Incremental value of functional assessment over coronary anatomy in an acute myocardial infarction associated with mitral valve replacement
We present the case of a 72-year-old female with a history of ventricular arrhythmia under treatment with amiodarone and posterior leaflet mitral valve prolapse, presenting with acute pulmonary edema. A transthoracic echocardiogram (TTE) and a transesophageal echocardiogram (TEE) examination showed rupture of the posterior cord of the mitral valve with severe valve regurgitation, requiring emergent surgery with mechanic mitral valve replacement.
Six months after surgery she presented with progressive dyspnea. A TTE revealed thinning and hypokinesia of mid and basal lateral left ventricle wall, suggestive of pseudoaneurysm. No echocardiographic evidence of prosthesis malfunction was found.
In order to confirm diagnostic and evaluate possible pseudoaneurysm etiologies and since the patient suffered from claustrophobia, she underwent a computed tomography coronary angiography (CTCA).
The study was acquired using retrospective modulated electrocardiogram (ECG) gating, in order to assess left ventricular function as well as prosthetic valve morphology and function.
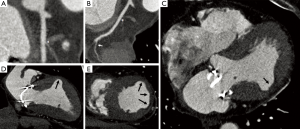
The CTCA identified non-calcified occlusion of the first obtuse marginal branch (Figure 1A,B, asterisk) and severe and diffuse non-calcified lesion at the second obtuse marginal branch (Figure 1B, arrow). The rest of the coronary tree showed no evidence of atherosclerosis.
CTCA also displayed concentric left ventricle hypertrophy, with interventricular septum thickness of 12.6 mm and left ventricular free wall thickness of 12.2 mm.
The left ventricular inferior and anterior lateral wall showed myocardial hypoattenuation suggestive of hypoperfusion (Figure 1C, arrow), mild wall thinning [Figure 1D,E, arrows (systolic images)], with akinetic inferolateral and incipient dyskinetic anterolateral wall motion at the transition of the mid and basal segments (Figure 2).

The mechanical mitral valve is well-placed and showed normal function, without any associated complications. Diffuse calcification of the posterior mitral annulus (peri-prosthesis) was also observed.
In this case, the temporal succession of events such as the absence of any other coronary artery lesion allows us to speculate that the occlusion might have developed during or after the surgery, suggesting that the underlying cause was the generation of a subintimal hematoma, a coronary spasm, vessel distortion generated by surgery, thrombotic occlusion by endothelium laceration or fixed mechanical occlusion by suture (2).
Injury of the obtuse marginal arteries is a rare but serious complication of mitral valve surgery. This complication is caused by the anatomical relationship that exist between the posterior segment of the mitral annulus and the coronary arteries that run through the left portion of the coronary network (3). Despite this was not the case, the distance of the circumflex and its branches from the mitral annulus is closer in hearts with left dominance or codominance comparing with right dominance. In fact no case of coronary artery injury in right dominance has been previously reported in the literature. If a big circumflex artery is present, running through the atrioventricular groove, damage of the artery can occur and has been documented particularly related to radiofrequency ablation procedures (4).
Therefore, it is mandatory that preoperative coronary angiography is performed in every patient undergoing mitral valve surgery to assess the dominance of coronary system and the course of the circumflex artery.
In this case, the role of the CTCA was vital, since it did not only clarify the diagnosis, showing the infarcted myocardial area and identifying the incipient aneurysm, but also contributed to identify the etiology by demonstrating the anatomic relationship of the structures and the absence of atherosclerotic disease in the rest of the coronary tree.
To the best of our knowledge, this is the first report of an aneurysm secondary to a complicated myocardial infarction associated to an occlusion of the obtuse marginal branches during or after valve replacement surgery.
AcknowledgementsOther Section
None.
FootnoteOther Section
Conflicts of Interest: The author has no conflicts of interest to declare.
ReferencesOther Section
- De Zan MC. Computed tomography coronary angiography. 2-chamber, 4-chamber and short axis views showing akinetic inferolateral and incipient dyskinetic anterolateral wall motion at the transition of the mid and basal segments. Asvide 2017;4:180. Available online: http://www.asvide.com/articles/1488
- Mantilla R, Legarra JJ, Pradas G, et al. Percutaneous coronary intervention for iatrogenic occlusion of the circumflex artery after mitral anuloplasty. Rev Esp Cardiol 2004;57:702-4. [Crossref] [PubMed]
- Warin-Fresse K, Isnard J, Guerin P, et al. J Radiol 2009;90:725-30. [Coronary CTA evaluation of the relationship between mitral valve annulus and coronary circulation: implications for percutaneous mitral annuloplasty]. [Crossref] [PubMed]
- Mao J, Moriarty JM, Mandapati R, et al. Catheter ablation of accessory pathways near the coronary sinus: value of defining coronary arterial anatomy. Heart Rhythm 2015;12:508-14. [Crossref] [PubMed]