
Is dedicated implantation tool set really needed for permanent His bundle pacing?
Introduction
In recent years there has been a growing interest in permanent His bundle pacing (HBP) due to its ability to simulate physiological electrical conduction and to prevent the dyssynchrony caused by the right ventricular (RV) pacing. From the first description in 2000 (1), numerous reports and studies on permanent HBP have been published showing a good success rate and improved patients outcomes (2). All of them have considered the use of dedicated pacing lead and delivery sheaths as a cornerstone of the implantation technique. This paper describes a successful attempt of permanent HBP using a standard active fixation lead positioned without delivery system.
Case report (Figures 1,2)
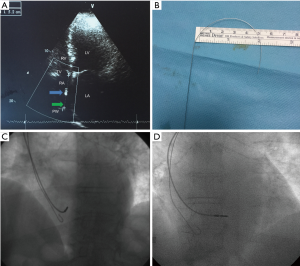
A 76-year-old female was indicated for permanent dual-chamber pacemaker implantation due to sick sinus syndrome. Baseline ECG parameters were: rest heart rate 45 beats/min, QSR axis 30°, PQ interval 196 ms, and QRS duration 120 ms. Before the procedure, at the echocardiographic examination (apical 4 chamber view at end-systolic phase) we found a distance of 5.2 cm between the inferior vena cava orifice in posteromedial region of right atrium (identified using color flow imaging) and the base of the septal cuspid of tricuspid valve (Figure 1A). This distance was considered comparable to that between the superior vena cava orifice and the base of the septal cuspid of tricuspid valve, as the two venous orifices are almost anatomically specular along a virtual vertical line.
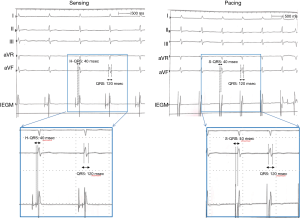
Following the left cephalic venous access, we inserted a standard bipolar 5.6-F lead (Solia S 60, BIOTRONIK SE & Co, Berlin, Germany) for permanent cardiac pacing. This lead has an active fixation system with extendable screw. In order to reach the His bundle region we pre-shaped a stylet using the length of 5.2 cm as reference for the J curve (Figure 1B). Using this stylet we quickly delivered the pacing lead above the tricuspid valve near the His bundle, which we were able to map in unipolar configuration without any delivery sheath and prior to active fixation (Figure 1C). Intracardiac electrograms confirmed the lead positioning on the His bundle and the selective HBP during both unipolar and bipolar configuration of pacing according to recent recommendations (3). Pacing stimulus to QRS onset interval (S-QRS) was equal to the native His-QRS interval (H-QRS), and the morphology and duration of the paced QRS was the same as the native QRS (Figure 2).
The lead was then screwed in that location with the active fixation system and its stability was verified removing the inner stylet (Figure 1D). We found single capture thresholds (3): 2.0 V at 1 ms and 1.2 V at 1 ms in bipolar and unipolar configuration, respectively, with stable selective His bundle capture. The time procedure was 40 minutes and the patient was discharged the next day without any acute complications.
Discussion
This case describes the feasibility of selective HBP with a standard bipolar lead positioned through cephalic access without a dedicated delivery sheath. The use of a stylet pre-shaped on an echocardiographic reference allowed a successful procedure without specific technical difficulties.
So far there is only one commercially available system for HBP: a dedicated 4-Fr, lumenless lead with an exposed screw (SelectSecure model #3830, Medtronic Inc., Minneapolis, MN) and a 7-Fr fixed or 8.5 Fr deflectable delivery sheath (SelectSite sheath, Medtronic Inc., Minneapolis, MN). In the recent literature this implantation tool set has been considered as the gold standard to perform HBP (4,5). In our case, we used a standard pacing lead, which has wider electrically active surface (4.5 vs. 3.6 mm2) and different active fixation system (extendable vs. exposed screw). These differences in lead design may provide some possible advantages: simplified detection of the His signal, possible electrophysiology-mapping prior to screw exposition avoiding additional myocardial lesions and less complicated transvenous lead extraction, in case of infection or lead malfunction. These advantages may be considered very useful in case of patients with anatomical anomalies in the right atrium due to previous surgical procedure since His Bundle mapping without exposed screw provides more safety to the procedure.
In addition, the absence of delivery system allowed an alternative option during the procedure in case of difficulties to place the lead in the right ventricle and a less invasive procedure. We used a cephalic access with a 5.6-Fr lead reducing the risk of pneumothorax and crush syndrome. Of note, also a subclavian access without HBP dedicated delivery sheath would have the advantage to avoid large size sheath insertion which could potentially increase the risk of pocket hematoma. It should be also considered a cost reduction of the procedure, as the use of dedicated delivery sheath and lead would be avoided.
The distance between the superior vena cava orifice and the base of the septal cuspid of tricuspid valve, simply obtainable from an echocardiogram, may be used as a reference to shape the stylet for the lead positioning. This approach can lead to a more patient-tailored procedure when compared to the use of standard curves of specific sheaths.
This is a single case report and, therefore, our observation cannot be considered as definitive.
However, we showed the feasibility of a “simplified” approach to HBP that may be applied in further studies and provide some advantages with respect to the only commercially available system.
Acknowledgements
None.
Footnote
Conflicts of Interest: D Giacopelli is employee of BIOTRONIK Italia S.p.a.; the other authors have no conflicts of interest to declare.
References
- Deshmukh P, Casavant DA, Romanyshyn M, et al. Permanent, direct His-bundle pacing: a novel approach to cardiac pacing in patients with normal His-Purkinje activation. Circulation. 2000;101:869-77. [Crossref] [PubMed]
- Zanon F, Ellenbogen KA, Dandamudi G, et al. Permanent His-bundle pacing: a systematic literature review and meta-analysis. Europace 2018. [Epub ahead of print]. [Crossref] [PubMed]
- Vijayaraman P, Dandamudi G, Zanon F, et al. Permanent His bundle pacing: Recommendations from a Multicenter His Bundle Pacing Collaborative Working Group for standardization of definitions, implant measurements, and follow-up. Heart Rhythm 2018;15:460-8. [Crossref] [PubMed]
- Vijayaraman P, Dandamudi G. How to Perform Permanent His Bundle Pacing: Tips and Tricks. Pacing Clin Electrophysiol 2016;39:1298-304. [Crossref] [PubMed]
- Lustgarten DL. Step-wise approach to permanent His Bundle Pacing. The Journal of Innovations in Cardiac Rhythm Management 2016;7:2313-21. [Crossref]


