
Intra- and interobserver reliability in measuring aortic root rotation with cardiac magnetic resonance imaging
Highlight box
Key findings
• This study found that cardiac magnetic resonance imaging is a valuable non-invasive imaging tool that allows to quantify aortic root (AoR) rotation angles with an excellent intra- and interobserver reliability.
What is known and what is new?
• AoR rotation is associated with a variation of myocardial support of the aortic valvar sinuses and the position of the atrioventricular bundle.
• The role of AoR rotation in aortic disease is not fully understood, but variations in AoR anatomy with the constant exposure to high pulsatile pressure may have an impact on the blood flow patterns and wall shear stress in the thoracic aorta.
What is the implication, and what should change now?
• A detailed understanding of AoR rotation could assist in daily clinical practice for executing safe and precise procedures of the AoR.
• Furthermore, this understanding could contribute to a more comprehensive insight into the risk profiles of patients with various aortic pathologies.
Introduction
The aortic root (AoR) is defined as the most proximal segment of the aorta, located between the left ventricular outflow tract and the tubular ascending aorta (1,2). The complex structure of the AoR supports the leaflets of the aortic valve and acts as an individual hemodynamic system (3,4). Due to the constant exposure to high pulsatile pressure, small variations in AoR anatomy may have a major impact on the blood flow patterns and wall shear stress in the thoracic aorta (5,6). In particular, certain rotational positions of the AoR have been associated with an increased dissection risk of the ascending aorta (7).
Several cardiac imaging techniques have previously been used to analyze the spatial position and rotation of the AoR (7-19). An echocardiographic study assessed the AoR rotation with various measurements and found a significant clockwise rotation in children with Tetralogy of Fallot (8). Other studies recently used a similar approach with multi-detector computed tomography to identify variation in the rotation of the AoR in the general population (9-11). While echocardiography and computed tomography have previously been used for the assessment of AoR rotation, a recent study utilized a previously validated method with computed tomography to quantify neo-AoR rotation following the arterial switch operation for transposition of the great arteries with cardiac magnetic resonance (CMR) (15). CMR has the potential to better visualize and quantify AoR rotation while avoiding X-ray related hazards. However, the CMR-based examination of AoR rotation has not yet been tested in a consecutive group of healthy subjects, and the reliability of such measurements is unknown.
In the present study, we used a CMR-based approach to measure AoR rotation angles in consecutive healthy subjects undergoing routine clinical CMR imaging, and we assessed the intra- and interobserver reliability of these measurements. In addition to the angles of all three aortic sinuses, we assessed the reliability of measuring the angle between the interatrial septum (IAS) and the posterior atrial wall which serves as a key anatomical landmark for this approach.
Methods
Study population and data collection
The electronic medical record database of Medisch Spectrum Twente was used to identify a random selection of 50 consecutive healthy subjects who underwent routine CMR imaging between January 2021 and April 2021. Anonymized data were collected about patient demographics and imaging characteristics.
CMR technique and imaging analysis
The CMR images were acquired by a 1.5 Tesla magnetic resonance scanner (Ingenia Ambition, Philips Medical Systems Best, The Netherlands). The routine scanner protocol included velocity-encoded cine gradient echo imaging: a slice thickness of 8 mm, a spatial resolution of 1.2 mm × 1.2 mm, a temporal resolution of 26 ms, velocity encoding at 200 cm/s, and 30 cardiac phases throughout the cardiac cycle. Images were acquired during breath-hold at expiration. All CMR images were reviewed on dedicated post-processing software (Philips Intellispace Portal 10.0; Philips Healthcare, Best, The Netherlands) that allowed geometric measurements and calculations.
Measurements of AoR rotation angles
AoR rotation angles were measured in the short-axis view at the level of the aortic valve in diastolic phase (Figure 1). We used a similar approach to measure AoR rotation as previously described by Isaaz et al. for an echocardiographic approach (8). We hypothesized that the IAS could be considered as key anatomical landmark or reference line to assess AoR rotation with CMR. To evaluate this hypothesis, we assessed the reliability of the IAS angle, the angle between the axis of the IAS and the posterior atrial wall (Figure 1). Due to the variable curvature of the middle part of IAS, the axis of IAS was determined by considering its anterior and posterior insertions, representing the muscular buttress and the posterior interatrial infolding (16,20,21).
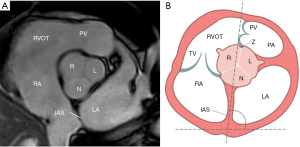
Figure 2 shows a schematic representation of the short-axis plane at aortic valve level with the construction of different lines for measuring the angles of the non-coronary sinus (NCS), right coronary sinus (RCS), and left coronary sinus (LCS) relative to the IAS. (I) The axis of the NCS was a line between mid-point of NCS and the commissure between the RCS and LCS; (II) the axis of the RCS was a line between mid-point of RCS and the commissure between the LCS and NCS; and (III) the axis of the LCS was a line between mid-point of LCS and the commissure between NCS and RCS.

Inter- and intraobserver variability
To assess the interobserver agreement in measuring AoR rotation, three independent analysts (M.V., W.F., J.v.E.) performed all geometric measurements. The first analyst (M.V.) was initially trained by a clinician (J.v.E) with more than 10 years of experience in CMR. The third observer (W.F.) was trained in the assessment of AoR rotation by the first observer (M.V.) by examining ten CMR images together. To asses intraobserver agreement repeated measurements were performed (M.V.) after a time interval of at least 3 weeks, for which the image sets were presented again in a random order.
Statistical analysis
Baseline characteristics were described by mean ± standard deviation (SD). Inter- and intraobserver reliability were analyzed using intraclass correlation coefficients (ICCs). The ICC is expressed as a value between 0 and 1. Values below 0.5 are indicative of poor reliability, values between 0.5 and 0.75 indicate moderate reliability, values between 0.75 and 0.9 indicate good reliability, and values greater than 0.90 indicate excellent reliability (22). Statistical analyses were performed using SPSS®, version 24 (IBM, Armonk, NY, USA).
Ethical statement
The single-center study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and was approved by the institutional ethical review board of Medisch Spectrum Twente (No. K21-22), which classified it as research that does not falls under the Dutch ‘Medical Research Involving Human Subjects Act’. As a consequence, the institutional ethical review board formally waved the requirement for obtaining a written informed consent from each individual patient.
Results
Of all 50 CMR images, 47 (94%) images from 47 subjects had a sufficient image quality, showed detectable structures, and were therefore considered suitable for analysis. A total of 3 (6%) images were excluded due to poor visualization of the anatomical landmarks as a result of arrhythmias or voluntary motion artefacts. Study subjects were 55.9±18.2 years old, and 23 (48.9%) were female. CMR measurements, calculated as a mean value for each of the four angles, are presented in Table 1. The IAS angle (i.e., the left inclination of the IAS) was 79.2°±8.9°. NCS, RCS, and LCS angles measured 25.9°±12.9°, 37.5°±15.2°, and 97.0°±13.1°, respectively.
Table 1
| Angle | T1.1 | T1.2 | T2 | T3 | All four measurements |
|---|---|---|---|---|---|
| IAS (°) | 80.7±9.7 | 79.6±9.7 | 77.3±9.9 | 79.4±9.4 | 79.2±8.9 |
| NCS (°) | 26.2±15.0 | 24.8±11.7 | 24.5±14.1 | 27.4±14.1 | 25.9±12.9 |
| RCS (°) | 35.3±15.7 | 36.9±14.4 | 39.1±15.7 | 37.4±17.2 | 37.5±15.2 |
| LCS (°) | 96.0±14.9 | 97.0±14.1 | 98.3±15.0 | 98.3±15.3 | 97.0±13.1 |
Data are presented as mean ± SD. IAS, interatrial septum; NCS, non-coronary sinus; RCS, right coronary sinus; LCS, left coronary sinus; SD, standard deviation.
The results of the intra- and interobserver reliability of CMR measurements are shown in Tables 2,3. For the interobserver agreement, ICCs were consistently high for all angles with excellent values (ICC for NCS, RCS, and LCS angles 0.90, 0.86, and 0.87, respectively). The intraobserver agreement of the IAS angle measurement [ICC =0.94, 95% confidence interval (CI): 0.88–0.96] was slightly higher than the interobserver agreement (ICC =0.76, 95% CI: 0.63–0.85). The intraobserver reliability of CMR measurements showed excellent agreement with ICC values ranging from 0.91 to 0.94 for the three angles.
Table 2
| Angle | ICC | 95% CI | |
|---|---|---|---|
| Lower bound | Upper bound | ||
| IAS | 0.76 | 0.63 | 0.85 |
| NCS | 0.90 | 0.84 | 0.94 |
| RCS | 0.86 | 0.77 | 0.92 |
| LCS | 0.87 | 0.80 | 0.92 |
AoR, aortic root; ICC, intraclass correlation coefficient; CI, confidence interval; IAS, interatrial septum; NCS, non-coronary sinus; RCS, right coronary sinus; LCS, left coronary sinus.
Table 3
| Measure | ICC | 95% CI | |
|---|---|---|---|
| Lower bound | Upper bound | ||
| Angle IAS | 0.94 | 0.88 | 0.96 |
| Angle NCS | 0.94 | 0.88 | 0.96 |
| Angle RCS | 0.93 | 0.87 | 0.96 |
| Angle LCS | 0.91 | 0.84 | 0.95 |
AoR, aortic root; ICC, intraclass correlation coefficient; CI, confidence interval; IAS, interatrial septum; NCS, non-coronary sinus; RCS, right coronary sinus; LCS, left coronary sinus.
Discussion
Main findings
The present study evaluates the reliability of a CMR-based approach for AoR rotation measurements. In 47 healthy subjects, we found that CMR imaging is a valuable non-invasive imaging tool that allows to quantify AoR rotation angles with an excellent intra- and interobserver reliability. In addition, the current study shows that the IAS can serve as a reliable reference line to assess AoR rotation with CRM in human in vivo.
Previous studies
AoR rotation has been assessed with echocardiographic and radiographic imaging, but there is a lack of analysis of reliability of these measurements. To our knowledge, the echocardiographic study by Isaaz et al. was the first to non-invasively measure AoR rotation angles with a cardiac imaging modality (8). Although a comprehensive method was described with various geometric measurements and calculations, a formal statistical analysis of measurement reliability was not performed. Yet, the authors compared the results of two observers and found that the measurements did not differ by more than 5%. The study found a relevant clockwise rotation in 22 children with Tetralogy of Fallot (59.2°±10.7°) as compared to 23 normal subjects (23.4°±8.3°) (8). In our present study with CMR, we found not only similar rotation angles in healthy subjects, but our CMR measurements of the angle of the IAS (79.2°±8.9°) also corroborated echocardiographic data (86°±6.1°) (8).
By contrast, more recently published studies that evaluated AoR rotation with computed tomography, found smaller AoR rotation angles in healthy subjects (7,9). Computed tomography-based analyses, performed by Moradi et al. (7) and Saremi et al. (9), found in healthy subjects mean rotation angles of 15.7°±10.7° and 13.8° (range, −21° to 58°), respectively. These computed tomography studies used a methodological approach that was similar to the echocardiography-based approach suggested by Isaaz and coworkers (8). Yet, Moradi and coworkers did not report a reliability assessment, and all measurements were performed by a single radiologist (7). Saremi and coworkers stated that their analysts had an excellent interobserver agreement for several aortic measurements (ICCs =0.81–0.89), but intra- and interobserver agreement specifically of measuring AoR rotation measurements was not reported (9).
To the best of our knowledge, so far only one study has reported details on both the intra- and interobserver agreement of measuring AoR rotation with a cardiac imaging modality (11). Romeih et al. assessed the AoR rotation with multi-slice computer tomography angiography in 287 patients with Tetralogy of Fallot, demonstrating a clockwise rotation of the AoR that varied from 52.6° to −64.9°, with an excellent inter- and intraobserver agreement (ICC between 0.90 and 0.91) between two independent analysts in a random sample of 100 patients (11).
Theoretically, the measurement discrepancies found between imaging modalities might be related to the visualization of the AoR and landmark structures (e.g., the IAS). Yet, with the high spatial resolution of modern computed tomography and CMR, one might expect a similarly detailed, accurate assessment of anatomical landmarks and, hence, similar findings with both imaging modalities. As the accuracy of AoR rotation measurement has not been examined yet by comparing data obtained from different imaging modalities, we can only speculate that the exact assessment of landmark structures may be crucial.
Despite appearing as a straight forward structure in conventional two-dimensional images, the atrial septum is remarkably complex, posing a challenge for accurate interpretation as a landmark structure (16). In our study, we established the IAS axis by utilizing the anterior and posterior insertions, which represent the muscular buttress and the posterior interatrial infolding. In contrast, Tretter et al. used a different anatomical landmark for the atrial septum—namely, the long axis of the triangular structure composed of the right fibrous trigone and muscular buttress (10). This methodological distinction may contribute to the observed variation in rotation, as this CT study reports in 78 patients a lower AoR rotation angle of 15.5° (range, −32° to 44.7°). It is crucial to note, that the intra- and interobserver reliability for the measurements undertaken with this approach were lower than in our study (ICC =0.71 and 0.64, respectively) (10).
Clinical and research implications
The role of AoR rotation in aortic disease is not fully understood, but variations in AoR anatomy with the constant exposure to high pulsatile pressure may have an impact on the blood flow patterns and wall shear stress in the thoracic aorta (4-6). Increased clockwise rotation of the AoR may not only be linked to aortic dilatation and an increased risk of aortic dissection, but a recent study has also shown that the neo-AoR rotational angle correlates with aortic dilation and neo-aortic valve incompetence in patients after arterial switch operation for transposition of the great arteries (7,9,15). Our findings show that CMR-based measurement allow to perform reliable measurements of AoR rotation, and could assist in better understanding the risk profiles of patients with abnormal AoR rotation or other aortic pathologies. Furthermore, as AoR rotation is associated with a variation of myocardial support of the aortic valvar sinuses and the position of the atrioventricular bundle, a detailed understanding of AoR rotation could assist both surgeons and interventionists in executing safe and precise procedures involving the AoR (10,17,19).
Our present study, which is the first to compare rotation angle measurements of all three aortic sinuses for defining AoR rotation, showed no advantage in measurement agreement for one of these cardiac structures over the other. As a consequence, in future studies it will be acceptable and would be most practical to define AoR rotation based on the measurement of a single angle.
Limitations
This study has some limitations. The study population did not have a particularly large sample size, yet we feel that it was sufficient for demonstrating the validity of the novel CMR-based method. In addition, the analysis of CMR images requires some interpretation, and findings may to some extent depend on the experience of the analyst. We found an excellent intraobserver reliability of measurements performed by one analyst, even after limited training, but we cannot exclude that there may be some variance in intraobserver reliability when comparing either very experienced or less experienced analysts. Furthermore, while (in our experience) the short-axis AoR cine stack with a balanced turbo-field-echo sequence provides an ideal image view with good visualization of all structures of interest, 6% of the images showed a poor visualization of the anatomical landmarks due to arrhythmias and voluntary motion artefacts and had to be excluded. Moreover, we did not utilize multiplanar reformatting of the short-axis of the AoR. This may result in a certain loss of accuracy, potentially causing the measured angles to be reliable but not necessarily confirming that the rotation angles align with previous studies which have employed this method (10,15-19).
We wish to emphasize that our study’s measurements were conducted on a consecutive series of healthy subjects with no anatomical anomalies. In these instances, the intra-atrial septum proves to be a reliable reference point. However, acknowledging that with this methodical approach, aortic rotation may be influenced by variations in the anatomy of the atrial septum, especially in situations involving altered anatomy such as congenital abnormalities or conditions like atrial dilation, we propose a vigilant approach to monitor potential variations in the reference point. This can be accomplished, for example, by measuring the angle IAS.
Conclusions
The present study in healthy subjects reports a CMR-based approach for measuring AoR rotation. It was shown that CMR allows to quantify the AoR rotation angle with excellent intra- and interobserver agreement.
Acknowledgments
Funding: None.
Footnote
Data Sharing Statement: Available at https://cdt.amegroups.com/article/view/10.21037/cdt-23-384/dss
Peer Review File: Available at https://cdt.amegroups.com/article/view/10.21037/cdt-23-384/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://cdt.amegroups.com/article/view/10.21037/cdt-23-384/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The single-center study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and was approved by the institutional ethical review board of Medisch Spectrum Twente (No. K21-22), which classified it as research that does not falls under the Dutch ‘Medical Research Involving Human Subjects Act’. As a consequence, the institutional ethical review board formally waved the requirement for obtaining a written informed consent from each individual patient.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Anderson RH. Clinical anatomy of the aortic root. Heart 2000;84:670-3. [Crossref] [PubMed]
- Ho SY. Structure and anatomy of the aortic root. Eur J Echocardiogr 2009;10:i3-10. [Crossref] [PubMed]
- Plonek T, Berezowski M, Bochenek M, et al. A comparison of aortic root measurements by echocardiography and computed tomography. J Thorac Cardiovasc Surg 2019;157:479-86. [Crossref] [PubMed]
- Ha H, Kim GB, Kweon J, et al. The influence of the aortic valve angle on the hemodynamic features of the thoracic aorta. Sci Rep 2016;6:32316. [Crossref] [PubMed]
- Meierhofer C, Schneider EP, Lyko C, et al. Wall shear stress and flow patterns in the ascending aorta in patients with bicuspid aortic valves differ significantly from tricuspid aortic valves: a prospective study. Eur Heart J Cardiovasc Imaging 2013;14:797-804. [Crossref] [PubMed]
- Sundström E, Jonnagiri R, Gutmark-Little I, et al. Effects of Normal Variation in the Rotational Position of the Aortic Root on Hemodynamics and Tissue Biomechanics of the Thoracic Aorta. Cardiovasc Eng Technol 2020;11:47-58. [Crossref] [PubMed]
- Moradi M, Mirfasihi RS. Is there any association between aortic root rotation angle and aortic dissection? Indian J Thorac Cardiovasc Surg 2020;36:181-5. [Crossref] [PubMed]
- Isaaz K, Cloez JL, Marçon F, et al. Is the aorta truly dextroposed in tetralogy of Fallot? A two-dimensional echocardiographic answer. Circulation 1986;73:892-9. [Crossref] [PubMed]
- Saremi F, Cen S, Tayari N, et al. A correlative study of aortic valve rotation angle and thoracic aortic sizes using ECG gated CT angiography. Eur J Radiol 2017;89:60-6. [Crossref] [PubMed]
- Tretter JT, Mori S, Saremi F, et al. Variations in rotation of the aortic root and membranous septum with implications for transcatheter valve implantation. Heart 2018;104:999-1005. [Crossref] [PubMed]
- Romeih S, Kaoud A, Hashem M, et al. A quantitative assessment of aorta root rotation in patients with tetralogy of Fallot evaluated by MSCT. Sci Rep 2021;11:14336. [Crossref] [PubMed]
- Amofa D, Mori S, Toh H, et al. The rotational position of the aortic root related to its underlying ventricular support. Clin Anat 2019;32:1107-17. [Crossref] [PubMed]
- Powell SK, Almeneisi H, Alsaied T, et al. Rotational Position of the Aortic Root is Associated with Increased Aortic Dimensions in Marfan and Loeys-Dietz Syndrome. Pediatr Cardiol 2021;42:1157-61. [Crossref] [PubMed]
- Chiu IS, Wu CS, Wang JK, et al. Influence of aortopulmonary rotation on the anomalous coronary artery pattern in tetralogy of fallot. Am J Cardiol 2000;85:780-4, A9.
- Tseng SY, Tretter JT, Gao Z, et al. Aortic root rotational position associates with aortic valvar incompetence and aortic dilation after arterial switch operation for transposition of the great arteries. Int J Cardiovasc Imaging 2023;39:1013-21. [Crossref] [PubMed]
- Mori S, Nishii T, Tretter JT, et al. Demonstration of living anatomy clarifies the morphology of interatrial communications. Heart 2018;104:2003-9. [Crossref] [PubMed]
- Toh H, Mori S, Tretter JT, et al. Living Anatomy of the Ventricular Myocardial Crescents Supporting the Coronary Aortic Sinuses. Semin Thorac Cardiovasc Surg 2020;32:230-41. [Crossref] [PubMed]
- Tretter JT, Spicer DE, Macías Y, et al. Vulnerability of the ventricular conduction axis during transcatheter aortic valvar implantation: A translational pathologic study. Clin Anat 2023;36:836-46. [Crossref] [PubMed]
- Oishi K, Arai H, Oi K, et al. The rotational position of the aortic valve: implications for valve-sparing aortic root replacement. Eur J Cardiothorac Surg 2022;62:ezac179. Erratum in: Eur J Cardiothorac Surg 2022. [Crossref] [PubMed]
- Elagha A, Othman Y, Darweesh R, et al. Characterization of the interatrial septum by high-field cardiac MRI: a comparison with multi-slice computed tomography. Egypt Heart J 2020;72:81. [Crossref] [PubMed]
- Fender EA, Sibley CT, Nazarian S, et al. Atrial septal angulation varies widely in patients undergoing pulmonary vein isolation. J Invasive Cardiol 2014;26:128-31. [PubMed]
- Koo TK, Li MY. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J Chiropr Med 2016;15:155-63. Erratum in: J Chiropr Med 2017;16:346. [Crossref] [PubMed]


