How far have we come with bioresorbable vascular scaffolds, and where should we go?
Bioresorbable vascular scaffolds (BVS) as the next revolution in interventional cardiology
Technical advances in percutaneous coronary intervention (PCI) have had huge impact on the treatment of coronary artery disease (CAD). Current guidelines recommend drug-eluting stent (DES) implantation as the standard care in CAD patients (1). However, even the newest generation DES have intrinsic limitations, such as the persistent risk of late stent failure, delayed chronic inflammation due to the polymer or metal components of stent, and loss of physiologic vasomotor function induced by the metal cage. Recently, BVS have emerged as an innovative tool to overcome the long-term complications of DESs. By applying a temporary scaffold, BVS provides adequate radial support to seal dissection, limit acute recoil and constrictive remodeling, whilst restoring normal vascular function after absorption.
To date, a number of BVS have been tested in clinical trials (2), among which, the Absorb is the most-studied BVS. After safety confirmation by cohort based studies (3,4), a series of registry studies and randomized clinical trials (RCTs) have shown promising results for the Absorb BVS, being non-inferior to the everolimus-eluting stent (EES). BVS proved to have comparable safety and effectiveness outcomes at 1-year follow up. However interventional cardiologists are not yet comfortable in applying this novel technology daily practice because of several issues. First, there are concerns of an increased rate of scaffold thrombosis (ST). This may have been caused not only by the property of the scaffold, such as its thick 150 µm strut, but also by suboptimal deployment techniques such as the lack of intravascular imaging tool use or lack of post-dilatation. Second, every doctor must pay attention to and adhere to the specific protocol of BVS deployment, which may be cumbersome and thus act as a practical hurdle in daily practice. Third, the indication for BVS is limited not only by lesion complexity but also by patients’ general or local complexity. The performance of BVS has not been well tested in the complex lesions such as bifurcation or calcified tortuous lesions, or in the patients with diabetes or STEMI.
Regarding the unsolved issues discussed above, Kraak et al. discussed the 2-year outcomes of Absorb BVS in a PCI population reflecting daily clinical practice (5). Of the 135 patients analyzed, 8% had chronic renal failure, 26% had previous PCI and 51% initially presented as acute coronary syndrome. Also, lesions included bifurcation (15%) and calcified lesions (11%). During the 2-year follow up period, event rates were cardiac death 0.7%, MI 5.3%, definite ST 3.0% and TVF 14.4%, respectively. By stratified analysis, patients who met the ABSORB II criteria and those with a SYNTAX score lower than the median value (11.5) had a significantly lower event rate.
ST after BVS implantation
Based on current studies, angiographic and clinical event rates after BVS were similar to that after EES in six RCTs evaluating the performance of Absorb (ABSORB II, ABSORB III, ABSORB China, ABSORB Japan, EVERBIO II, TROFI II). Also, the 1-year relative rates of the patient-oriented composite endpoint did not differ significantly between BVS and EES in a recent patient-level, pooled meta-analysis including 3,389 patients with stable CAD or stabilized acute coronary syndrome (6). Despite the current promising results, there exists a concern of the increased rate of ST. For example, several registry based results, such as the GHOST-EU and BVS-EXAMINATION registry, have reported numerically higher thrombosis rates after BVS implantation [2.1% in the GHOST-EU registry (7), 2.4% in the BVS-EXAMINATION registry (8)]. Also, a meta-analysis including 10,510 patients concluded that those with BVS implantation were at a higher risk for ST (OR 2.06; 95% CI, 1.31–3.22, P=0.03) (9). Until now, a few meta-analyses have shown the overall risk of BVS ST was a little bit higher than that of EES (Table 1). Within these studies, we could see a trend of higher ST in BVS, although the statistical significances were slightly inconsistent probably due to the different profile of included studies.
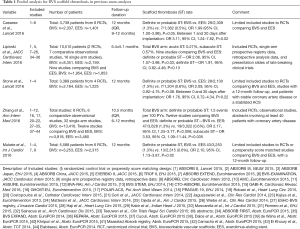
Full table
Moreover, in a recent report at the TCT 2016, the 3-year results of the Absorb II trial showed that definite or probable thrombosis was significantly higher in the BVS group than in EES group [2.8% (9/320) vs. 0.0% (0/159), P=0.03]. Interestingly, the rate of very late ST (those occurring from 1–3 years after deployment) was significantly higher in BVS than in EES [1.8% (6/320) vs. 0.0% (0/159), P=0.19], reflecting the safety concern of the dissolved or dismantled scaffold during 3 years.
Regarding thrombosis in BVS, a few unique characteristics of BVS may contribute to the increased risk of ST. Current BVS has struts that are thicker and wider than 2nd generation DES (10). This leads to a greater strut protrusion, leading to a greater turbulent flow and platelet activation. Therefore, due to the physical characteristics of BVS, optimization techniques, such as intravascular imaging and high-pressure post-dilation are strongly recommended in BVS implantation (2). The ST event rate in Kraak et al. was 3.0%, all occurring during the initial 6 months. Although the usage of intravascular imaging was not reported, post-dilatation was performed only in 55% of the total lesions, which can partially explain the high thrombosis rate. Regarding the BVS-specific technique, Puricel et al. stated that the Absorb-specific protocol significantly reduced thrombosis rate, compared to results of early BVS experience (11). Also, results of optimal implantation using the ‘Prepare the lesion, Size appropriately, Post-dilate (PSP) method’ was introduced at the TCT 2016. From five RCTs of Absorb, only 10.4% (292/2,815) of the patients received optimal PSP, and this population showed decreased target lesion related outcomes and ST compared to others. Thus the clinical outcomes of recent papers on BVS that were implanted under early DES techniques are somewhat worse than EES or future results of BVS that are implanted under new PSP method. In the more recent study such as ABSORB China, the target-lesion related outcomes at 2 years were comparable between Absorb and EES. Further large scale studies with a long follow-up (ABSORB III) will give us answers to current issues comparing BVS and EES. Additionally, we should keep in mind that it takes 3 years for Absorb to be fully resolved. During the resolving period, antiplatelet therapy should be stressed, and the beneficial values of BVS, such as recovery of vasomotion, may be accelerated after the initial 3 years.
BVS to complex lesions
Most RCTs for BVS implantation were based on relatively stable patients with simple lesions. The ABSORB trials included patients with minimal comorbidities while excluded patients with history of renal insufficiency, cancer or congestive heart failure, depressed systolic function, or ongoing myocardial infarction. Also, they enrolled only simple lesions, such as, one de novo native lesion per epicardial artery, with diameter stenosis between 50% and 100%, with a TIMI flow of ≥1, whereas excluded long lesions, left main lesions, ostial lesions, bifurcation lesions, lesions with excessive tortuosity of extreme angulation or heavy calcification. This population is distinctly different from the PCI population that we usually meet in the clinic, especially in the current era where more complex coronary lesions are candidates of PCI. In the study of Kraak et al., authors showed increased clinical outcomes in those with complex clinical and lesion factors. Two years target vessel failure for patients who did not meet the Absorb criteria was 20.3%, which was significantly higher than that of patients who met the Absorb criteria.
To expand the spectrum of BVS, some recent studies have shown acceptable results of BVS in extended candidates (i.e., patients with ST elevation myocardial infarction or complex lesions such as bifurcation and left main diseases) (12,13). The results of BVS for off-label indications will be assessed by ongoing large scale all-comer registries such as the FRANCE-ABSORB registry (ClinicalTrials.gov identifier: NCT02238054) and FEAST Russia registry (ClinicalTrials.gov identifier: NCT02707783). The result of BVS for long (>24 mm) lesion or multi-vessel CAD will be evaluated in ongoing IT-DISAPPEARS registry (ClinicalTrials.gov identifier: NCT02004730). Comparison of performance between BVS vs. EES in patients at high risk of restenosis is underway in COMPARE-ABSORB RCT (ClinicalTrials.gov identifier: NCT02486068). Patients with moderate complex coronary lesions are enrolled in the ongoing ABSORB EXTEND registry, which is different from the initial BVS studies like ABSORB III and IV trial. Data from these studies will give us additional answers on the role of BVS in complex lesions. Before the routine use of BVS for patients with multiple comorbidities and complex lesions can be advocated, we need more data on long-term safety and efficacy along with improvements in scaffold design.
Development of an Ideal BVS
Although 2nd generation DES could dramatically minimize adverse clinical outcomes after PCI, long term limitations are still a major challenge. Also, the metal cage on coronary artery inhibits compensatory vascular remodeling, non-invasive imaging options, or future treatment options including coronary bypass surgery (14). Absorbable scaffolds were designed to overcome the limitations of conventional, non-absorbable metal-based DESs. The theoretical benefits of BVS such as recovery of physiologic vasomotor function should be achieved under implantation techniques as comfortable as 2nd generation DESs. However, due to the relatively short history of BVS, this technology is still in its infancy. Currently used 1st generation BVS have limitations, such as scaffold thickness that limits deliverability and materials that limit overexpansion and side branch access, and the increased rate of ST. To improve the difficult and cumbersome technique of implantation, absorbable metal scaffolds are under development based on its superior radial strength, negligible elastic recoil, better adaptability, and/or better visibility under fluoroscopy (2). Preliminary results of various new BVS were presented at the TCT 2016 (the FANTOM II study, MeRes-1 study, FORTITUDE study, and the FUTURE-I study). These studies presented that new BVS showed favorable angiographic outcomes, such as a low late loss with a stable scaffold area. However, despite the promising angiographic results, we still need long term follow up results for comparison of clinical outcomes. Other ongoing studies should give us additional answers to the efficacy and safety of newly developed BVSs (15).
Antiplatelet therapy after BVS
The adequate duration of dual antiplatelet therapy after BVS is an important issue that needs to be answered. Appropriate antiplatelet therapy should be more actively considered due to the concern of higher ST. Although various current studies support the use of DAPT <12 months in 2nd generation DES, this should not be adopted to BVS. Based on current available data, DAPT should be used for a sufficient period, and also new P2Y12 receptor antagonists (i.e., prasugrel and ticagrelor) should be considered, especially in patients with increased thrombosis risk under the situation of acute coronary syndrome. Dismantled scaffold fragment may play a role as the nidus of very late thrombosis. Thus BVS implantation may require the stronger and longer antiplatelet therapy until the complete resolution. Considering the existence of remnant scaffold until 3-year post-implantation and the increased rate of very late ST, DAPT should be prescribed until the BVS is fully resolved. Thus, we may avoid BVS implantation in patients who require short DAPT. Along with the development of 2nd generation BVS with thinner struts and technical advances to achieve homogenous stent expansion and apposition, the adequate duration of DAPT may also change.
Conclusions
The Absorb BVS has been shown to be safe and effective in treatment for CADs, and thus received both the CE mark and FDA approval. However, recent data of ongoing trials have presented that BVS possess several critical drawbacks that should be overcome in future developments. This includes the concern of higher ST, and the limited spectrum of application only to simple CADs because of the poor deliverability. Appropriate techniques of implantation and adequate duration of antiplatelet agents are major issues that should be solved. In order to improve clinical outcomes and expand indications of BVS, new BVS should include a stronger radial force, thinner strut, shorter resolution time than 3 years, better visibility and deliverability.
Acknowledgements
Funding: This study was supported by a research grant funded by Endocor Korea (grant number 800-20150069).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Levine GN, Bates ER, Blankenship JC, et al. 2015 ACC/AHA/SCAI Focused Update on Primary Percutaneous Coronary Intervention for Patients With ST-Elevation Myocardial Infarction: An Update of the 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention and the 2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction. J Am Coll Cardiol 2016;67:1235-50. [Crossref] [PubMed]
- Indolfi C, De Rosa S, Colombo A. Bioresorbable vascular scaffolds - basic concepts and clinical outcome. Nat Rev Cardiol 2016;13:719-29. [Crossref] [PubMed]
- Onuma Y, Dudek D, Thuesen L, et al. Five-year clinical and functional multislice computed tomography angiographic results after coronary implantation of the fully resorbable polymeric everolimus-eluting scaffold in patients with de novo coronary artery disease: the ABSORB cohort A trial. JACC Cardiovasc Interv 2013;6:999-1009. [Crossref] [PubMed]
- Gogas BD, Serruys PW, Diletti R, et al. Vascular response of the segments adjacent to the proximal and distal edges of the ABSORB everolimus-eluting bioresorbable vascular scaffold: 6-month and 1-year follow-up assessment: a virtual histology intravascular ultrasound study from the first-in-man ABSORB cohort B trial. JACC Cardiovasc Interv 2012;5:656-65. [Crossref] [PubMed]
- Kraak RP, Grundeken MJ, Hassell ME, et al. Two-year clinical outcomes of Absorb bioresorbable vascular scaffold implantation in complex coronary artery disease patients stratified by SYNTAX score and ABSORB II study enrolment criteria. EuroIntervention 2016;12:e557-65. [Crossref] [PubMed]
- Stone GW, Gao R, Kimura T, et al. 1-year outcomes with the Absorb bioresorbable scaffold in patients with coronary artery disease: a patient-level, pooled meta-analysis. Lancet 2016;387:1277-89. [Crossref] [PubMed]
- Capodanno D, Gori T, Nef H, et al. Percutaneous coronary intervention with everolimus-eluting bioresorbable vascular scaffolds in routine clinical practice: early and midterm outcomes from the European multicentre GHOST-EU registry. EuroIntervention 2015;10:1144-53. [Crossref] [PubMed]
- Brugaletta S, Gori T, Low AF, et al. Absorb bioresorbable vascular scaffold versus everolimus-eluting metallic stent in ST-segment elevation myocardial infarction: 1-year results of a propensity score matching comparison: the BVS-EXAMINATION Study (bioresorbable vascular scaffold-a clinical evaluation of everolimus eluting coronary stents in the treatment of patients with ST-segment elevation myocardial infarction). JACC Cardiovasc Interv 2015;8:189-97. [Crossref] [PubMed]
- Lipinski MJ, Escarcega RO, Baker NC, et al. Scaffold Thrombosis After Percutaneous Coronary Intervention With ABSORB Bioresorbable Vascular Scaffold: A Systematic Review and Meta-Analysis. JACC Cardiovasc Interv 2016;9:12-24. [Crossref] [PubMed]
- Colombo A, Ruparelia N. Who Is Thrombogenic: The Scaffold or the Doctor? Back to the Future! JACC Cardiovasc Interv 2016;9:25-7. [Crossref] [PubMed]
- Puricel S, Cuculi F, Weissner M, et al. Bioresorbable Coronary Scaffold Thrombosis: Multicenter Comprehensive Analysis of Clinical Presentation, Mechanisms, and Predictors. J Am Coll Cardiol 2016;67:921-31. [Crossref] [PubMed]
- Felix CM, Fam JM, Diletti R, et al. Mid- to Long-Term Clinical Outcomes of Patients Treated With the Everolimus-Eluting Bioresorbable Vascular Scaffold: The BVS Expand Registry. JACC Cardiovasc Interv 2016;9:1652-63. [Crossref] [PubMed]
- Biscaglia S, Ugo F, Ielasi A, et al. Bioresorbable Scaffold vs. Second Generation Drug Eluting Stent in Long Coronary Lesions requiring Overlap: A Propensity-Matched Comparison (the UNDERDOGS study). Int J Cardiol 2016;208:40-5. [Crossref] [PubMed]
- Iqbal J, Onuma Y, Ormiston J, et al. Bioresorbable scaffolds: rationale, current status, challenges, and future. Eur Heart J 2014;35:765-76. [Crossref] [PubMed]
- Bouchi YH, Gogas BD. Biocorrodible metals for coronary revascularization: Lessons from PROGRESS-AMS, BIOSOLVE-I, and BIOSOLVE-II. Glob Cardiol Sci Pract 2015;2015:63. [Crossref] [PubMed]


