
The effect of aortic morphology on perioperative rupture of abdominal aortic aneurysm—a retrospective cohort study
Highlight box
Key findings
• Our research confirmed a significant correlation between the extent of proximal neck angulation and the risk of perioperative rupture in abdominal aortic aneurysms. Notably, this angulation varies considerably between genders, with females displaying greater angulation than males.
What is known and what is new?
• It is well-established that abdominal aortic aneurysms exceeding 5cm in diameter, especially those with complex neck anatomy, face a rapidly increasing risk of rupture.
• Our study specifically addressed the perioperative rupture risk associated with these aneurysms, introducing new insights into the gender disparities in rupture risks, emphasizing the heightened vulnerability among females.
What is the implication, and what should change now?
• Clinicians should rigorously evaluate proximal neck angulation in patients scheduled for endovascular aneurysm repair, prioritizing early intervention for those with severe angulation to reduce rupture risks. Alternatively, for abdominal aortic aneurysms with severely angulated neck that is outside the Instructions for Use, open repair should be considered instead.
• Additionally, the observed gender differences in aneurysm rupture underscore the need for enhanced focus on and management of abdominal aortic aneurysms in female patients.
• The predictive model developed in this study requires validation with multi-center data to ensure its applicability and accuracy across broader populations.
Introduction
Abdominal aortic aneurysms (AAAs) are often asymptomatic with slow expansion until rupture. If left untreated, AAAs can grow and rupture, leading to death in 80% of patients (1-5). In recent years, studies (6-13) have been carried out on the effects of morphology on the mortality, re-intervention rate and postoperative complications of endovascular aneurysm repair (EVAR) for AAA. While previous studies have highlighted high postoperative mortality and endoleak rates often identified during follow-up, the influence of proximal aneurysm neck angulation on these outcomes remains underexplored (14,15). This oversight emphasizes the need for focused management of perioperative risks associated with AAAs. This study investigates the impact of increased angulation at the proximal aneurysm neck on the incidence of perioperative ruptures. Additionally, it elucidates the correlation between the degree of neck angulation and the risk of perioperative rupture, providing crucial insights into potential preventive strategies. We present this article in accordance with the STROBE reporting checklist (available at https://cdt.amegroups.com/article/view/10.21037/cdt-24-210/rc).
Methods
Study population
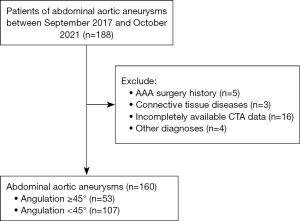
This is a retrospective cohort study. Patients with a proven AAA were identified retrospectively based on the interventional therapy in multiple medical centers (including Shandong Provincial Hospital Affiliated to Shandong First Medical University, Affiliated Suzhou Hospital of Nanjing Medical University and Tangshan Workers Hospital) for cardiovascular disease in China. Patients were included for this analysis if the AAAs had been treated by means of EVAR between September 2017 and October 2021. We reviewed 188 consecutive patients; after excluding 3 with connective tissue disease, 5 with a history of AAA surgery, and 4 without AAAs, as well as 16 lacking computed tomography angiography (CTA) data, 160 patients were ultimately included in the study (Figure 1). Rupture of AAAs was defined as bleeding outside the adventitia of a dilated aortic wall. Inclusion criteria: (I) diagnosed with AAA via CTA; (II) proximal aneurysm neck greater than 10 mm and diameter greater than 5 cm. Exclusion criteria: (I) patients with pararenal, suprarenal, and type IV thoracoabdominal aneurysms; (II) anatomical structures not suitable for EVAR, requiring surgical intervention, and patients who have undergone previous EVAR or open repair (OR); (III) aortic ulcers, pseudoaneurysms, iliac artery aneurysms, and traumatic dissecting aneurysms; (IV) concurrent connective tissue diseases, such as Ehlers-Danlos syndrome. Patient clinical status, medical history, treatment data were collected through hospital, imaging department, interventional therapy department records.
Endpoints
The primary endpoint was the occurrence of AAA rupture during the perioperative period of EVAR. Perioperative period was defined as all time from admission to discharge of the patient.
Definitions
The study cohort of patients was divided into two groups based on infrarenal aortic neck anatomy. All patients with AAAs had proximal neck lengths greater than 10 mm. Angulation measurement has been reported previously (16) (Figure 2). The alpha angle is formed between the suprarenal aorta and the aneurysm neck, and the beta angle between the aneurysm neck and sac. Accordingly, patients were included in the severe proximal aneurysm neck angulation group if the neck length >10 mm with an infrarenal angle (β) ≥45°, and/or suprarenal angle (α) ≥45° and non-severe proximal aneurysm neck angulation was defined as alpha angle and beta angle <45°. The length of the neck was defined as the distance between the most distal point of the origin of the lower most renal artery and the beginning of the aneurysm.
Data collection
Data were collected from patient medical records and included the following baseline and morphological variables: age, gender, hypertension, diabetes, smoking, symptom, max aneurysm diameter (mm), proximal aneurysm neck angulation aneurysm neck diameter at distal renal artery (mm), maximum common iliac diameter (mm), maximum common femoral diameter, bilateral common iliac angle (degrees). Patients were divided into two groups: with or without severe proximal aneurysm neck angulation.
Statistical analysis
Characteristics of the study population were summarized using descriptive statistical methods. The patients were categorized according to the angulation in 2 groups from 0–44° and from 45–90°. Next, univariate logistic regression and multivariate logistic regression models were used to examine whether proximal aneurysm neck angulation and other covariates had an independent effect on rupture of AAAs. Linear regression was used to assess the association of proximal neck angle with rupture risk. Continuous variables were described as mean and standard deviation. Categorical variables are presented as count and percentage. Confidence intervals of 95% (95% CI) were used and statistical significance was considered for P<0.050.
Ethical statement
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Institutional Review Board of the Shandong Provincial Hospital Affiliated to Shandong First Medical University (No. 2024-713) with a waiver for informed consent due to the retrospective nature of the study. The Affiliated Suzhou Hospital of Nanjing Medical University and Tangshan Workers Hospital were also informed and agreed with the study.
Results
Among the 160 patients included in the study, 53 (33.1%) exhibited severe proximal AAA neck angulation (≥45°). The demographic and clinical characteristics of the cases including age, gender, hypertension, diabetes, smoking, symptom and morphological and characteristics of AAA are summarized in Table 1. Females were found more frequently in the severe proximal aneurysm neck angulation group than in those with non-severe proximal aneurysm neck angulation group (P=0.03). Apart from the factor, there was no noticeable difference in the basic characteristics between the two groups.
Table 1
| Characteristics | Angulation ≥45° (n=53) | Angulation <45° (n=107) | P value |
|---|---|---|---|
| Age (years) | 69.5±8.6 | 68.5±8.3 | 0.44 |
| Gender | 0.03 | ||
| Female | 26 (49.1) | 34 (31.8) | |
| Male | 27 (50.9) | 73 (68.2) | |
| Hypertension | 38 (71.7) | 73 (68.2) | 0.65 |
| Diabetes | 5 (9.4) | 17 (15.9) | 0.26 |
| Smoking | 21 (39.6) | 57 (53.3) | 0.10 |
| Symptom | 0.93 | ||
| Abdominal pain | 16 (30.2) | 33 (30.8) | |
| Non-abdominal pain | 37 (69.8) | 74 (69.2) | |
| Max aneurysm diameter (mm) | 53.7±14.4 | 54.9±12.3 | 0.52 |
| Aneurysm neck diameter at distal renal artery (mm) | 21.1±4.6 | 21.9±4.4 | 0.26 |
| Maximum common iliac diameter (mm) | 16.8±6.5 | 15.1±4.6 | 0.95 |
| Maximum common femoral diameter (mm) | 9.5±1.4 | 9.9±1.8 | 0.13 |
| Bilateral common iliac angle (degrees) | 53.0±13.0 | 52.4±13.6 | 0.79 |
Data are presented as n (%) or mean ± standard deviation. Brunner-Munzel t approximation (for two sample comparison). P<0.05 indicates a significant difference between the two groups.
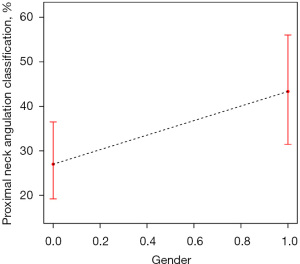
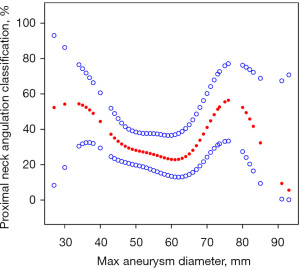
A total of 18 patients (11.3%) developed perioperative rupture of AAA following severe proximal aneurysm neck angulation in this study. The univariate regression analysis showed that severe proximal aneurysm neck angulation was significantly correlated with rupture of AAAs (OR =4.927, 95% CI: 1.733–14.009, P=0.002). In addition, female vs. male (OR =2.983, 95% CI: 1.088–8.179, P=0.03), abdominal pain vs. non-abdominal pain (OR =3.301, 95% CI: 1.214–8.975, P=0.01) and max aneurysm diameter (OR =1.092, 95% CI: 1.048–1.139, P<0.001) might also be associated with rupture of AAAs (Table 2). Prior to conducting the multivariable regression analysis, we meticulously assessed the potential for multicollinearity, particularly considering the variables: proximal aneurysm neck angulation, gender, and maximum aneurysm diameter. Employing the variance inflation factor (VIF) as our primary quantitative tool, the results revealed that the collinearity among these variables was not significant (all VIF values were below 5). This indicates that there is no excessive correlation between the independent variables and retaining them in the model does not compromise the accuracy or stability of our regression analysis. Therefore, we decided to include all these variables in our final multivariable regression model to comprehensively evaluate their impact on the risk of AAA rupture. After multivariable risk adjustment for potential confounding factors (Table 3), severe proximal aneurysm neck angulation (OR =8.159, 95% CI: 2.202–30.236, P=0.001) and max aneurysm diameter (OR =1.093, 95% CI: 1.046–1.143, P<0.001) were still positively associated with rupture of AAAs. Meanwhile, we found that proximal aneurysm neck angulation was obviously correlated with the female (r=0.0716, P=0.02) and max aneurysm diameter (r=0.0221, P=0.03) (Figures 3,4).
Table 2
| Variables | Values | Odds ratio (95% CI) | P value |
|---|---|---|---|
| Age (years) | 68.8±8.4 | 1.052 (0.989–1.120) | 0.10 |
| Gender | |||
| Female | 60 (37.5) | 2.983 (1.088–8.179) | 0.03 |
| Male | 100 (62.5) | 1.0 | |
| Symptom | |||
| Abdominal pain | 49 (30.6) | 3.301 (1.214–8.975) | 0.01 |
| Non-abdominal pain | 111 (69.4) | 1 | |
| Proximal neck angulation classification | |||
| Severe proximal aneurysm neck angulation | 53 (33.1) | 4.927 (1.733–14.009) | 0.002 |
| Non-severe proximal aneurysm neck angulation | 107 (66.9) | 1.0 | |
| Max aneurysm diameter (mm) | 54.5±13.0 | 1.092 (1.048–1.139) | <0.001 |
| Aneurysm neck diameter at distal renal artery (mm) | 21.7±4.4 | 1.069 (0.960–1.190) | 0.22 |
| Maximum common iliac diameter (mm) | 51.6±14.4 | 0.968 (0.934–1.003) | 0.07 |
| Maximum common femoral diameter (mm) | 9.7±1.7 | 0.972 (0.722–1.308) | 0.85 |
| Bilateral common iliac angle (degrees) | 52.6±13.4 | 1.010 (0.974–1.048) | 0.57 |
Data are presented as n (%) or mean ± standard deviation. Severe proximal aneurysm neck angulation: the neck length >10 mm with an infrarenal angle (β) ≥45°, and/or suprarenal angle (α) ≥45°; non-severe proximal aneurysm neck angulation: alpha angle and beta angle <45°. AAA, abdominal aortic aneurysm; CI, confidence interval.
Table 3
| Variables in model | Odds ratio (95% CI) | P value |
|---|---|---|
| Gender | ||
| Male | 1.0 | |
| Female | 2.301 (0.569–9.379) | 0.24 |
| Proximal neck angulation classification | ||
| Severe proximal aneurysm neck angulation | 8.159 (2.202–30.236) | 0.001 |
| Non-severe proximal aneurysm neck angulation | 1.0 | |
| Max aneurysm diameter (mm) | 1.093 (1.046–1.143) | <0.001 |
| Symptom | ||
| Abdominal pain | 2.158 (0.516–9.028) | 0.29 |
| Non-abdominal pain | 1.0 |
All models adjusted for gender, proximal neck angulation classification, max aneurysm diameter and symptom. Odds ratios are presented per standard deviation increase of morphological parameter. Severe proximal aneurysm neck angulation: the neck length >10 mm with an infrarenal angle (β) ≥45°, and/or suprarenal angle (α) ≥45°; non-severe proximal aneurysm neck angulation: alpha angle and beta angle <45°. AAA, abdominal aortic aneurysm; CI, confidence interval.
Twelve patients developed rupture in the severe proximal aneurysm neck angulation group, and 6 patients developed rupture in the no-severe proximal aneurysm neck angulation group. The distribution of rupture in patients with severe proximal aneurysm neck angulation was significantly higher than in patients without severe proximal aneurysm neck angulation (15.9% vs. 7.8%, P=0.001). After adjusting for confounding factors such as gender and maximum aneurysm diameter, separate nonlinear relationships were observed: proximal aneurysm neck angulation and rupture (P<0.001), as well as aneurysm neck classification and rupture (P<0.001), as illustrated in Figures 5,6. The risk of rupture increased after the proximal aneurysm neck angulation level up to the turning point (41°) (OR =1.086, 95% CI: 1.037–1.137; P<0.001). When the proximal aneurysm neck angulation was <41°, the level of proximal aneurysm neck angulation was not associated with the risk of rupture (OR =0.985, 95% CI: 0.933–1.040; P=0.58) (Table 4).
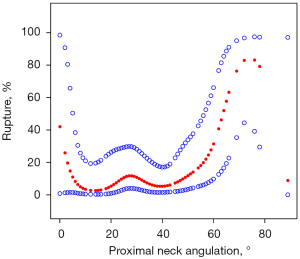

Table 4
| Proximal neck angulation | Odds ratio (95% CI) | P value |
|---|---|---|
| <41° | 0.985 (0.933–1.040) | 0.58 |
| ≥41° | 1.086 (1.037–1.137) | <0.001 |
AAA, abdominal aortic aneurysm; CI, confidence interval.
Discussion
To date, a series of studies (8,17-19) have investigated for morphological parameters influencing mortality and reintervention after EVAR. Some studies have shown partial morphological parameter difference in prognosis, while others have shown no difference in mortality and reintervention rates (20,21). Our research focused on the morphological parameters influencing perioperative rupture of AAAs. A single morphological parameter, proximal neck angulation, appeared to have a significant influence on rupture of AAAs, independent of known confounders. In addition, max aneurysm diameter was considered another risk factor related to rupture of AAAs. As the current analysis found, these two factors were also associated with the difference of gender. Accordingly, gender was also adjusted in the analysis. Even after accounting for potential confounding factors, our analysis revealed a significant correlation between the angulation of the proximal neck and perioperative rupture of AAAs.
The findings indicate that severe neck angulation may not be a poor prognostic indicator for overall/aneurysm related mortality and rupture in the medium term after EVAR, but may increase the risk of late type 1 endoleak and secondary re-intervention (17). Our research focused on aneurysmal ruptures during perioperative periods. We found that 33.1% of patients exhibited severe angulation of the proximal aneurysmal neck. Unfortunately, our study indicated that the greater the proximal aneurysmal neck angulation, the higher risk of aneurysm rupture. More importantly, the data further revealed that the risk of rupture increased with the increase of proximal aneurysmal neck angulation until the critical point (41°) had been exceeded. After multivariable risk adjustment for potential confounding factors, severe proximal aneurysm neck angulation (OR =8.159, 95% CI: 2.202–30.236, P=0.001) was still positively associated with rupture of AAAs. Our data demonstrated a relatively large 95% CI, and while the corresponding P value is significant, we adopt a cautious stance in interpreting these results. This finding underscores the need for more precise criteria to evaluate proximal aneurysmal neck angulation, aiming to prevent rupture. Consequently, patients necessitate vigilant monitoring throughout preoperative assessments and subsequent EVAR follow-ups.
Gender difference has been widely noticed in cardiovascular disease (22). Several studies (23,24) have suggested that the prognosis of individuals with AAA is worse for women than men, with the operative mortality following repair of intact aneurysm being higher in women than men. Meanwhile, females are at higher risk than males for mortality and major complications in AAAs. If left untreated, AAAs can grow and rupture, leading to death in 80% of patients (25). Sex-based differences exist in AAAs disease, including its prevalence [2–6 times more common in men than in women (26)], presentation [smaller aneurysms with higher risk of rupture in women (4)], and treatment [women being less likely than men to undergo repair (25)]. Females were significantly associated with ruptured AAAs in univariate regression analysis, but females were slightly associated with ruptured AAAs in multivariate confounding regression analysis. This may be related to the confounding of proximal neck angulation. Our study indicated a severe proximal neck angulation in females. It is noteworthy that Qayyum et al. (17) reported that patients with severe neck angulation were less likely to be males (OR =0.50, 95% CI: 0.41–0.61, P<0.001), which are consistent with our results. In the study of ruptured AAA risk, more attention should be paid to the risk of females, especially to the females with severe proximal aneurysm angulation. Additional evaluations of survival following elective AAA repairs indicate improved short-term surgical outcomes. However, there is a concerning trend of poor long-term prognosis, particularly among female patients. Our results also indicated that women exhibited more complex morphological characteristics perioperatively in EVAR, which correlates with a poorer prognosis for female patients. Such interventions must undergo rigorous scientific assessment prior to EVAR, and comprehensive management of AAAs in women is critical (4).
The generally accepted annual risk of rupture exceeds the perioperative risks associated with elective repair at a maximum aortic diameter of 5 cm for women and 5.5 cm for men (27). Our results demonstrated the correlation between max aneurysm diameter and proximal neck angulation classification for linear terms. Proximal neck angulation classification showed slightly positive correlation with max aneurysm diameter (r=0.0716, P=0.02). With the increase of aneurysm diameter, the proximal aneurysmal neck angulation of the patients will become larger and larger. The risk of AAA rupture was higher when aneurysmal diameter combined with severe aneurysmal neck angulation.
Although our analysis suggested that proximal aneurysmal neck angulation was associated with rupture of AAAs, there are some limitations in this study that should be noted. Firstly, inherent to all observational studies, residual or unmeasured confounding cannot be entirely ruled out. Moreover, the retrospective nature of this study introduces potential biases inherent to such studies, and the findings may reflect the particular demographics or procedures specific to our institution rather than a broader population. Thirdly, the definition and classification of proximal aneurysmal neck angulation remain subjects of ongoing debate. Additionally, no increase in aneurysm diameter was observed among the patients included, which could imply a lack of comprehensive data to substantiate more definitive conclusions.
Conclusions
EVAR remains the preferred surgical approach for managing AAAs, guided by morphological and anatomical considerations. Research has demonstrated that morphological variances significantly impact mortality and re-intervention rates associated with EVAR. Our study further establishes a significant correlation between the extent of proximal neck angulation and the risk of perioperative rupture in these aneurysms. Notably, we found that proximal neck angulation differs significantly between genders, with females exhibiting greater angulation than males. Given these findings, clinicians should meticulously assess proximal neck angulation in patients undergoing EVAR and consider early intervention for those with severe angulation to mitigate the risk of rupture.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://cdt.amegroups.com/article/view/10.21037/cdt-24-210/rc
Data Sharing Statement: Available at https://cdt.amegroups.com/article/view/10.21037/cdt-24-210/dss
Peer Review File: Available at https://cdt.amegroups.com/article/view/10.21037/cdt-24-210/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://cdt.amegroups.com/article/view/10.21037/cdt-24-210/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Institutional Review Board of the Shandong Provincial Hospital Affiliated to Shandong First Medical University (No. 2024-713) with a waiver for informed consent due to the retrospective nature of the study. The Affiliated Suzhou Hospital of Nanjing Medical University and Tangshan Workers Hospital were also informed and agreed with the study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Krisna Pertiwi PF, Sudarma IW, Prana Jagannatha GN, et al. Outcomes of advanced EVAR versus open surgery in the management of complex abdominal aortic aneurysm repair: A systematic review and meta-analysis. Asian Cardiovasc Thorac Ann 2024; Epub ahead of print. [Crossref] [PubMed]
- Stather PW, Sidloff DA, Rhema IA, et al. A review of current reporting of abdominal aortic aneurysm mortality and prevalence in the literature. Eur J Vasc Endovasc Surg 2014;47:240-2. [Crossref] [PubMed]
- Cooper MA, Upchurch GR Jr. The Society of Vascular Surgery Practice Guidelines on the Care of Patients With Abdominal Aortic Aneurysms. JAMA Surg 2019;154:553-4. [Crossref] [PubMed]
- Chaikof EL, Dalman RL, Eskandari MK, et al. The Society for Vascular Surgery practice guidelines on the care of patients with an abdominal aortic aneurysm. J Vasc Surg 2018;67:2-77.e2. [Crossref] [PubMed]
- Long C, Katsargyris A, Milner R, et al. Five-Year Results for Abdominal Aortic Aneurysm Repair with the GORE® EXCLUDER® Device: Insights from the Gore Global Registry for Endovascular Aortic Treatment (GREAT). Ann Vasc Surg 2024;106:247-54. [Crossref] [PubMed]
- Taofan T, Adiarto S, Dakota I, et al. Endovascular management of aortic aneurysm with severe neck angulation and/or iliac artery tortuosity using multiple stiff wire technique: a case series. F1000Res 2024;12:1137. [Crossref] [PubMed]
- Accarino G, De Vuono F, Accarino G, et al. Endurant Stent Graft for Treatment of Abdominal Aortic Aneurysm Inside and Outside of the Instructions for Use for the Proximal Neck: A 14-Year, Single-Center Experience. J Clin Med 2024;13:2589. [Crossref] [PubMed]
- GnanaDev R. Use of the GORE Conformable Excluder Device in Highly Angulated Aortic Neck Anatomy: Mid-term Outcomes. Vasc Endovascular Surg 2024;58:663-8. [Crossref] [PubMed]
- Columbo JA, Martinez-Camblor P, O'Malley AJ, et al. Long-term Reintervention After Endovascular Abdominal Aortic Aneurysm Repair. Ann Surg 2021;274:179-85. [Crossref] [PubMed]
- Gunnarsson K, Wanhainen A, Björck M, et al. Nationwide Study of Ruptured Abdominal Aortic Aneurysms During Twenty Years (1994-2013). Ann Surg 2021;274:e160-6. [Crossref] [PubMed]
- Bulder RMA, Talvitie M, Bastiaannet E, et al. Long-term prognosis after elective abdominal aortic aneurysm repair is poor in women and men: the challenges remain. Ann Surg 2020;272:773-8. [Crossref] [PubMed]
- Varkevisser RRB, Patel PB, Swerdlow NJ, et al. The Impact of Proximal Neck Anatomy on the 5-Year Outcomes Following Endovascular Aortic Aneurysm Repair With the Ovation Stent Graft. J Endovasc Ther 2023; Epub ahead of print. [Crossref] [PubMed]
- Chinsakchai K, Sirivech T, Moll FL, et al. The correlation of aortic neck angle and length in abdominal aortic aneurysm with severe neck angulation for prediction of intraoperative neck complications and postoperative outcomes after endovascular aneurysm repair. J Clin Med 2023;12:5797. [Crossref] [PubMed]
- Bonvini S, Spadoni N, Frigatti P, et al. Early outcomes of the Conformable endograft in severe neck angulation from the Triveneto Conformable Registry. J Vasc Surg 2023;78:954-962.e2. [Crossref] [PubMed]
- Oliveira NFG, Gonçalves FB, Hoeks SE, et al. Long-term outcomes of standard endovascular aneurysm repair in patients with severe neck angulation. J Vasc Surg 2018;68:1725-35. [Crossref] [PubMed]
- Bastos Gonçalves F, de Vries JP, van Keulen JW, et al. Severe proximal aneurysm neck angulation: early results using the Endurant stentgraft system. Eur J Vasc Endovasc Surg 2011;41:193-200. [Crossref] [PubMed]
- Qayyum H, Hansrani V, Antoniou GA. Prognostic Role of Severe Infrarenal Aortic Neck Angulation in Endovascular Aneurysm Repair. Eur J Vasc Endovasc Surg 2021;62:409-21. [Crossref] [PubMed]
- Stather PW, Sayers RD, Cheah A, et al. Outcomes of endovascular aneurysm repair in patients with hostile neck anatomy. Eur J Vasc Endovasc Surg 2012;44:556-61. [Crossref] [PubMed]
- Li RD, Soult MC. Advanced Endovascular Treatment of Complex Aortic Pathology. Surg Clin North Am 2023;103:e1-e11. [Crossref] [PubMed]
- Chinsakchai K, Suksusilp P, Wongwanit C, et al. Early and late outcomes of endovascular aneurysm repair to treat abdominal aortic aneurysm compared between severe and non-severe infrarenal neck angulation. Vascular 2020;28:683-91. [Crossref] [PubMed]
- Murray D, Szeberin Z, Benevento D, et al. A comparison of clinical outcomes of abdominal aortic aneurysm patients with favorable and hostile neck angulation treated by endovascular repair with the Treovance stent graft. J Vasc Surg 2020;71:1881-9. [Crossref] [PubMed]
- Mosca L, Barrett-Connor E, Wenger NK. Sex/gender differences in cardiovascular disease prevention: what a difference a decade makes. Circulation 2011;124:2145-54. [Crossref] [PubMed]
- Lo RC, Schermerhorn ML. Abdominal aortic aneurysms in women. J Vasc Surg 2016;63:839-44. [Crossref] [PubMed]
- Norman PE, Powell JT. Abdominal aortic aneurysm: the prognosis in women is worse than in men. Circulation 2007;115:2865-9. [Crossref] [PubMed]
- Aber A, Tong TS, Chilcott J, et al. Sex differences in national rates of repair of emergency abdominal aortic aneurysm. Br J Surg 2019;106:82-9. [Crossref] [PubMed]
- Salata K, Hussain MA, de Mestral C, et al. Prevalence of Elective and Ruptured Abdominal Aortic Aneurysm Repairs by Age and Sex From 2003 to 2016 in Ontario, Canada. JAMA Netw Open 2018;1:e185418. [Crossref] [PubMed]
- Rokosh RS, Wu WW, Eskandari MK, et al. Society for Vascular Surgery implementation of guidelines in abdominal aortic aneurysms: Preoperative surveillance and threshold for repair. J Vasc Surg 2021;74:1053-4. [Crossref] [PubMed]



