The impact of IVUS guidance in treating complex lesions; are all “complex” lesions the same?
The main reason for the application of intravascular ultrasound (IVUS) in guiding drug-eluting stent (DES) implantation is because of its clinical benefit that has been shown in previous meta-analyses which included more than 30,000 patients across all coronary lesion subsets (1). Complex coronary lesions represent a unique subset which are more susceptible to adverse clinical events such as restenosis and thrombosis following percutaneous coronary interventions (PCI) in the DES era and while IVUS guidance has been reported to be favorable in treating some classes of complex lesions (2-4), the lingering question remains: what is a complex lesion? Regarding chronic total occlusions (CTOs) for instance, they have been graded in their own complexity according to: long vs. short occluded segment, extent of calcification, etc. Thus, a very short and non-calcified lesion may not be as complex as a long and severely calcified one. Likewise, bifurcation lesions could be either true bifurcations or just simply involve the ostium of the side branch. These two scenarios pose different challenges that could be resolved via imaging, but eventually their long-term outcome will be greatly defined by the extension of the pre-existing disease. Additionally, the degree of shear stress, low flow velocity and presence of multiple layers of stent struts make bifurcation lesions vulnerable to stent thrombosis (ST) and thus surrogates of their complexity (5). For these reasons, CTO and bifurcations may not be equal in terms of complexity. Specifically, by Syntax score, the maximum scoring points for a CTO is 9 points, while for a bifurcation the maximal possible point is 3. Should they both be considered complex? Should we lump these studies together in a “complex” lesion meta-analysis?
Bavishi et al. (6) showed in this meta-analysis, including eight RCTs, that IVUS-guided PCI led to significant reductions in the rates of major adverse cardiac events (MACE) by 36%, mainly driven by repeat revascularizations, in comparison with angiography-guidance and maximal benefit in-patients with acute coronary syndromes, diabetes mellitus and long lesions. We would like to congratulate the authors for reporting this meta-analysis, which may help trigger further studies. There are, however, a few points that merit further discussion. Firstly, the conspicuous absence of extensively calcified lesions from the cohorts reviewed must be noted, perhaps due to the limited data available for that subset of complex lesions. Secondly, the diverse anatomic characteristics of complex coronary lesions is probably one strong point in favor of imaging guidance and some may argue the importance of imaging in some over others. Two studies included in the meta-analyses included only CTOs and interestingly both studies accounted for greatest differences in ST in favor of IVUS-guidance (7,8). For example, Tian et al. showed that IVUS-guidance in CTO lesions led to lower incidence of stent restenosis possibly due to the optimization of stent expansion and edge dissections secondary to IVUS, and no benefit in the MACE outcome while another randomized study by Hong et al. (IVUS-XPL) have reported improvement in the MACE outcome and insignificant differences in cardiac death and target-lesion related myocardial infarction between the IVUS-guided and angiography-guided groups (2). Perhaps, differences in baseline characteristics and specific types of complex lesions would require different outcome variables (i.e., for CTO/bifurcation studies having ST as the main outcome variable would be preferable and for LMCA studies mortality and revascularizations would reflect better the effect of IVUS guidance).
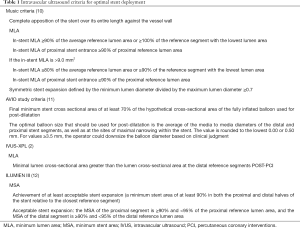
In addition, as reported, the meta-analysis included first-generation DES studies which may have impacted the outcomes reported when compared to the effect second-generation stents would have as shown by Shin et al. in a meta-analysis including studies with only newer-generation stents (9). Overall, the timing of imaging guidance is a critical aspect of employing IVUS in optimizing PCI. IVUS has been shown to be useful in preparing the lesion, facilitating device delivery and ensuring expansion in the pre-PCI phase as well as ensuring adequate apposition by guiding post-dilation in the immediate post-PCI period. Finally, there have been multiple criteria proposed for IVUS guidance in optimizing stent deployment dating back to the bare-metal stent era and subsequently tested in different variations ever since, hence the different criteria observed in recent studies (Table 1). So far, two of the criteria have stood out: the IVUS-XPL and the ILUMIEN III, the former having been tested and proven in a randomized trial of 1,400 patients and the latter will be further investigated in the ILUMIEN IV study.
Full table
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Steinvil A, Zhang YJ, Lee SY, et al. Intravascular ultrasound-guided drug-eluting stent implantation: An updated meta-analysis of randomized control trials and observational studies. Int J Cardiol 2016;216:133-9. [Crossref] [PubMed]
- Hong SJ, Kim BK, Shin DH, et al. Effect of Intravascular Ultrasound-Guided vs Angiography-Guided Everolimus-Eluting Stent Implantation: The IVUS-XPL Randomized Clinical Trial. JAMA 2015;314:2155-63. [Crossref] [PubMed]
- Kim JS, Kang TS, Mintz GS, et al. Randomized comparison of clinical outcomes between intravascular ultrasound and angiography-guided drug-eluting stent implantation for long coronary artery stenoses. JACC Cardiovasc Interv 2013;6:369-76. [Crossref] [PubMed]
- Park SJ, Kim YH, Park DW, et al. Impact of intravascular ultrasound guidance on long-term mortality in stenting for unprotected left main coronary artery stenosis. Circ Cardiovasc Interv 2009;2:167-77. [Crossref] [PubMed]
- Chen HY, Koo BK, Kassab GS. Impact of bifurcation dual stenting on endothelial shear stress. J Appl Physiol (1985) 2015;119:627-32. [PubMed]
- Bavishi C, Sardar P, Chatterjee S, et al. Intravascular ultrasound-guided vs angiography-guided drug-eluting stent implantation in complex coronary lesions: Meta-analysis of randomized trials. Am Heart J 2017;185:26-34. [Crossref] [PubMed]
- Tian NL, Gami SK, Ye F, et al. Angiographic and clinical comparisons of intravascular ultrasound- versus angiography-guided drug-eluting stent implantation for patients with chronic total occlusion lesions: two-year results from a randomised AIR-CTO study. EuroIntervention 2015;10:1409-17. [Crossref] [PubMed]
- Kim BK, Shin DH, Hong MK, et al. Clinical Impact of Intravascular Ultrasound-Guided Chronic Total Occlusion Intervention With Zotarolimus-Eluting Versus Biolimus-Eluting Stent Implantation: Randomized Study. Circ Cardiovasc Interv 2015;8:e002592. [Crossref] [PubMed]
- Shin DH, Hong SJ, Mintz GS, et al. Effects of Intravascular Ultrasound-Guided Versus Angiography-Guided New-Generation Drug-Eluting Stent Implantation: Meta-Analysis With Individual Patient-Level Data From 2,345 Randomized Patients. JACC Cardiovasc Interv 2016;9:2232-9. [Crossref] [PubMed]
- de Jaegere P, Mudra H, Figulla H, et al. Intravascular ultrasound-guided optimized stent deployment. Immediate and 6 months clinical and angiographic results from the Multicenter Ultrasound Stenting in Coronaries Study (MUSIC Study). Eur Heart J 1998;19:1214-23. [Crossref] [PubMed]
- Chieffo A, Latib A, Caussin C, et al. A prospective, randomized trial of intravascular-ultrasound guided compared to angiography guided stent implantation in complex coronary lesions: the AVIO trial. Am Heart J 2013;165:65-72. [Crossref] [PubMed]
- Ali ZA, Maehara A, Généreux P, et al. Optical coherence tomography compared with intravascular ultrasound and with angiography to guide coronary stent implantation (ILUMIEN III: OPTIMIZE PCI): a randomised controlled trial. Lancet 2016;388:2618-28. [Crossref] [PubMed]


