Kounis syndrome induced by amoxicillin following vasospastic coronary event in a 22-year-old patient: a case report
Introduction
There has been a noticeable increase in the reports of incidence of Kounis syndrome (KS) during the last decade (1,2). KS refers to the concurrent occurrence of acute coronary syndrome and acute coronary spasm in the presence of hypersensitive reactions and is more common in middle aged men (3). Although there is no documented epidemiological data, the spectrum of KS due to various causative agents has been constantly evolving. Amoxicillin, a potential beta-lactam antibiotic, is generally associated with possible adverse events like erythema, angioedema, and hypersensitive reactions. Apparently, such incidence of cardiovascular events in young patients after amoxicillin administration is a rare finding and yet to be established as a clinical fact. The misdiagnosis of KS as a relevant infarct is an unavoidable clinical challenge. Despite increased instances of the syndrome, there are no published guidelines pertinent to the diagnosis and treatment of KS in young patients. Moreover, the amount of literature and data available are insufficient to establish the exact pathogenesis and spectrum of its causative substrates. Herein, we present the case of a young male patient with KS triggered by amoxicillin administration.
Case presentation
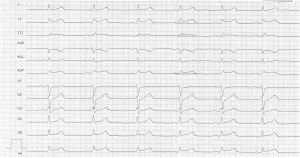
A 22-year-old man with acute retrosternal pain and chest tightness was admitted to the Marien Hospital, Herne, Germany. Before arrival, the patient was diagnosed with acute tonsillitis and administered with a single dosage of amoxicillin. Within an hour of the dosage, the patient was observed to have ST elevations in II, III, aVF, V5, and V6 (0.2 mV) in electrocardiogram (ECG) (Figure 1) and positive troponin (300 pg/dL). Following this critical observation, the patient was transferred to the emergency unit with a tentative diagnosis of ST elevation myocardial infarction (STEMI).
The routine clinical investigations including a repeat ECG along with a blood sample test were carried out in the emergency unit. The vital signs showed stable blood pressure (135/88 mmHg), pulse rate (72 beats/min), respiratory rate (16 breaths/min), pulse oximetry (100% on room air), and temperature (36.6 °C). Except for tender throat and white patches over the tonsils there was no relevant pathological cardiovascular finding. The standard 12-lead ECG showed ST elevation. Elevated troponin and creatine kinase (CK) (troponin 550 pg/mL; CK 315 IU/L) levels were detected in the blood sample, which confirmed the provisional diagnosis pertinent to ECG findings. In orienting echocardiography, a normal functioning heart with preserved ejection fraction could be observed.
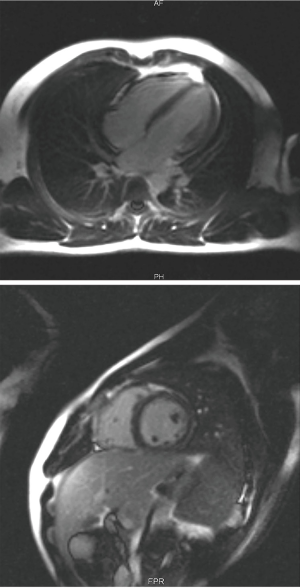
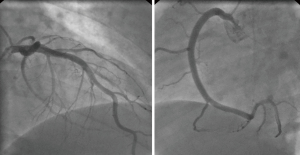
A heparin bolus was administered, and the patient was transferred for emergency cardiac catheterization. Percutaneous coronary angiography was immediately performed. Apparently, the epicardial arteries showed a normal flow status, and preliminary diagnosis of acute infarct was found to be subverted (Figure 2). Right after the conduction of coronary angiography a short monitoring in the intermediate care unit was done; there after the patient was transferred to the indoor ward in a stable cardiopulmonary status.
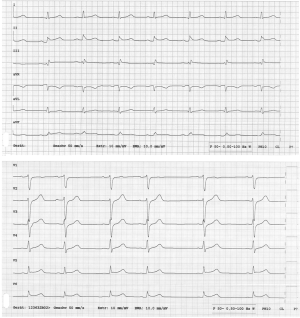
A single antiplatelet therapy with 100 mg acetylsalicylic acid was included into his daily drug regimen. Clinical examinations and laboratory findings during his next indoor-stay and regular follow-ups showed that the patient was symptom-free with continuously decreasing cardiac markers to normal level. The successive 12-lead ECG showed the restoration of ST elevation to baseline (Figure 3).
In the backdrop of a pertinent tonsillitis and above diagnostic result, myocarditis was considered as a differential diagnosis. Cardiac MRI performed on him failed to establish any signs of active myocarditis (Figure 4). Additionally, the left ventricular ejection fraction (LVEF) was preserved and there were no signs of morphological abnormalities in the heart.
Except for a short history of smoking for about 3–4 months, we could not find any other major cardiovascular risk factor in the patient. In the absence of any other relevant clinical findings after stopping amoxicillin, the profound STEMI was suggested to be due to acute vasospastic episode triggered by hypersensitive reaction to amoxicillin. Diagnosis of KS was established and the patient was discharged in a stable condition after 5 days. A telephonic follow-up after a week revealed good recovery of the patient.
Discussion
There have been exponentially increased reports of myocardial infarction with a normal epicardial artery in coronary angiography in the last decade (4). This finding, especially in young patients, coincides mainly with congenital coronary anomaly, coronary artery spasm, or drug induced scenarios. Although this condition has been rarely described in young adolescents, our literature review reveals few cases of patients including a 13- and 16-year-old children to be diagnosed with KS triggered by amoxicillin compound (5,6). It’s noteworthy that a number of children has also been reported with a progression to allergic myocardial infarction against various form of allergens (7).
There are no widespread studies available till date on the presence of acute coronary syndrome secondary to coronary vasospasm triggered by drug-induced hypersensitivity. Apparently, like many other agents, a formal connection of cardiovascular events triggered by hypersensitivity to amoxicillin is yet to be established.
A recent analysis of individual case reports of KS from the international pharmacovigilance databases VigiBase™ and EudraVigilance (3,8,9) has revealed that nonsteroidal anti-inflammatory drugs (NSAID) most frequently trigger KS (31 cases, 60.7%), followed by drugs for cardiovascular disease (10 cases, 19.6%), antibiotics (9 cases, 17.6%), and anesthetics (5 cases, 9.8%). Amongst the 16 reported cases of antibiotic-induced KS, a total of 6 cases were related to amoxicillin/clavulanic acid. Although this analysis convincingly summarizes the broadened spectrum of KS, it fails to explain the reason why amoxicillin is reported to be the most frequent KS triggering drug amongst the antibiotics inducing KS.
While the exact pathogenesis of KS remains ambiguous, the best given explanation of ischemia due to allergic insult is secondary to the release of mast-cell mediated inflammatory substances including histamine, tryptase, chymase, platelet-activating factor, cytokines, prostaglandins, and leukotriene synthesis. These substances trigger endothelial dysfunction, leading to coronary vasospasm (10).
The diagnosis and treatment of KS can be challenging, requiring simultaneous attention to both cardiac and anaphylactic pathophysiologies. The clinical, laboratory, and ECG features of KS with cardiovascular symptoms of normal epicardial coronary artery are indistinguishable from those detected in majority of patients with acute myocardial infarction (AMI) and atherosclerotic coronary heart disease.
The main diagnostic approach of KS includes history, clinical manifestation, and screening tests. Clinical manifestations of KS are variable and the reasons behind the variability are still unknown. Frequently mentioned biological tests for screening include an increased serum tryptase level, selective spasm test with acetylcholine or ergonovine and skin-prick allergic test. The specificity of these biological tests is still a topic for research and therefore are not accepted or practiced worldwide.
In the present case, myocardial injury in the patient occurred in the absence of an anaphylactic reaction. Tryptase test was not performed as there was a time interval of more than 2 hours between the occurrence of initial symptoms and first presentation of the patient at the hospital. It is to be noted that the best time for the first blood samples for tryptase measurement is half an hour after the initial symptoms and 30 minutes thereafter during the following 2 hours (11).
Furthermore, a spasm provocation test could not be done during the emergently performed coronary angiography. On the other hand, the provocation test results could be influenced by several other factors. Therefore, evidence regarding coronary spasm with this test would not have established a direct relationship between vasospastic potential of amoxicillin.
An intradermal skin test has high sensitivity but very low specificity. But the value of skin test as a diagnostic measure remains unclear as a systemic hypersensitivity reaction can occur anytime without any primary cutaneous manifestation (12). Moreover, with the unknown safety profile and already reported cases of skin test-induced KS (13), we chose not to perform it as the odds of inducing another acute cardiovascular episode with amoxicillin skin test would have been difficult to eliminate.
In the present case, a possible local effect of amoxicillin could be inferred on the basis of the triggered adverse cardiovascular events within a short period of its single-dose administration and absence of coronary lesions on the angiogram. We assumed that the triggered vasospasm without any apparent allergic reaction could be due to the direct action of amoxicillin on the coronary mast cells. A drug-induced KS type 1 variant could be indicated in this case based on the sole cardiac involvement that reflects another aspect of allergic reactions in KS, especially in young patients with no major cardiovascular risk factors.
Minimum awareness of potential cardiovascular risk factors of several drugs is necessary to avoid misdiagnosis of KS as AMI with culprit lesion and unnecessary coronary intervention. The treatment strategy also requires a thoughtful use of several common drugs as there are no major guidelines for the treatment approaches in drug-induced KS. Multiple reported cases in the literature showed that frequent use of acute chest pain drugs like morphine, beta-blockers, and epinephrine aggravated anaphylactic reactions (4,14). Prudent treatment strategy should be developed to eliminate the allergic insult of aggravating agent.
It is a matter of debate whether AMI in young patients, in the setting of allergic insult, should be reclassified into a separate group with individualized guidelines for the treatment approaches of KS. But it is undeniable that increasing number of case reports of KS definitely warrants for widespread study and analysis.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: As per the university hospital policy, all of the patient’s data are used with the consent of the patient.
References
- Kounis NG, Zavras GM. Histamine-induced coronary artery spasm: the concept of allergic angina. Br J Clin Pract 1991;45:121-8. [PubMed]
- Kounis NG. Coronary hypersensitivity disorder: the Kounis syndrome. Clin Ther 2013;35:563-71. [Crossref] [PubMed]
- Abdelghany M, Subedi R, Shah S, et al. Kounis syndrome: A review article on epidemiology, diagnostic findings, management and complications of allergic acute coronary syndrome. Int J Cardiol 2017;232:1-4. [Crossref] [PubMed]
- Akgullu C, Eryilmaz U, Gungor H, et al. Myocardial infarction secondary to morphine-induced Kounis syndrome. Herz 2014;39:874-6. [Crossref] [PubMed]
- Biteker M, Duran NE, Biteker FS, et al. Kounis syndrome secondary to amoxicillin/clavulanic acid use in a child. Int J Cardiol 2009;136:e3-5. [Crossref] [PubMed]
- Ilhan E, Akbulut T, Gürsürer M. An underdiagnosed syndrome; Kounis syndrome secondary to amoxicillin/clavulanic acid use in a 16 year-old child. Int J Cardiol 2013;167:e90-1. [Crossref] [PubMed]
- Biteker M, Duran NE, Biteker FS, et al. Allergic myocardial infarction in childhood: Kounis syndrome. Eur J Pediatr 2010;169:27-9. [Crossref] [PubMed]
- Renda F, Landoni G, Trotta F, et al. Kounis Syndrome: An analysis of spontaneous reports from international pharmacovigilance database. Int J Cardiol 2016;203:217-20. [Crossref] [PubMed]
- Renda F, Marotta E, Landoni G, et al. Kounis syndrome due to antibiotics: A global overview from pharmacovigilance databases. Int J Cardiol 2016;224:406-11. [Crossref] [PubMed]
- Kounis NG. Kounis syndrome (allergic angina and allergic myocardial infarction): a natural paradigm? Int J Cardiol 2006;110:7-14. [Crossref] [PubMed]
- Kounis NG. Serum tryptase levels and Kounis syndrome. Int J Cardiol 2007;114:407-8. [Crossref] [PubMed]
- Andrews ID, Scheinman P. Systemic hypersensitivity reaction (without cutaneous manifestations) to an implantable cardioverter-defibrillator. Dermatitis 2011;22:161-4. [PubMed]
- González-de-Olano D, Gandolfo-Cano M, Mohedano-Vicente E, et al. Kounis syndrome following the performance of skin test to amoxicillin. Int J Cardiol 2014;174:856-7. [Crossref] [PubMed]
- Goddet NS, Descatha A, Liberge O, et al. Paradoxical reaction to epinephrine induced by beta-blockers in an anaphylactic shock induced by penicillin. Eur J Emerg Med 2006;13:358-60. [Crossref] [PubMed]