
Impact of surgical aortic valve replacement volume on tamponade after transcatheter aortic valve replacement
Transcatheter aortic valve replacement (TAVR) is the standard of care for patients with severe symptomatic aortic stenosis carrying a high surgical risk (1). Cardiac tamponade is a rare but life-threatening complication witnessed after TAVR. The results of cardiovascular therapies are significantly influenced by institutional experience. We opted for surgical aortic valve replacement (SAVR) volumes for two main reasons. Firstly, it provides a viable treatment avenue for patients diagnosed with aortic stenosis, supported by a robust multidisciplinary team. Secondly, it allows us to effectively manage potential complications necessitating surgical intervention. Cardiac tamponade is one such complication that may require surgical expertise. Therefore, we aimed to investigate the impact of SAVR volumes on the incidence and outcomes of patients who experienced tamponade following TAVR.
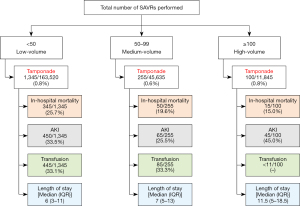
We utilized the National Inpatient Sample (NIS) database 2016–2019 to identify all patients who underwent TAVR using the International Classification of Diseases, 10th revision code (ICD-10 CM) 02RF3 (2). The cohort was stratified based on institutional SAVR volumes into low-volume (<50), medium-volume (50–99), and high-volume (≥100) SAVR centers. We examined the incidence of developing post-TAVR tamponade (ICD-10 CM code, I314) based on SAVR hospital volumes. Among patients who developed tamponade, further analysis was conducted to check the association of SAVR hospital volume to in-hospital outcomes of patients. Outcomes were compared using the Pearson chi-square test for categorical variables and independent-samples t-test for continuous variables. Statistical analysis was SPSS version 27, and a P value of <0.05 was considered statistically significant. The study was exempt from the institutional review board approval as the NIS is a publicly available de-identified database.
Between 2016–2019, a total of 221,000 weighted TAVR hospitalizations were identified. The incidence of tamponade was lowest in medium SAVR volume hospitals as compared to low and high SAVR volume hospitals (0.6% vs. 0.8% vs. 0.8%, P<0.001) (Figure 1). The female gender was more likely to develop tamponade (66.2% vs. 45.3%, P<0.01). Additionally, White race was associated with a higher likelihood of occurrence of post-TAVR tamponade (89.6% vs. 87%, P<0.01). Advanced age [odds ratio (OR): 1.04, 95% confidence interval (CI): 1.03–1.04], female sex (OR: 2.20, 95% CI: 1.98–2.45), peripheral vascular disease (OR: 1.23, 95% CI: 1.10–1.39), and atrial fibrillation (OR: 1.29, 95% CI: 1.16–1.42) were significantly associated with higher risk of cardiac tamponade (P<0.01). The in-hospital mortality associated with post-TAVR cardiac tamponade was significantly less in the high-SAVR volume centers (15%) as compared to low- (25.7%) and medium-SAVR volume institutions (19.6%) (P=0.01). Similarly, the need for red blood cell transfusion was considerably lower in high SAVR volume hospitals in contrast to low (33.1%) and medium (33.3%) SAVR volume institutions (P<0.001). Acute kidney injury (AKI) (45.0%) and the median length of stay [11.5 days, interquartile range (IQR), 5–18.5 days] were highest in the high SAVR volume centers as compared to low and medium volume hospitals (P<0.001). Our multivariable regression model was adjusted for age, race, sex, hospital location, hospital region, hospital teaching status, hypertension, hyperlipidemia, diabetes (with and without chronic complications), chronic pulmonary disease, smoking, obesity, peripheral vascular diseases, chronic heart failure, history of stroke, atrial fibrillation, coronary artery disease, alcohol abuse, solid tumor without metastasis, and elective status of the procedure.
Our findings demonstrate that high SAVR volume hospitals exhibited significantly lower in-hospital mortality associated with post-TAVR tamponade. The lower mortality can be attributed to more expertise in high SAVR volume centers where there is an effective and timely intervention for the management of complications, leading to better patient outcomes (3). High surgical volume may also provide better resuscitation technologies like easy availability of cardiopulmonary bypass, rapid transfusion capabilities, perfusionist, etc. This, in turn, reduces the need for red blood cell transfusion in high SAVR volume centers because the familiarity with complex aortic valve interventions may allow for prompt identification and response to tamponade management. The higher incidence of AKI and tamponade in higher-volume centers may be attributed to their propensity to attract more complex cases, thereby increasing the likelihood of complications. Patient-specific factors, such as higher comorbidities or anatomical variations, may influence the likelihood of developing complications and could override any potential volume-outcome relationship. Additionally, variability in surgical techniques and postoperative management across different centers may impact the occurrence of complications.
One of the major limitations of our study is that NIS lacks granular data like procedural or imaging information, which limits us from identifying the exact reasons for tamponade following TAVR. Being an administrative database, NIS relies on ICD-10 codes, which are deemed less effective as compared to the manual chart review. However, it has found extensive utilization in medical research and is considered dependable when subjected to appropriate analytical methods.
The mortality related to cardiac tamponade post-TAVR is lowest in high SAVR volume centers. Effective protocols for managing cardiac tamponade in low- and medium-volume centers should be employed to bridge the outcome gap in patient care. Diagnosing and managing cardiac tamponade after TAVR demands heightened clinical awareness and a comprehensive approach to avoid potential pitfalls. Given the diversity of symptoms and the possibility of overlapping clinical presentations with other post-TAVR complications, clinicians must maintain a high index of suspicion. Timely recognition is paramount, as diagnostic delays can lead to rapid hemodynamic deterioration. Furthermore, the interpretation of diagnostic imaging, particularly echocardiography, can be challenging due to artifacts and anatomical complexities post-TAVR, necessitating meticulous evaluation by experienced operators. Treatment decisions, including pericardiocentesis or surgical intervention, should be guided by individual patient factors, hemodynamic stability, and procedural considerations. Collaborative teamwork among interventionalists, imaging specialists, and intensivists is imperative to navigate these complexities effectively and ensure optimal patient outcomes in the management of post-TAVR cardiac tamponade.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was a standard submission to the journal. The article has undergone external peer review.
Peer Review File: Available at https://cdt.amegroups.com/article/view/10.21037/cdt-23-467/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://cdt.amegroups.com/article/view/10.21037/cdt-23-467/coif). The authors have no conflict of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was exempt from the institutional review board approval as the NIS is a publicly available de-identified database. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2021;143:e72-227. [PubMed]
- HCUP-US NIS Overview [Internet]. [cited 2022 Oct 13]. Available online: https://www.hcup-us.ahrq.gov/nisoverview.jsp#about
- Hirji SA, McCarthy E, Kim D, et al. Relationship Between Hospital Surgical Aortic Valve Replacement Volume and Transcatheter Aortic Valve Replacement Outcomes. JACC Cardiovasc Interv 2020;13:335-43. [Crossref] [PubMed]


