
Improving clinical practice in primary care for the prevention and control of noncommunicable diseases: a multi-actor approach to two regional pilot projects in Kazakhstan
Kazakhstan, like other health systems of the Commonwealth of Independent States (CIS), inherited a highly centralized, executive-style governance model for policy-making from the Soviet period (1,2). A lack of clearly defined roles and training for health management personnel, as well as frequent changes in the organizational structure of the health system, are cited among key governance bottlenecks stalling early progress in health reforms (1-3). The Government of Kazakhstan has taken important steps to redress this, evidenced by the priority weighted to organizational and managerial reforms in the 2011–2015 National Health Care Development Program Salamatty Kazakhstan. Nonetheless, countering the tradition of a top-down governance model that is characteristic to Semashko systems takes time and faces the challenge to overcome the lack of consideration previously given to the role of managers at district or facility level, and to their influence on quality of care (4,5). In effect, quality of care is predominately attributed to the role of health practitioners, to the exclusion of managers as well as other system actors (6-8).
The changing burden of disease in Kazakhstan, but also globally, is a primary ‘push factor’ for a focus on governance and quality of care at present. In Kazakhstan, health trends put a spotlight on noncommunicable diseases (NCDs) and in particular, the burden of premature mortality from cardiovascular diseases (CVDs) is significant. Kazakhstan has one of the highest rates of premature mortality due to NCDs in the WHO European Region at a rate of 648.31 deaths per 100,000 population aged 30–69 years in 2012 (9). 2012 estimates account 84% of total deaths in Kazakhstan to NCDs, of which more than half (54%) were caused by CVDs (10). Nevertheless, there is an overall downward trend in premature mortality due to the four major NCDs and if this trend continues, Kazakhstan would appear to be on track to achieve the global target of a 25% reduction in premature mortality from NCDs by 2025 (9).
Faced with such trends, there is increasing demand for both access and quality services that identify and manage high-risk individuals for CVDs. The principles of cardiovascular risk assessment and management, as one of WHO’s ‘best buys’, are already included in Kazakhstan national policies, screening programmes and clinical practice guidelines. Kazakhstan has also invested heavily in innovative technologies to deliver highly specialized heart surgeries, contributing to fewer CVD related deaths. Nevertheless, premature mortality is high and signals the need for further strengthening primary health care (PHC). A recent WHO assessment on the health system’s strength to respond to NCDs found limited use of risk scores in PHC to stratify risk or define disease management (Farrington et al., 2017, unpublished). Concerns for the quality of PHC were also raised in a 2015 study, estimating 75% of hospitalizations for hypertension in Kazakhstan could have been avoided through more effective PHC interventions (11).
In the historically centralized structures described, the sense of a clear mandate and the autonomy among health practitioners and health facility managers to take full responsibility for the population’s health outcomes and improve quality of care in Kazakhstan is in progress yet not fully cultivated. Thus, while it is widely accepted that quality of care is a reflection of system limitations and requires a system-wide response (6,12,13), there remains a persisting divide between quality improvement at the policy-level and in clinical practice.
This review describes the experience of two regional (oblast) level pilot projects in Kazakhstan implemented over a three-year period and aimed at improving NCD outcomes for CVDs and diabetes. These projects set out with a common objective and design: to tackle the dichotomy between clinical and system quality improvement efforts by translating the multifaceted nature of quality into roles and responsibilities of actors across the system. The implemented interventions and impact are described as well as relevant policy lessons for improving quality of care in other CIS countries or similar systems of centralized governance models.
Pilot design
Purpose
In 2014, the Government of Kazakhstan, together with the Ministry of Regional Development, regional Akimats (councils) and seven agencies of the United Nations present in Kazakhstan, initiated two joint programmes for development in the regions of Kyzylorda and Mangystau. The programmes shared a common aim of sustainable social, health and economic development.
In the scope of working towards sustainable health gains for both joint programmes, WHO was lead responsible agency. Specific interventions for improving clinical practice in PHC for the prevention and control of CVDs and diabetes were identified. By adopting a system’s perspective, the interventions set out to bring together services delivery actors that included: policy-makers; health facility managers; health practitioners and patients (14).
The multi-actor approach adopted is rooted in the principles of systems-thinking and multi-stakeholder engagement (6,15,16), working to instill the notion of individual yet also joint roles for quality improvement. Acknowledging these different contributions and roles and responsibilities aims to avoid over burdening health practitioners and establish a culture of quality of care where all actors see their integral role and are empowered and engaged in the process of quality improvement. Ultimately, the purpose of the pilot projects was to design an approach to bring actors together with a shared understanding for the importance of their unique perspective and contribution to quality of care rather than to prescribe roles for each actor involved.
Rationale
The design of the pilot projects reflects the following three principles. (I) Quality of care is integral to universal health coverage. There is growing recognition that poor quality of care can be a barrier to universal health coverage independent of access (4). This is increasingly reflected in global health policies (17-20). Making progress towards sustainable development, therefore, requires a move towards access that also priorities quality health services.
(II) Well-resources systems alone do not equate to improved outcomes. The capacity of services delivery systems includes also the unique processes of the services delivery function (21). Thus, while services delivery relies on the system for quality inputs, including safe medicines, a skilled workforce and effective technologies, among others, improving services delivery processes is also a relevant and critical entry point for improving quality.
And (III) quality of care is everyone’s business. Taking a system’s perspective, quality of care is the resultant of the unique role of all health system actors, including patients. Engaging individuals and applying a people-centred approach to quality improvement interventions is a relatively recent principle (18-20).
Pilot oblasts
The two oblasts of Kyzylorda and Mangystau selected as pilots represent the unique challenges of Kazakhstan’s regions that range from areas with a less favourable environment and climate to those that are naturally resource-rich. Both, nonetheless, share similar challenges of equitable health and development. These sites were designated by the Government at the outset.
Kyzylorda Oblast is situated in the southern part of Kazakhstan with a largely rural population, totalling 753,200 people [2012] (22). The region faces key challenges to sustainable health development including poor economic and social infrastructure, harsh climate conditions, high environmental and health risks caused by the Aral Sea crisis, the extensive mining industry, pesticide use and subsequent limited access to clean water and sanitation, especially in rural areas. As a consequence, its population’s health indicators, including the increasing burden of NCDs, are among the worst in the country.
Mangystau Oblast is situated in south-western Kazakhstan, east of the Caspian Sea with a population of 633,000 (23). Mangystau is a unique, natural resource-rich region of Kazakhstan, with its economy heavily dependent on oil and gas resources. The extracting industry makes up a large part of the gross regional domestic product, yet it is poorly connected to the local economy. Thus, despite its high per capita gross regional domestic product, Mangystau is a region struggling to ensure that its economic growth is reflected in human, social and health development, while also reducing social inequality. In this context, preventable differences in health status are noted especially for the prevalence of NCDs.
Approach to design of pilots
The pilot projects applied the classic framework on quality of care developed by Donabedian, making the distinction between structures, processes and outcomes (24). Table 1 illustrates this logic model and the health services delivery interventions deployed in the pilots to improving clinical practice.

Full table
The specific interventions of the pilot projects correspond to those system bottlenecks revealed by earlier studies calling for transformations that are rooted in a PHC approach and transform services delivery processes while also creating the enabling system conditions. Adopting a multi-actor and system perspective, each intervention corresponds to a specific goal and different stakeholder that collectively contribute to the quality of NCD services delivered in PHC. The interventions draw from the well-developed evidence-base and previously implemented tools and mechanisms for improving quality of care. These include: population-based planning and design (25-28); health facility strategic planning (29-31); action plans, monitoring and evaluation plans, and internal audits (32-35); and communication training (36).
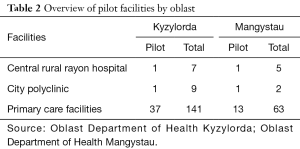
In both Kyzylorda and Mangystau, the interventions were applied at a facility-basis. The PHC network in Kyzylorda consists of seven central rural rayon hospitals and nine city polyclinics and in Mangystau as five central rural rayon hospitals and two city polyclinics. The Department of Health in each oblast selected one urban polyclinic and one central rural rayon hospital as pilot facilities as well as a sample of primary care facilities affiliated to the central rayon hospitals or city polyclinics (37 in Kyzylorda and 13 in Mangystau) (Table 2). Thus, while the interventions have put focus on primary care, the pilot design has also recognized the importance of coordination across the network of facilities locally. Importantly, training opportunities for health practitioners and facility managers took a broader approach in an effort to be inclusive and were offered to health practitioners and managers in the two regions in both pilot and non-pilot facilities.
Full table
Review methods
This review uses multiple data sources and methods to establish an overview of the development of the two pilots. The sources of information and process for collection are described as follows.
- Rapid baseline assessments. Conducted in December 2014 and February 2015, this period of initial assessments worked to detail the current context and its existing challenges. Topics included services for NCDs, management practices, and modalities of planning and budgeting in facilities in both oblasts. From these assessments, the specific interventions for the pilot projects were selected.
- Implementation plans, curriculums and other pilot-related material. Material developed for the implementation of each intervention informs their description. This includes mission reports, workshop presentations and other teaching resources.
- Mid-way joint implementation meeting and exchange of lessons learned. In December 2016, an implementation meeting convening actors from across pilot projects was organized in Almaty, Kazakhstan. The one-day event showcased the status of implementation to-date, and exchanged lessons learned for moving forward. The material presented at this event has informed this review’s findings.
- Intervention-specific evaluations. Reports for the interventions deployed were developed by external experts. These reports offer insights on the impact of interventions. This reporting includes also participant evaluations from intervention-related trainings and workshops organized.
- Final external evaluation. In September 2017, a final external evaluation of the pilot projects was conducted. In addition to the reporting described above, this evaluation included key informant interviews and focus group discussions as well as direct observations at pilot primary care facilities. Monitoring data has been collected by the Oblast Department of Health in Kyzylorda and Mangystau.
Interventions
This section describes the interventions deployed by the pilots according to the specific goals defined by the domains of outcome, output, process and input (Table 1). In summarizing the interventions, the objectives are described based on the relevant bottlenecks identified as well as the changes activated and the processes employed.
Engaging patients for resilient communities
In order to explore in-depth the issues surrounding patient engagement in health services delivery and patients’ interactions with health practitioners, fourteen focus groups were held involving 89 patients from pilot facilities. Findings from focus group discussions signalled ineffective health practitioner communication, including explanations, and poor attitudes among health practitioners towards patients, contributing to poor adherence to treatment recommendations and low satisfaction with services. Based on these results, communication trainings to develop the skills of health practitioners was prioritized and applied to both pilot and non-pilot facilities across the two oblasts.
Communications training
Communication trainings aimed to improve practices in building trust in the interactions between health practitioners and patients and develop skills including active and empathic listening, conflict resolution and managing aggressive patients, establishing relationships with patients and motivating patients for health behavior changes. These trainings featured tailored modifications for the context of Kazakhstan, including a greater emphasis on provider introductions and nonverbal communication with patients, demonstrating listening and understanding through verbal and nonverbal behaviors, responding to and preventing aggressive behavior, checking for patient understanding and adherence, and self- and peer-assessments to improve communication practices over time.
Empowering health practitioners for quality improvement
This component of the pilot projects set out with the objective to establish mechanisms for continuous quality improvement and contribute to a culture of learning among health practitioners. The introduction of population-based cardiovascular risk stratification and management through this component was a key pillar for clinical practice changes of the pilot project. This focus responds to the identified limitations of quality indicators that were found in baseline studies to potentially mislead on the performance of health practitioners and contribute to a punitive approach for performance monitoring. The interventions employed also respond to challenges identified for internal audit and quality control mechanisms to allow for flexibility in services delivery according to the needs of patients.
Clinical quality improvement action plans
After a series of capacity-building trainings and workshops, each pilot facility was tasked to establish clinical quality improvement teams. External experts supported each team to conduct a root-cause analysis of key bottlenecks and develop action plans on quality improvement with an aligned monitoring and evaluation framework. These plans were designed to include as a minimum: shared responsibilities; milestones based on implementation of cardiovascular risk assessment; and disease management with a focus on improving integration within the facility and with other levels of care.
Audits and supportive supervision
Each pilot facility developed and introduced an internal self- and peer review system. During implementation, a series of supportive supervision visits were conducted by international and local experts. Meetings for sharing experiences among health practitioners and between the two pilot regions were also organized. External monitoring results and earlier baseline self-monitoring results have been discussed with the clinical quality improvement teams in order to identify lessons learned to better inform and fine-tune their respective action plans.
Quality control and feedback
A call centre has been established to provide information about the ‘Support and Internal Control Service’ as well as a ‘hotline service’ on urgent medical issues. The introduction of call centres extends beyond pilot facilities following a Ministry of Health decree (prikaz) for their creation. Information on the Support and Internal Control Service is also provided on the website of the pilot facilities and in all public places at outpatient clinics.
Enabling facility managers for responsive services
This component of the pilot projects targeted facility managers, but also planners and policy-makers, in the course of introducing strategic planning in pilot facilities. To identify gaps in current management practices, a rapid assessment of pilot facilities in both oblasts was carried out. This assessment signalled most facility managers had limited knowledge and experience in strategic planning including services delivery, human resources and financial management planning. As such, support to develop strategic facility plans, based on an analysis of population needs, the local context and in alignment with national health policies, was prioritized.
Strategic facility plans
A hands-on training on strategic facility planning was designed and targeted to Oblast Health Department planners and health facility managers from rayon hospitals and polyclinics. Two-day trainings were carried out in both regions for not only pilot facilities but also other facilities that the Oblast Health Departments identified. Through a set of sessions that combined concepts and practices, the participants were guided to develop their own strategic facility plan following a stepwise approach: (I) knowing your population; (II) adapting services; (III) aligning health system enablers; (IV) managing change; (V) developing human resource plans; (VI) financial planning and (VII) monitoring and evaluating performance.
Enhancing policy-makers for evidence-based decisions
Baseline interviews with senior health management and policy-makers in the two oblasts indicated their awareness and motivation towards adopting modern approaches to public health and adapting models of care to transform the provision of services towards a patient-centred approach that is responsiveness to the population’s needs. Doing so, highlighted the importance of adopting an evidence-based approach to public health practices that demonstrate an understanding of the causes of NCDs, epidemiological patterns and their risk factors and promoting the use of effective interventions (37).
Population-based planning and design
In order to share good practices for organizing population-based, integrated health services delivery and innovative ways of using health information systems for this purpose, a study visit was organized for a delegation of senior health management and policy-makers from the two pilot oblasts to Venice, Italy, and Barcelona, Spain. Meetings with regional health authorities and visits to hospital and primary care facilities provided an opportunity to learn about good regional practices in PHC and innovative tools for promoting integration between primary, hospital, and social care, as well as community health strategies, population health management tools and examples of pooling district-population data to inform health planning. The study visit demonstrated the role of indispensable elements required for constructing a successful integrated services model in Kazakhstan for NCDs such as: using stratification models for assessing population needs; developing a shared outcome framework (joint responsibility and accountability); aligning incentives and a shared vision about the use of resources; and developing a shared electronic health and social record.
Discussion
Despite an understanding of the importance for differentiated roles and responsibilities in working towards quality of care (4,6,38), the implementation of quality improvement initiatives has continued to predominantly target individual actors and single interventions. In the field of integrated care this has been attributed to the methodological limitations to define, measure and evaluate complex interventions (39). As a consequence, implementation research that adopts a multi-actor, multi-intervention approach for improving quality of care has lagged behind more analytical progress.
However, the significance of a system’s perspective in practice for improving quality of care is especially relevant in the context of NCDs. In 2010, the WHO Package of Essential Noncommunicable Disease Interventions (WHO PEN) (40)—an innovative and action-oriented response for the prevention and control of NCDs—made progress in strengthening this link between a prioritized set of cost-effective interventions and their quality implementation. The discourse on quality of care has also evolved and sophisticated in recent years. Current momentum includes a global WHO initiative on national quality policy and strategy (39), putting emphasis on multi-stakeholder engagement as a core element of delivering on national health objectives.
This review has attempted describe the approach to improving clinical practice in PHC for the prevention and control of CVDs and diabetes in two regional pilot projects in Kazakhstan. Since the pilots were first introduction in 2014, Kazakhstan has continued to prioritize NCDs, notable in the National Health Program “Densaulyk” for 2016–2019 aimed at implementing social health insurance, public health services and integrated PHC and guided by WHO recommended NCD indicators.
The pilot projects described here reinforce the WHO PEN model, by adopting a system’s perspective for the delivery of NCDs interventions based on a PHC approach. That is, the pilot projects by design have promoted PHC-led interventions, yet reinforced this through system-enabling conditions for quality improvement (41). The relevance of overcoming implementation challenges to adopt a multi-actor approach to quality improvement is found especially relevant in systems of traditionally centralized governance models like the case of Kazakhstan.
Following the three-year implementation period for the interventions described, the following changes are observed.
Improving CVD and diabetes services
Prior to the pilot projects, screening coverage for circulatory diseases and diabetes in both pilot and non-pilot sites was reportedly high, consistently above 90% for attached population according to 2014 data of the respective Oblast Departments of Health.
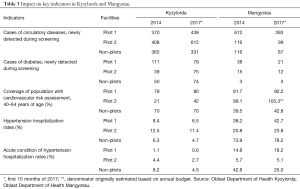
Table 3 summarizes key services delivery sensitive indicators in both pilot and non-pilot sites of the two oblasts, comparing 2014 and the first 10 months of 2017.
Full table
In Kyzylorda, pilot facilities showed a consistent increase of newly detected circulatory diseases and diabetes cases. Hospitalization rates for hypertension and acute conditions of hypertension—as a key indicator of the performance of PHC—show a consistently decreasing trend. Interestingly, the trends observed apply to both pilot and non-pilot facilities; with the positive trend more pronounced in the pilot health facilities. The consistent changes in pilots and non-pilots can be attributed, in part, to the inclusive approach taken to the interventions described as workshops and trainings extended to actors across the whole oblast, reaching actors beyond the pilots. It is also noted that the period of implementation for the pilot projects paralleled a number of actions country-wide that worked to prioritize NCDs, including the implementation of the national health program.
In Mangystau, overall, the trends observed are less consistent when comparing pilots with non-pilot facilities. For instance, hospitalization rates for hypertension and acute conditions of hypertension in Mangystau show slightly increased rates. Besides the level of development of the health information system, this can be attributed to a number of causes. These include differences in approaches to managing hypertension in PHC. Health practitioners in Mangystau report a tendency to refer patients to hospital ‘to avoid complications’ while in Kyzylorda patients are referred only when assessments determine it is not possible to provide care in PHC. It is also noted that the position of Head of Oblast Health Department was vacant from 2016, with possible implications to data collection processes and accuracy. Furthermore, in Kyzylorda, where positive trends are clear, a dedicated local coordinator supported the implementation of the project while this was not the case in Mangystau. In Mangystau pilot facility 2, the coverage of the population with cardiovascular risk assessment increased up to 105.3%. This can be explained by the changes in the planning processes. In 2017, emphasis was placed on the use of denominators estimated based on target population rather than budgets resulting in an increased over 100%.
Developing a shared understanding for quality of care
Overall, through the multi-actor, multi-intervention approach applied, there appears progress towards a shared understanding and sense of ownership for improving service quality. This can be credited to the varied interventions that together generated a regular dialogue on quality of care, worked to instill an appreciation for the importance of patient-centred care and developed a tangible understanding for quality through the measurement of indicators and their use to inform and improve performance.
The progress made to develop an appreciation for quality is evidenced by a number of facility-led innovations. For example, facilities initiated a number of clinical quality improvement mechanisms like a system of patients’ triage and an electronic queue management system, ‘WhatsApp’ groups to improve the communication between health practitioners, logbooks that resulted in ensuring continuous monitoring of patients’ health status after discharge from hospital and ‘passports’ for facility catchment areas in order to assign newly detected patients to disease groups and to ensure free prescriptions were initiated.
The development and implementation of quality improvement action plans in facilities also resulted in a number of organizational changes for the coordination and integration of approaches. In general, these efforts worked to adapt national protocols, such as patient pathways for screening programmes and approaches for implementing population stratification for cardiovascular risk assessment, to the local context.
Taken together, the interventions fostered a collective understanding for quality of care and created a more conducive learning process for health practitioners and managers while also establishing a team spirit for achieving goals jointly. The capacity for clinical quality improvement generated has also allowed for clinical quality improvement teams to transfer this understanding and skills to other clinical areas such as women and child health, tuberculosis and HIV services.
Appreciating the complementarity of individual roles in working towards improved population health
From the perspective that ‘everyone has a role to play’ in working towards quality of care, clear progress was made in developing an appreciation for the varied yet complimentary roles of different actors. Through the trainings and workshops awareness for these different actors was achieved; seen as a first step to facilitating joint efforts.
The final evaluation finds as a result of interventions described, an understanding for strategic planning in pilot PHC facilities in both regions improved. Moreover, the organizational capacity and responsiveness to public needs has improved.
The implementation of theses pilots also ran alongside national debates for improving governance and accountability arrangements towards the improved integration of health services and public health. In order to improve the public health and system’s response to NCDs, a new decree was issued on “Further improvement of the public administration system of the Republic of Kazakhstan” (No. 412), in January 2017. Its focus on detailing roles and responsibilities of actors in the health sector is well aligned with the discussions and approach generated through the pilot projects.
Establishing a culture of exchanging ideas and practices
As part of implementation, various opportunities to meet and exchange experiences within pilot oblasts but also across and with national representatives were introduced. Mid-way through implementation, for example, a 1-day event was organized to bring together actors engaged in the pilot oblasts to share and discuss their experiences. Participants also included representatives from Rayons outside of the pilots yet leading innovative practices. The unique opportunity this event created to exchange practices with one another is illustrative of concrete steps towards a culture of learning and feedback.
As part of implementation, the opportunity for participants to visit other countries and learn and exchange practices was also employed in a similar spirit of learning and improvement. From individual evaluations, participants flagged the relevance of the different applications they were exposed to, such as techniques for population stratification, management of poly-pharmacy patients, innovative systems for patient triage and use of digital services to increase patient engagement.
The principles of continuous performance improvement are most inherent to the practice of clinical quality improvement teams within facilities that observed an improvement in the regular involvement of practitioners and appreciation for teams as ‘common practice’.
Practical implications
The multi-actor, multi-intervention approach adopted here is found overall an effective model to improving quality of clinical practice while also taking on the rigidity of systems, particular to CIS countries, to tackle NCDs. In considering replicating this model, the following contextual factors are noted, having contributed to the success but also challenges of implementation.
Factors contributing to the overall successful implementation in the two oblasts are recognized to include: the continuous political support of the Oblast Departments of Health in Kyzylorda and Mangystau; the dedication and commitment of facility managers to changes; the openness and readiness of all actors to learn and improve their practices; and existing mechanisms to measure and compare results based on common indicators.
Challenges to the effective implementation of the pilot projects are also recognized and offer lessons for similar efforts. For example, some key interventions of the pilots have been lost due to the abundance of existing national regulations. Baseline assessments consistently signalled the existing regulatory framework includes an array of decrees and rules and is overly prescriptive in the areas of service delivery, staffing and financial management, leaving little space to exercise managerial and clinical autonomy. This challenge highlights the importance of protecting pilot projects with exemptions from existing reporting requirements and stimulating them with opportunities for improvements to allow the space for innovation.
Ultimately, the changes sought, including improving outcomes through the prevention of NCDs but also establishing a cultural change that promotes quality improvement, takes time. Finally, while the pilots have targeted services delivery improvements, the aligned system conditions are needed to realize sustained transformations. In the case of developing managerial competences for example, this becomes increasingly pertinent as the government of Kazakhstan intends to foster competition in health services delivery and introduce a single purchaser through a mandatory social health insurance scheme next year (Law No. 405-V 2015, with amendments and additions as of June 30, 2017) (42). Investing in the future health workforce with the skills for strategic planning and employing population-based strategies can support managerial and clinical autonomy in working towards better health outcomes.
Conclusions
This review has attempted to detail the experience of improving quality of NCD services in PHC in two oblast level pilot projects in Kazakhstan implemented over a 3-year period. Drawing from the well-established notion that improving quality of care demands a system’s focus and in effect, relies on multiple actors and interventions applied synergistically, the design of the pilot projects sought to realize this in practice. With a focus on improving outcomes for NCDs, the pilot projects have adopted a PHC approach. Attention put to ensuring all actors have a clear sense of their role and responsibility for improving quality has proven effective in the unique context of Kazakhstan and offers a relevant model for other countries of similar systems of traditionally centralized governance models.
Acknowledgements
This work has benefited from the technical expertise and collaborations with a number of experts. The pilot projects were managed under the oversight of the WHO Representative to Kazakhstan, Melita Vujnovic (WHO Regional Office for Europe), together with the Division of Health Systems and Public Health Directed by Hans Kluge (WHO Regional Office for Europe).
In addition to the authors Angela Ciobanu (WHO Regional Office for Europe), Brett Craig (St Louis College of Pharmacy), David Gzirishvili (Consulting Group Curatio Ltd.), Aizhan Kapysheva (Columbia University), Tino Marti (WHO Regional Office for Europe), Shanthi Mendis (formerly, WHO), David Sulaberidze (Consulting Group Curatio Ltd.), Altynai Satylganova (WHO Regional Office for Europe) and Laura Utemisova (project implementation, WHO Country Office in Kazakhstan) contributed at varied stages to baseline assessments, the development or implementation of interventions. Symon Lord conducted the final evaluation for the pilot projects. Data for monitoring has been provided by the Oblast Department of Health in Kyzylorda and Mangystau. This work is credited to all those individuals working in the two pilot oblasts.
The pilot projects were funded by the Government of Kazakhstan and United Nations agencies present in Kazakhstan as part of the joint programmes: “Expanding opportunities of the Mangystau region in achieving sustainable development and socio-economic modernization” and “Improving the welfare and quality of life in the Kyzylorda region through innovative approaches to delivering economic, social and environmental services to the local population, including those most vulnerable.” The WHO Regional Office for Europe was lead coordinating agency for the two pilot projects described.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Rechel B, Richardson E, McKee M. Trends in health systems in the former Soviet countries. Observatory Studies Series. Copenhagen: WHO Regional Office for Europe, 2014.
- Katsaga A, Kulzhanov M, Karanikolos M, et al. Kazakhstan Health Review. Health Systems in Transition Copenhagen: WHO Regional Office for Europe 2012:14.
- McKee M, Figueras J, Chenet L. Health sector reform in the former Soviet Republics of Central Asia. Int J Health Plann Manage 1998;13:131-47. [Crossref] [PubMed]
- Hanefeld J, Powell-Jackson T, Balabanova D. Understanding and measuring quality of care: dealing with complexity. Bull World Health Organ 2017;95:368. [Crossref] [PubMed]
- Balabanova D, Mills A, Conteh L, et al. Good health at low cost 25 years on: lessons for the future of health systems strengthening. Lancet 2013;381:2118-33. [Crossref] [PubMed]
- World Health Organization. Quality of care: a process for making strategic choices in health systems. Geneva: World Health Organization, 2006.
- World Health Organization. Guidance on developing quality and safety strategies with a health system approach. Geneva: World Health Organization, 2008.
- WHO Regional Office for Europe. A brief synopsis on patient safety. Copenahgen: WHO Regional Office for Europe, 2010.
- WHO Regional Office for Europe. European health for all database. Copenhagen: WHO Regional Office for Europe, 2017. Available online: http://data.euro.who.int/hfadb/
- World Health Organization. Noncommunicable diseases (NCD) country profiles - Kazakhstan. Geneva: World Health Organization, 2014.
- WHO Regional Office for Europe. Ambulatory care sensitive conditions in Kazakhstan. Copenhagen: WHO Regional Office for Europe, 2015.
- Donaldson MS, Corrigan JM, Kohn LT. To err is human: building a safer health system. National Academies Press, 2000.
- Institute of Medicine (US) Committee on Quality of Health Care in America. Crossing the quality chasm: a new health system for the 21st century. Washington (DC): National Academies Press (US), 2001.
- WHO Regional Office for Europe. Strengthening people-centred health systems in the WHO European Region: framework for action on integrated health services delivery. Copenhagen: WHO Regional Office for Europe, 2016.
- World Health Organization. Everybody’s business: strengthening health systems for improved health outcomes: WHO’s framework for action. Geneva: World Health Organization, 2007.
- Adam T, de Savigny D. Systems thinking for strengthening health systems in LMICs: need for a paradigm shift. Health Policy and Planning 2012;27:iv1-iv3. [Crossref] [PubMed]
- WHO Regional Office for Europe. Health 2020: a European policy framework supporting action across government and society for health and well-being. Copenhagen: WHO Regional Office for Europe, 2013.
- World Health Organization. Global strategy on people-centred and integrated health services. Geneva: World Health Organization, 2016.
- WHO Regional Office for Europe. Priorities for health systems strengthening in the European Region 2015-2020: walking the talk on people centredness. Copenhagen: WHO Regional Office for Europe, 2015.
- Resolution: Strengthening people-centred health systems in the WHO European Region: framework for action on integrated health services delivery (2016).
- Tello J, Barbazza E. Health services delivery: a concept note. Copenhagen: WHO Regional Office for Europe.
- Akimat of Kyzylorda Oblast. Official internet-resource of the Akimat of Kyzylorda Region 2017. Available online: https://e-kyzylorda.gov.kz/?q=en
- The Mangystau region Akim’s administration. The Mangystau Region - Official internet resource of the region akimat. 2017. Available online: http://mangystau.gov.kz/en
- Donabedian A. The definition of quality and approaches to its assessment. Explorations in quality assessment and monitoring 1980. Donabedian A. Ann Arbor, MI: Health Administration Press, 1980.
- Suter E, Oelke ND, Adair CE, et al. Ten key principles for successful health systems integration. Healthc Q 2009;13:16-23. [Crossref] [PubMed]
- Balicer RD, Shadmi E, Lieberman N, et al. Reducing health disparities: strategy planning and implementation in Israel's largest health care organization. Health Serv Res 2011;46:1281-99. [Crossref] [PubMed]
- Basque Government. A strategy to tackle the challenge of chronicity in the Basque Country. Basque Country: Basque Government Department of Health and Consumer Affairs, 2010.
- Hutchings HA, Evans BA, Fitzsimmons D, et al. Predictive risk stratification model: a progressive cluster-randomised trial in chronic conditions management (PRISMATIC) research protocol. Trials 2013;14:301. [Crossref] [PubMed]
- Wendt D, Bouchet YSL, Nanda L, et al. Health system rapid diagnostic tool. Durham, NC: FHI 2013;360.
- Brinkerhoff DW, Wetterberg A. Performance-based public management reforms: experience and emerging lessons from service delivery improvement in Indonesia. International Review of Administrative Sciences 2013;79:433-57. [Crossref]
- Bohmer RM. Leading clinicians and clinicians leading. N Engl J Med 2013;368:1468-70. [Crossref] [PubMed]
- Davis DA, Mazmanian PE, Fordis M, et al. Accuracy of physician self-assessment compared with observed measures of competence: a systematic review. JAMA 2006;296:1094-102. [Crossref] [PubMed]
- Merkur S, Mladovsky P, Mossialos E, et al. Do lifelong learning and revalidation ensure that physicians are fit to practise? Copenhagen: WHO Regional Office for Europe, 2008.
- Filipe HP, Silva ED, Stulting AA, et al. Continuing professional development: Best practices. Middle East Afr J Ophthalmol 2014;21:134. [Crossref] [PubMed]
- Shaw CD, Kalo I. A background for national quality policies in health systems. Geneva: World Health Organization, 2002.
- Ferrer L. Engaging patients, carers and communities for the provision of coordinated/integrated health services: strategies and tools. Copenhagen: WHO Regional Office for Europe, 2015.
- Diem G, Brownson RC, Grabauskas V, et al. Prevention and control of noncommunicable diseases through evidence-based public health: implementing the NCD 2020 action plan. Glob Health Promot 2016;23:5-13. [Crossref] [PubMed]
- Legido-Quigley H, McKee M, Nolte E, et al. Assuring the quality of health care in the European Union: a case for action. Copenhagen: European Observatory on Health Systems and Policies, 2008.
- Nolte E, Pitchforth E. What is the evidence on the economic impacts of integrated care? Copenhagen: WHO Regional Office for Europe, 2014.
- World Health Organization. Package of essential noncommunicable (PEN) disease interventions for primary health care in low-resource settings. Geneva: World Health Organization, 2010.
- Narain JP. Integrating services for noncommunicable diseases prevention and control: Use of primary health care approach. Indian J Community Med 2011;36:S67-71. [Crossref] [PubMed]
- Law of the Republic of Kazakhstan No. 405-V “On compulsory social health insurance” (with amendments and additions as of June 30, 2017). 2015. Available online: https://online.zakon.kz/Document/?doc_id=32908862#pos=1;-96


