 8 (11.6) |
| Smoking | 36 (26.1) | 21 (30.4) |
| Arterial hypertension | 136 (98.6) | 67 (97.1) |
| Atrial fibrillation | 24 (17.4) | 11 (15.9) |
| Peripheral vascular disease | 23 (16.7) | 11 (15.9) |
| Medically treated type II diabetes | 33 (23.9) | 13 (18.8) |
| Preoperative creatinine value (mg/dL) | 1.2±1.3 | 1.1±0.6 |
| Impaired renal function (GFR <50 mL/min/1.73 m2) | 33 (23.9) | 16 (23.2) |
| History of stroke | 9 (6.5) | 7 (10.1) |
| Acute myocardial infarction (<3 months) | 53 (38.4) | 0 |
| History of PCI | 50 (36.2) | 17 (24.6) |
| Extent of CAD | ||
| 1 VD | 2 (1.4) | 1 (1.4) |
| 2 VD | 57 (41.3) | 26 (37.7) |
| 3 VD | 79 (57.2) | 42 (60.9) |
| LVEF (%) | ||
| >50 | 91 (65.9) | 46 (66.7) |
| 30–50 | 34 (24.6) | 17 (24.6) |
| <30 | 13 (9.4) | 6 (8.7) |
| Status | ||
| Elective | 111 (80.4) | 69 (100.0) |
| Urgent | 27 (19.6) | 0 |
Values are presented as n (%) or mean ± SD. CAD, coronary artery disease; BMI, body mass index; EuroSCORE, European System for Cardiac Operative Risk Evaluation; SYNTAX, SYNergy between PCI with TAXUS and Cardiac Surgery; COPD, chronic obstructive pulmonary disease; GFR, glomerular filtration rate; PCI, percutaneous coronary intervention; VD, vessel disease; LVEF, left ventricular ejection fraction; SD, standard deviation.
Operative and 30-day results
Among the 138 patients, 97 had a MIDCAB operation, 39 had a MICS-CABG with two grafts, and two had a total of three distal anastomoses. All patients received LITA as transplant material. A radial artery was used as an extra arterial transplant in 25 individuals. All patients had bypasses to the anterior wall, 18 had bypasses to the lateral wall, and only one had a bypass to the posterior wall of the heart. Neither a sternotomy nor a conversion to CPB occurred. The mean transfusion rates for red blood cells (0.4±1.6 units/patient), fresh frozen plasma (0.3±1.7 units/patient), and platelets (0.1±0.4 units/patient) were found to be at a low level. The subset of patients with chronic CAD exhibited nearly identical intraoperative data.
Patients spent an average of 8.4 days in the hospital and 1.5 days in the intensive care unit (ICU) following surgery, indicating a low prevalence of postoperative problems.
The subgroup with chronic CAD had a similar risk profile of in-hospital postoperative complications, with the exception of a lower rate of surgical site wound infection (4.3% vs. 1.4%). A decreased rate of planned PCI was observed in these patients within the initial 30 days (8.7% vs. 5.8%).
Seven patients (5.1%) had reoperations due to bleeding. Three patients died within the first 30 days. In the chronic CAD group, there were no 30-day fatalities.
Tables 2,3 provide details on the operational and postoperative results, respectively.
Table 2
| Variables | All (n=138) | Chronic CAD (n=69) |
|---|---|---|
| Type of surgery | ||
| MIDCAB | 97 (70.3) | 49 (71.0) |
| MICS-CABG | 41 (29.7) | 20 (29.0) |
| 2 grafts | 39 | 19 |
| 3 grafts | 2 | 1 |
| Use of LITA | 138 (100.0) | 69 (100.0) |
| Use of radial artery | 25 (18.1) | 13 (18.8) |
| Conversion to sternotomy and/or CPB | 0 | 0 |
| Number of grafts to the anterior wall | ||
| 1 | 116 (84.1) | 60 (87.0) |
| 2 | 22 (15.9) | 9 (13.0) |
| Number of grafts to the posterior wall | ||
| 1 | 1 (0.7) | 1 (1.4) |
| Number of grafts to the lateral wall | ||
| 1 | 17 (12.3) | 8 (11.6) |
| 2 | 1 (0.7) | 1 (1.4) |
Values are presented as n (%). CAD, coronary artery disease; MIDCAB, minimally invasive direct coronary artery bypass; MICS-CABG, minimally invasive multivessel coronary artery bypass grafting; LITA, left internal thoracic artery; CPB, cardiopulmonary bypass.
Table 3
| Variables | All (n=138) | Chronic CAD (n=69) |
|---|---|---|
| Postoperative new onset renal failure requiring dialysis | 3 (2.2) | 2 (2.9) |
| Postoperative new onset atrial fibrillation | 3 (2.2) | 3 (4.3) |
| Postoperative stroke | 3 (2.2) | 2 (2.9) |
| Surgical site wound infection | 6 (4.3) | 1 (1.4) |
| Postoperative CPR | 2 (1.4) | 0 |
| Postoperative acute myocardial infarction | 2 (1.4) | 0 |
| Postoperative PCI (30-d) | 12 (8.7) | 4 (5.8) |
| Reoperation for bleeding | 7 (5.1) | 3 (4.3) |
| Reoperation with bypass revision | 1 (0.7) | 0 |
| Length of ICU stay (d) | 1.5±1.7 | 1.3±0.7 |
| Length of hospital stay (d) | 8.4±4.2 | 8.2±3.3 |
| 30-d mortality | 3 (2.2) | 0 |
Values are presented as n (%) or mean ± SD. CAD, coronary artery disease; CPR, cardiopulmonary resuscitation; PCI, percutaneous coronary intervention; ICU, intensive care unit; SD, standard deviation.
Follow-up data
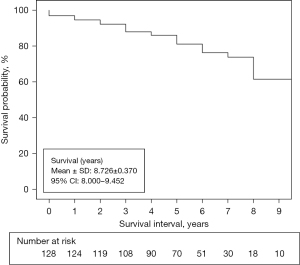
Long-term follow-up was available for the vast majority of patients (92.8%, n=128), with a mean duration of 8.7±0.3 years and a median duration of 11 years. The chronic CAD group exhibited an even higher follow-up rate, comprising 65 out of 69 cases, or 94.2%. Table 4 shows the number of MACCE that occurred during the follow-up period.
Table 4
| Variables | All (n=128)† | Chronic CAD (n=65)† |
|---|---|---|
| Myocardial infarction | 3 (2.3) | 1 (1.5) |
| Repeat revascularization by means of PCI | 18 (14.1) | 10 (15.4) |
| Repeat revascularization by means of CABG | 0 | 0 |
| Stroke | 4 (3.1) | 4 (6.2) |
| Fatalities | 28 (21.9) | 10 (15.4) |
| Cardiac-related fatalities | 7 (5.5) | 4 (6.2) |
| MACCE (total) | 47 (36.7) | 19 (29.2) |
Values are presented as n (%). †, 92.8% follow up rate for the entire cohort, corresponding to 128 out of 138, 10 patients were lost to follow up; 94.2% follow up rate for the chronic CAD subgroup, corresponding to 65 out of 69, 4 patients were lost to follow up. MACCE, major adverse cardiac and cerebral events; CAD, coronary artery disease; PCI, percutaneous coronary intervention; CABG, coronary artery bypass grafting.
During follow-up, 18 of the 29 patients who had coronary angiography underwent PCI. Five of the 18 patients treated with PCI had had a PCI performed shortly before surgery. In the end, only 70 of the 138 patients underwent the planned PCI procedure, accounting for 50.7% of the total study group. The chronic CAD group had a substantially lower PCI rate of only 39.1%.
Throughout the duration of the follow-up period, there were no reoperations. Four individuals had a stroke, and three had a myocardial infarction.
MACCE-free survival at 3 and 5 years was 90% and 80%, respectively; 3- and 5-year survival rates were 92% and 85%, respectively. MACCE-free survival was 94% and 79% at 3 and 5 years, respectively, for the chronic CAD group; survival rates were 95% and 86% at the same time points.
Only seven of the 28 deaths recorded throughout the follow-up period were attributable to a heart problem. Figure 2 depicts the Kaplan-Meier survival analysis for the entire study population.
We decided to compare the outcomes of individuals who received the full hybrid procedure to those who did not receive the initially planned PCI. The survival rate was greater in the PCI group, with 95% confidence intervals (CIs) mean survival of 8.4–10.2 vs. 6.8–9.1 years. For the two groups (PCI performed vs. PCI not performed), the log-rank test for the Kaplan-Meier survival analysis was 0.071 (Figure 3).
Discussion
The objective of this retrospective, single-center study was to analyse the characteristics and outcomes of a cohort of 138 patients who underwent minimally invasive off-pump total arterial grafting and were treated with various hybrid revascularization techniques. MACCE, as well as overall survival, were the primary endpoints that were evaluated over the course of 12 years. Despite having a mean SYNTAX Score I in the upper tertile, the patients exhibited a significantly reduced incidence of in-hospital adverse events, surgical complications, and blood transfusions, along with a 30-day mortality rate that was considerably lower than what EuroSCORE had predicted. We performed a second analysis by eliminating patients who received emergency surgery or who had had a myocardial infarction within three months of the procedure and examined their risk profile and postoperative results. This group was later labelled “chronic CAD”, and it included fewer than half of the original cohort, 69 out of 138 people. Baseline characteristics, as well as operative and follow-up outcomes, were not significantly different. However, the overall PCI percentage in this subgroup was just 39.1%. By 3 years, this subgroup had higher rates of survival and MACCE-free-survival, but by 5 years, the rates were almost identical between the total cohort and the chronic CAD group.
Only 70 patients, or 50.7% of the sample, received the targeted PCI treatment, which likely contributed to their reduced survival rate. The main results indicated that patients who underwent complete hybrid revascularization exhibited enhanced survival rates in the intermediate and long-term. This is simultaneously a fundamental finding of our research and one of the limitations that prevents a comprehensive comparison of our results to those of other studies of a similar nature. Concurrently, it is this aspect that enhances the value of this article—notifying the community of the severe repercussions that may ensue from abandoning the initially planned course of treatment.
The study’s biggest drawback is its retrospective nature. Furthermore, the study describes the results of a single centre over a somewhat lengthy period of time; hence, results should be interpreted with caution. The study population was recruited through a process of selection and debate among the Heart-Team. There is no control group in the study. Because only 50.7% of patients received the full hybrid treatment, it is impossible to draw any conclusions about the benefits of HCR. As a result, a bias due to unknown confounding factors must be considered.
As per the guidelines on myocardial revascularization published by the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) in 2018, it is recommended that patients with isolated proximal LAD stenosis undergo a MIDCAB procedure (5). Additionally, in certain cases involving MV CAD, the MIDCAB procedure may be employed as part of a hybrid approach for selected patients (5). The use of HCR is recommended with a Class IIb designation for certain subsets of patients with CAD, but only in medical facilities with a high level of expertise in this procedure (5).
In routine clinical practise, the attending physician makes a decision regarding the most suitable approach for the patient, taking into consideration the risk-benefit ratio. This decision involves evaluating the merits of optimised medicinal therapy, PCI, CABG, or a combination of these interventions. PCI is preferred due to its minimal invasiveness (4), whereas CABG with multiple arterial grafts outperforms PCI in terms of survival rates and survival free of reintervention (1).
In our facility, we have successfully implemented and improved a broad spectrum of minimally invasive cardiac surgery procedures during the past 14 years (6-12). Since 2011, off-pump coronary artery bypass (OPCAB) techniques have been used in over 90% of our coronary bypass surgeries (11). The percentage of minimally invasive coronary bypass surgery accounts for 10% of the annual total volume of CABG procedures. Nonetheless, HCR is also present in our centre, though it only represents a very minor portion of everyday practise.
According to the POLMIDES (HYBRID) study, a prospective randomised trial assigning patients to HCR or CABG in a 1:1 ratio, HCR can be a viable treatment option for certain patients with MV CAD who would otherwise be referred for traditional CABG surgery. With a mean EuroSCORE II of 3.2±2.1, only 17% of trial participants had a EuroSCORE II >6 (13,14).
After conducting a multicenter observational study, the authors concluded that there was no statistically significant distinction in the 1-year and above MACCE rate between patients who received multivessel PCI or HCR (2).
Patients in our study had a higher mean EuroSCORE I additive score of 7.6±10.2. In the three months prior to surgery, 38.4% of them had experienced an acute myocardial infarction. PCI was employed to treat 36.2% of the acute culprit lesions, leaving the remaining vessel(s) to be operated on. There were no conversions to sternotomy or CPB, and transfusion requirements were minimal. Re-exploration for bleeding was more common than expected, accounting for 5.1% of the total research population. Six of the seven patients who needed re-exploration for bleeding underwent a PCI prior to surgery and were operated on while on dual antiplatelet therapy. The length of intensive care stay and hospitalisation were comparable to the HYBRID study data (14).
The 1-, 3-, and 5-year survival rates in our research population were 97%, 92%, and 85%, respectively, while the 5-year MACCE-free survival rate was 80%. The mean survival rate was higher in the patients who received the planned PCI, 8.4–10.2 vs. 6.8–9.1 years. The survival data are comparable to those published by Repossini et al. (15), given that the median EuroSCORE II in their research group was 3.2%. They reported an 86.2%±2.6% 5-year survival rate and an 87.4%±2.4% 5-year MACCE free survival rate. In their evaluation, Modrau et al. reported a 3-year MACCE rate of 31.1% (16).
In their meta-analysis, Panoulas et al. discovered that the majority of HCR patients are male, slightly older than 60, and have a diabetes prevalence of 23–40.7% (17). All of these findings are congruent with our HCR research population, as does the fact that the left ventricular ejection fraction was preserved in the majority of cases (17).
In certain instances of MV CAD, HCR, herein defined as MIDCAB with PCI, has been validated as safe and feasible. A meta-analysis of six observational studies comparing 366 patients undergoing HCR to 824 patients undergoing CABG found that HCR was associated with lower need for blood transfusions, shorter length of stay, and faster return to work, as well as comparable mortality, myocardial infarction, and stroke rates (18). Dixon and colleagues observed similar outcomes in a meta-analysis of 3,399 MV CAD patients, of whom 1,164 were treated with HCR and 2,235 were treated with CABG, including shorter ICU stays and lower blood transfusions for HCR, equivalent additional short term postoperative complications, and similar mid-term survival (19). The HYBRID trial’s 5-year follow-up data revealed that the two groups had comparable rates of all-cause death, myocardial infarction, stroke, and repeat revascularization (13). A recent review of twenty-two studies with a total of 6,981 individuals shown that HCR is a viable option to standard CABG. Both groups had similar short- and long-term outcomes, including mortality, MACCE, and postoperative morbidity, although hybrid techniques were linked with lower perioperative morbidity (20).
Shen et al. (21) observed better MACCE results for HCR patients in the highest EuroSCORE II tertile (>6) in a well-designed retrospective trial comparing HCR with CABG, indicating that high-risk patients would benefit most from an HCR method. A reduced rate of blood transfusion, a shorter hospital stay, and ventilation time were all in favour of HCR in a meta-analysis by Reynolds and King, whereas the CABG group experienced lower hospital expenses (22). The authors came to the conclusion that while HCR is more costly than traditional CABG, it is safe and might have some short-term advantages (22).
Shimamura et al. performed a meta-analysis using Kaplan-Meier derived data compiled from thirteen studies. At a mean follow-up time of 5.1±3.1 years, they discovered that HCR was comparable to CABG in terms of overall mortality, but substantially more prone to MACCE incidence and repeat revascularization. During the mid-term phase (1–5 years), the incidence of MACCE was greater in the HCR cohort; however, it remained comparable throughout the long-term phase (≥5 years) (23).
After a mean follow-up of 8.0±2.6 years, the authors of a recently published propensity score-matched population of 540 simultaneous HCR vs. 540 OPCAB vs. 540 PCI treated between 2007 and 2018 concluded that the cumulative MACCE in the HCR group was comparable to that observed in the OPCAB group, but significantly lower than in the PCI group (24). Furthermore, a subgroup examination of long-term clinical outcomes revealed similar results in patients with varying EuroSCORE II or SYNTAX Score stratifications, as well as individuals with multivessel disease and diabetes (24).
In a recent meta-analysis of 18 trials on MV CAD patients, which involved 2,041 cases of HCR and 2,993 cases of CABG, the authors discovered that the rates of MACCE were comparable in the short, medium (1–5 years), and long-term (>5 years) follow-up periods (25). When comparing the survival rates at the same specific time periods, it was found that the rates were similar for both short- and medium-term follow-up. However, the rates were higher for HCR in the long-term follow-up, with a statistically significant difference (P=0.002) (25). Regrettably, the authors fail to provide any information regarding the demographics or risk scores of the patients involved in the study (25).
Nenna et al. conducted an extensive review that encompassed three randomised trials, ten meta-analyses, and 27 retrospective studies. Their conclusion was that the most significant advantages of HCR, in terms of both adverse events and survival, were observed in patients with a low-to-intermediate risk and less complex coronary anatomy (26).
The use of a new generation of drug-eluting stents and the survival benefit of LITA-LAD grafts are the main benefits of HCR (17). Two large-scale investigations with long-term follow-up established the safety of minimally invasive surgical revascularization in both single VD and selected patients with MV CAD (15,27). In their hands, the surgical treatment was associated with minimal complication rates and favourable long-term results (15,27). Only a few observational reports on a small number of patients treated with HCR described as MICS-CABG plus PCI or ‘advanced hybrid technique’ exist (28,29). The surgical community should prioritise multiple arterial grafts and minimally invasive approaches in order to avoid the morbidity associated with median sternotomy and CPB, given recent findings indicating that drug-eluting stents are comparable to saphenous vein grafts (4), if not superior to them.
Either “the hybrid approach” or “the reversed hybrid approach” was used to treat the patients in our study. Nevertheless, our group’s total PCI percentage was only 50.7%. This could be explained by one of two theories: either the patients did not feel the need to proceed with the planned PCI procedure because they did not experience symptoms of recurrent angina after surgery, or the patients showed up for the planned coronary angiography and the remaining untreated stenosis was not considered severe enough to warrant an intervention based on measurements of the fractional flow reserve (FFR) or instantaneous wave-free ratio (IFR).
Our study population, which included a high proportion of patients who received a reverse hybrid approach, reflects the reality of everyday practice, which is that collaboration between interventional cardiologists and cardiac surgeons needs to improve significantly, and that minimally invasive CABG surgery procedures still account for a small percentage of total CABG surgeries due to limited dissemination. HCR is also not widely used in clinical practice due to a paucity of data in clinical trials involving a great number of individuals with long-term follow-up and diverse HCR operating circumstances (30), despite the fact that recent meta-analyses on a large number of patients show that HCR achieves good short- and long-term outcomes (19,20,23,26,30). As a result, in many cases, the cardiologist will choose PCI treatment first in order to treat the culprit lesion or the lesion that is most likely to cause the most muscle damage if left untreated.
The study’s goal was to reveal the long-term implications of this population treated using different hybrid approaches, as well as to try to identify the critical components required for the success of this evolving strategy. Although interest in HCR has increased, our data indicates that these procedures require extensive planning and patients must be guided and monitored to ensure they complete the intended course of treatment. As a result of these outcomes during the last year in our centre, we were able to optimise the selection process, better structure the course of treatment, and ensure that the targeted hybrid procedure was accomplished.
Foundational pillars of a successful HCR programme include well-functioning Heart-Teams that maintain stability and engage in open and sincere communication with patients when presenting potential treatment options.
Conclusions
Based on our findings, it appears that even patients with higher morbidity scores can undergo HCR with extremely satisfactory mid- and long-term outcomes. Going forward, the organisation of the PCI step following cardiac surgery needs to be the main focus.
Acknowledgments
Certain data were included in a poster presentation entitled “Long-term follow-up of hybrid strategy of total arterial minimally invasive off-pump coronary revascularization and PCI” that was presented during the “Surgical myocardial revascularization” session at the German Cardiology Society’s Annual Meeting in 2023.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://cdt.amegroups.com/article/view/10.21037/cdt-23-413/rc
Data Sharing Statement: Available at https://cdt.amegroups.com/article/view/10.21037/cdt-23-413/dss
Peer Review File: Available at https://cdt.amegroups.com/article/view/10.21037/cdt-23-413/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://cdt.amegroups.com/article/view/10.21037/cdt-23-413/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the ethics board of the Medical University Tübingen (ethics registration No. 777/2021B02) and informed consent was taken from all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Habib RH, Dimitrova KR, Badour SA, et al. CABG Versus PCI: Greater Benefit in Long-Term Outcomes With Multiple Arterial Bypass Grafting. J Am Coll Cardiol 2015;66:1417-27. [Crossref] [PubMed]
- Puskas JD, Halkos ME, DeRose JJ, et al. Hybrid Coronary Revascularization for the Treatment of Multivessel Coronary Artery Disease: A Multicenter Observational Study. J Am Coll Cardiol 2016;68:356-65. [Crossref] [PubMed]
- Ursulescu A, Droc G, Stan A, et al. Minimally Invasive Coronary Artery Bypass Surgery. In: Ţintoiu I, Underwood M, Cook S, et al., editors. Coronary Graft Failure: State of the Art. Springer International Publishing, Switzerland; 2016; Chapter 7: 53-64.
- Van Praet KM, Kofler M, Shafti TZN, et al. Minimally Invasive Coronary Revascularisation Surgery: A Focused Review of the Available Literature. Interv Cardiol 2021;16:e08. [Crossref] [PubMed]
- Neumann FJ, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J 2019;40:87-165. Erratum in: Eur Heart J 2019;40:3096. [Crossref] [PubMed]
- Franke UF, Ursulescu A, Göbel N, et al. Results and Quality of Life after Minimally Invasive Ross Procedure. J Heart Valve Dis 2015;24:295-301. [PubMed]
- Franke UF, Albert M, Rustenbach C, et al. Minimally invasive Ross procedure through partial upper sternotomy. Interact Cardiovasc Thorac Surg 2009;9:545-6. [Crossref] [PubMed]
- Wachter K, Franke UF, Yadav R, et al. Feasibility and clinical outcome after minimally invasive valve-sparing aortic root replacement. Interact Cardiovasc Thorac Surg 2017;24:377-83. [PubMed]
- Baumbach H, Rustenbach CJ, Ahad S, et al. Minimally Invasive Extracorporeal Bypass in Minimally Invasive Heart Valve Operations: A Prospective Randomized Trial. Ann Thorac Surg 2016;102:93-100. [Crossref] [PubMed]
- Goebel N, Bonte D, Salehi-Gilani S, et al. Minimally Invasive Access Aortic Arch Surgery. Innovations (Phila) 2017;12:351-5. [Crossref] [PubMed]
- Rufa MI, Ursulescu A, Nagib R, et al. Off-pump versus on-pump redo coronary artery bypass grafting: A propensity score analysis of long-term follow-up. J Thorac Cardiovasc Surg 2020;159:447-456.e2. [Crossref] [PubMed]
- Rufa MI, Ursulescu A, Aktuerk D, et al. Minimally invasive strategies of surgical coronary artery revascularization for the aging population. J Cardiovasc Surg (Torino) 2023;64:534-40. [Crossref] [PubMed]
- Tajstra M, Hrapkowicz T, Hawranek M, et al. Hybrid Coronary Revascularization in Selected Patients With Multivessel Disease: 5-Year Clinical Outcomes of the Prospective Randomized Pilot Study. JACC Cardiovasc Interv 2018;11:847-52. [Crossref] [PubMed]
- Gąsior M, Zembala MO, Tajstra M, et al. Hybrid revascularization for multivessel coronary artery disease. JACC Cardiovasc Interv 2014;7:1277-83. [Crossref] [PubMed]
- Repossini A, Di Bacco L, Nicoli F, et al. Minimally invasive coronary artery bypass: Twenty-year experience. J Thorac Cardiovasc Surg 2019;158:127-138.e1. [Crossref] [PubMed]
- Modrau IS, Nielsen PH, Nielsen DV, et al. Outcome of hybrid compared to conventional revascularization in multivessel coronary artery disease. Scand Cardiovasc J 2020;54:376-82. [Crossref] [PubMed]
- Panoulas VF, Colombo A, Margonato A, et al. Hybrid coronary revascularization: promising, but yet to take off. J Am Coll Cardiol 2015;65:85-97. [Crossref] [PubMed]
- Harskamp RE, Bagai A, Halkos ME, et al. Clinical outcomes after hybrid coronary revascularization versus coronary artery bypass surgery: a meta-analysis of 1,190 patients. Am Heart J 2014;167:585-92. [Crossref] [PubMed]
- Dixon LK, Akberali U, Di Tommaso E, et al. Hybrid coronary revascularization versus coronary artery bypass grafting for multivessel coronary artery disease: A systematic review and meta-analysis. Int J Cardiol 2022;359:20-7. [Crossref] [PubMed]
- Hinojosa-Gonzalez DE, Bueno-Gutierrez LC, Salan-Gomez M, et al. Hybrid revascularization vs. coronary bypass for coronary artery disease: a systematic review and meta-analysis. J Cardiovasc Surg (Torino) 2022;63:353-68. [Crossref] [PubMed]
- Shen L, Hu S, Wang H, et al. One-stop hybrid coronary revascularization versus coronary artery bypass grafting and percutaneous coronary intervention for the treatment of multivessel coronary artery disease: 3-year follow-up results from a single institution. J Am Coll Cardiol 2013;61:2525-33. [Crossref] [PubMed]
- Reynolds AC, King N. Hybrid coronary revascularization versus conventional coronary artery bypass grafting: Systematic review and meta-analysis. Medicine (Baltimore) 2018;97:e11941. [Crossref] [PubMed]
- Shimamura J, Miyamoto Y, Hibino M, et al. Long-Term Outcomes After Hybrid Coronary Revascularization Versus Coronary Artery Bypass Grafting: Meta-Analysis of Kaplan-Meier-Derived Data. Am J Cardiol 2024;212:13-22. [Crossref] [PubMed]
- Ding T, Yuan X, Chen K, et al. Simultaneous Hybrid Coronary Revascularization vs Conventional Strategies for Multivessel Coronary Artery Disease: A 10-Year Follow-Up. JACC Cardiovasc Interv 2023;16:50-60. [Crossref] [PubMed]
- Yu L, Zhu K, Du N, et al. Comparison of hybrid coronary revascularization versus coronary artery bypass grafting in patients with multivessel coronary artery disease: a meta-analysis. J Cardiothorac Surg 2022;17:147. [Crossref] [PubMed]
- Nenna A, Nappi F, Spadaccio C, et al. Hybrid coronary revascularization in multivessel coronary artery disease: a systematic review. Future Cardiol 2022;18:219-34. [Crossref] [PubMed]
- Holzhey DM, Jacobs S, Mochalski M, et al. Seven-year follow-up after minimally invasive direct coronary artery bypass: experience with more than 1300 patients. Ann Thorac Surg 2007;83:108-14. [Crossref] [PubMed]
- Kitahara H, Hirai T, McCrorey M, et al. Hybrid coronary revascularization: Midterm outcomes of robotic multivessel bypass and percutaneous interventions. J Thorac Cardiovasc Surg 2019;157:1829-1836.e1. [Crossref] [PubMed]
- Bonaros N, Schachner T, Kofler M, et al. Advanced hybrid closed chest revascularization: an innovative strategy for the treatment of multivessel coronary artery disease. Eur J Cardiothorac Surg 2014;46:e94-e102. [Crossref] [PubMed]
- Harskamp RE, Brennan JM, Xian Y, et al. Practice patterns and clinical outcomes after hybrid coronary revascularization in the United States: an analysis from the society of thoracic surgeons adult cardiac database. Circulation 2014;130:872-9. [Crossref] [PubMed]


