Current research status on the psychological situation of adults with congenital heart disease
Introduction
Congenital heart diseases (CHDs) are among the most common types of birth defects. Each year 1.35–1.5 million children are born with CHD worldwide. Due to the advances in congenital cardiology and cardiac surgery, survival rates of infants born with CHD have improved substantially (1). More than 90% of all children born with CHD reach adulthood in the industrial world, and the number of adults with CHD (ACHD) meanwhile exceeds the number of children with CHD in the long run. Unfortunately, most of the affected patients are not cured and are chronically ill due to residua, sequelae, complications from the underlying heart disease. Moreover, recent studies uncovered that many of them suffer from cardiac and non-cardiac comorbidities, and are at increased risk of psychological distress, neurocognitive deficits, and social challenges (2-4). Therefore, the need for an ongoing, lifelong holistic care for these patients is undisputed (5,6).
Given the heterogeneity of CHD, patients are faced with unique and often complex medical and psychological challenges beginning from the day they are born. These life-changing experiences entail early trauma due to numerous hospitalizations, continuous medical emergencies and developmental constraints. It has been found that this patient population tends to have an increased prevalence of mood and anxiety disorders (7,8) and a significantly higher risk of post-traumatic stress disorder (PTSD) (9). However, large-scale research on the psychological situation of ACHD and the relation to physiological health is still insufficient. Given the cross-sectional design of current research, the direction of mechanisms and the progression of psychological symptoms cannot be determined. In addition, no valid statements can be made in regards to the different types of CHD.
The purpose of this article is to raise awareness for the complex psychological situation of patients with CHD. Both medical and mental health care professionals need to provide adequate measures in order to accommodate the patients' special needs. Sensitive communication and adequate education play a vital role in reducing denial and empowering patients to make wise decisions in their healthcare. Furthermore, ongoing research should seek to identify reliable screening tools for early detection and management of mental issues in patients with CHD.
Prevalence of emotional distress [depression, anxiety, PTSD and quality of life (QOL)]
Living with CHD can be a major challenge to a person’s life as it is accompanied by a great burden in various aspects of private and professional life (10). Although most patients adjust their individual lifestyles, research shows that a significant number of ACHD experience emotional distress in terms of depression, anxiety and a compromised QOL (7). At present, knowledge of the psychological situation is relatively limited. Accordingly, the need for psychological support is high but currently only minimally covered (11).
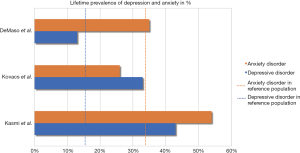
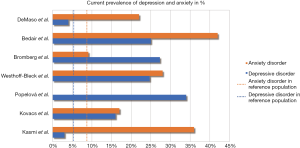
Two reviews (7,8) indicate elevated levels of depression and anxiety in ACHD. Figures 1 and 2 show the prevalence of depression and anxiety among ACHD in recent studies extracted from the reviews. Three out of seven studies present lifetime prevalence rates on depression and anxiety disorders in ACHD (11-13). In comparison to the general population (18,19), ACHD show higher rates in depression (weighted prevalence ACHD: 24% vs. global prevalence: 15%) and anxiety (weighted prevalence ACHD: 38% vs. global prevalence: 34%). Similarly, current prevalence rates of depression (weighted prevalence in ACHD: 16% vs. global prevalence: 6%) and anxiety (weighted prevalence ACHD: 29% vs. global prevalence: 8%) are elevated among ACHD compared to reference norms (18,19). The largest German study (14) using structured clinical interviews points to a significantly higher prevalence for overall psychopathology in ACHD when compared to the general population (48.0%, 95% CI: 44.7–60.0 vs. 35.7%, 95% CI: 33.5–37.9). The study included only 150 ACHD, mostly of mild or moderate severity.
In this context it is remarkable that PTSD has scarcely been investigated in ACHD although it is qualified by the exposure to a traumatic event in childhood (20). A single-center study at The Children’s Hospital of Philadelphia which enrolled 134 adult participants found that PTSD was present in 11–21% of ACHD compared to a rate of 3.5% in the general population. The researchers identified two factors that were associated with PTSD: elevated depressive symptoms and the year of most recent cardiac surgery. Accordingly, patients who had undergone cardiac surgery at an earlier stage in life were more likely to develop PTSD. Furthermore, subjects with PTSD reported lower QOL (9). Their findings support the “residual stress” theory of PTSD stating that traumatic events manifest in lasting, chronic stress (21). Their study has important clinical implications as PTSD is known to be linked to serious medical conditions in other cardiac populations (22).
Several studies (23-25) found that ACHD experience a generally good QOL. However, compromising factors entail adverse social and economic circumstances like lack of employment, older age and single life. ACHD tend to differ from healthy individuals in higher financial strain and less social support which in turn results in higher scores of emotional distress (26). A recent large-scale international study conducted by Moons et al. (27) identified functional class, higher age, unemployment status, standard of living and healthcare system characteristics as important predictors for a patient’s health status and found significant variations across the countries patients live in. Patient-reported health outcomes defined as a composite of psychological well-being, physiological functioning and health behaviors were most favorable in Switzerland, Sweden and the Netherlands and lowest in France, Japan and India. Intercou
ntry variation can be partly attributed to economic differences and healthcare system factors.
Etiology of emotional distress in ACHD
Different psychological disease models can be referred to for an explanation of emotional stress among adult CHD survivors. From a psychoanalytical perspective, the internalization of early psychological trauma due to illness and hospitalizations with the separation from parents at times leads to a higher risk for depression later in life. In fact, van Rijen et al. (28) could verify a significant relation between early hospitalizations with reoperations in CHD patients and higher behavioral and emotional problems later in life (28).
According to Bowlby’s attachment theory, a secure and trusting mother-infant relationship is essential for a child’s social-emotional development. Early mother-child separation due to hospitalizations with reoperations during infancy may disrupt the formation of a secure attachment and result in later psychological maladjustment (29).
The psycho-biological approach to depression provides evidence that repetitive stress events in early childhood lead to a neuro-transmitter imbalance in the brain. These events make individuals more vulnerable for developing maladaptive psychological responses, such as posttraumatic stress disorder or depression, later on (30).
From a behavioristic perspective depression in CHD patients can be addressed as “learned helplessness”. This view holds that because patients are permanently exposed to stressful situations linked to their illness associated with a lack of control they tend to adapt a passive (helpless) role. Learned helplessness contributes to the development of depression (8). Aggravating psychosocial factors, such as financial strain or lack of social support may contribute to the sense of helplessness (26).
Mechanisms and impact of emotional distress on health outcomes
There is sparse evidence on the impact of chronic emotional distress on health outcomes among ACHD. However, the findings on acquired heart disease suggest that high levels of emotional distress increase the risk for adverse medical outcomes and premature mortality (31-33).While depression is clearly linked to mortality in coronary artery disease patients, a meta-analysis (34) also confirmed that anxiety can be detrimental to cardiac health in patients with acquired cardiovascular disease (CVD). Based on the findings in patients with acquired CVD, it is conceivable that unrecognized and hence untreated mental issues may also put individuals with CHD at an increased risk for recurrent cardiac events. However, there is a substantial deficit of research on the interaction of psychological conditions and physiological outcomes in CHD patients. Particularly, longitudinal research on the consequences of emotional distress in CHD patients is needed.
Research among ACHD is mostly observational, identifying possible risk factors for emotional distress and diminished QOL. The research suggests that the relationship between the CHD severity and the patient’s QOL is relatively complex (23,24). Holbein et al. (35) found that individual illness perceptions are an important mediating factor in the association between the CHD diagnosis and the patients’ QOL. However, the relation of depression and anxiety symptoms to illness perceptions and QOL remains unclear and needs to be further investigated (35).
In order to understand how ACHD experience chronic illness, Oris et al. (36) went beyond illness perceptions. They examined how ACHD integrate their chronic illness into their sense of self (Illness Identity). Four different illness identity states were identified (i.e., engulfment, rejection, acceptance, and enrichment) and set in relation to psychological and physiological parameters. Oris et al. (36) found that engulfment is accompanied by maladaptive psychological and physiological outcomes in line with previous research (37). Rejection was related to more illness symptoms, but unrelated to depression and anxiety. The authors conclude that patients might reject their illness as part of their identity as a self-defense mechanism. Acceptance was linked to better psychological functioning—that is, less depression and anxiety symptoms—and less physical symptoms. Lastly, enrichment was related to more physical symptoms in ACHD as individuals experience the full scope of their illness in order to grow as a person (38). Their findings stress the importance of integrating the illness into one’s identity in order to better cope with individual disease related challenges in ACHD. Their research also implies, that providing patients with clear information on their illness (psychoeducation) and how to deal with it can improve the understanding of the illness which is beneficial to the patients’ health condition and their QOL.
Research conducted by van Rijen et al. suggests that younger patients (20 to 27 years) and female patients show more psychopathology than older patients (28 to 32 years) and male patients. In addition, the assessment of caregivers suggested more problems than the patients’ self-reports (39). It is unclear, whether rather optimistic self-reports stem from well-adjusted coping skills, or other states such as overcompensation or denial which might extend the framework of illness identity.
Treatment of emotional distress in ACHD
There is insufficient research on the treatment of mental issues in ACHD. To date, only a small amount of patients receive psychosocial or pharmacological treatment for anxiety and depression (11). According to Kovacs et al., 39% of ACHD who fulfilled diagnostic criteria for a mood or anxiety disorder have not received any psychosocial treatment (11). Preliminary results of their randomized controlled trial examining the efficacy of a cognitive-behavioral treatment in ACHD (n=42) showed reductions in depressive symptoms. Their eight-session group intervention (ACHD-CARE Program) included psychoeducation and cognitive behavioral techniques such as cognitive restructuring, relaxation, self-awareness techniques and soft skills training (40). The authors confirmed the feasibility of conducting a large-scale trial on a broad composition of ACHD to improve psychological well-being (41).
Conclusions and perspectives
Decades ago, CHD was considered a fatal pediatric condition. Due to medical and technological advances, ACHD are now becoming a fast-growing population. As research indicates, a significant number of ACHD suffer from symptoms of depression, anxiety and PTSD. These mental disorders do not only negatively impact patients’ QOL but can also put them at greater risk for cardiovascular morbidity and mortality. Explanations range from early trauma to neurological imbalances in the brain and aggravating psychosocial factors later in life. Yet, to date only a minority receives psychosocial treatment.
The influences on the psychological situation of ACHD have received little attention. An in-depth investigation of the unique role of illness identity in the psychological well-being of ACHD needs to be undertaken. It may be reasonable to consider additional psychological constructs (e.g., meaning in life, recovery-stress model) in order to gain a deeper understanding into the relation between psychological processes and physiological outcomes. Considering the tremendous heterogeneity of ACHD large-scale population-based studies are feasible to help caregivers identify crucial indicators for diagnosis and treatment.
Acknowledgements
Funding: The research work was supported by the patient organization “Herzkind e. V.”, the German Heart Foundation (“Deutsche Herzstiftung e.V.) [grant number F-30-15], and the German health care insurance AOK-Bayern.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Stout KK, Daniels CJ, Aboulhosn JA, et al. AHA/ACC guideline for the management of adults with congenital heart disease: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. J Am Coll Cardiol 2018.2018. [Epub ahead of print].
- Lui GA, Saidi A, Bhatt AB, et al. Diagnosis and management of noncardiac complications in adults with congenital heart disease: a scientific statement from the American Heart Association. Circulation 2017;136:e348-92. [Crossref] [PubMed]
- Neidenbach RC, Lummert E, Vigl M, et al. Non-cardiac comorbidities in adults with inherited and congenital heart disease: report from a single center experience of more than 800 consecutive patients. Cardiovasc Diagn Ther 2018;8:423-31. [Crossref] [PubMed]
- Singh S, Desai R, Fong HK, et al. Extra-cardiac comorbidities or complications in adults with congenital heart disease: a nationwide inpatient experience in the United States. Cardiovasc Diagn Ther 2018. [Epub ahead of print].
- van der Linde D, Konings EE, Slager MA, et al. Birth prevalence of congenital heart disease worldwide: a systematic review and meta-analysis. J Am Coll Cardiol 2011;58:2241-7. [Crossref] [PubMed]
- Neidenbach R, Niwa K, Oto O, et al. Improving medical care and prevention in adults with congenital heart disease (ACHD)—reflections on a global problem—part I: development of congenital cardiology, epidemiology, clinical aspects, heart failure, cardiac arrhythmia. Cardiovasc Diagn Ther 2018. [Epub ahead of print].
- Jackson JL, Leslie CE, Hondorp SN. Depressive and anxiety symptoms in adult congenital heart disease: Prevalence, health impact and treatment. Prog Cardiovasc Dis 2018;61:294-9. [Crossref] [PubMed]
- Pauliks LB. Depression in adults with congenital heart disease-public health challenge in a rapidly expanding new patient population. World J Cardiol 2013;5:186-95. [Crossref] [PubMed]
- Deng LX, Khan AM, Drajpuch D, et al. Prevalence and correlates of post-traumatic stress disorder in adults with congenital heart disease. Am J Cardiol 2016;117:853-7. [Crossref] [PubMed]
- Nagdyman N, Huntgeburth M, Hager A, et al. Belastungen bei Erwachsenen mit angeborenen Herzfehlern (EMAH): Sport, Beruf, Familienplanung und Schwangerschaft. Herzmedizin 2016;5:16-26.
- Kovacs AH, Saidi AS, Kuhl EA, et al. Depression and anxiety in adult congenital heart disease: predictors and prevalence. Int J Cardiol 2009;137:158-64. [Crossref] [PubMed]
- DeMaso DR, Calderon J, Taylor GA, et al. Psychiatric disorders in adolescents with single ventricle congenital heart disease. Pediatrics 2017;139. [Crossref] [PubMed]
- Kasmi L, Calderon J, Montreuil M, et al. Neurocognitive and Psychological Outcomes in Adults With Dextro-Transposition of the Great Arteries Corrected by the Arterial Switch Operation. Ann Thorac Surg 2018;105:830-6. [Crossref] [PubMed]
- Westhoff-Bleck M, Briest J, Fraccarollo D, et al. Mental disorders in adults with congenital heart disease: Unmet needs and impact on quality of life. J Affect Disord 2016;204:180-6. [Crossref] [PubMed]
- Bedair R, Babu-Narayan SV, Dimopoulos K, et al. Acceptance and psychological impact of implantable defibrillators amongst adults with congenital heart disease. Int J Cardiol 2015;181:218-24. [Crossref] [PubMed]
- Bromberg JI, Beasley PJ, D'Angelo EJ, et al. Depression and anxiety in adults with congenital heart disease: a pilot study. Heart Lung 2003;32:105-10. [Crossref] [PubMed]
- Popelová J, Slavík Z. Are cyanosed adults with congenital cardiac malformations depressed? Cardiol Young 2001;11:379-84. [Crossref] [PubMed]
- Kessler RC, Bromet EJ. The epidemiology of depression across cultures. Annual review of public health. 2013;34:119-38. [Crossref] [PubMed]
- Bandelow B, Michaelis S. Epidemiology of anxiety disorders in the 21st century. Dialogues Clin Neurosci 2015;17:327-35. [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Washington, DC, 2013.
- Boe HJ, Holgersen KH, Holen A. Reactivation of posttraumatic stress in male disaster survivors: The role of residual symptoms. J Anxiety Disord 2010;24:397-402. [Crossref] [PubMed]
- Edmondson D, Richardson S, Falzon L, et al. Posttraumatic stress disorder prevalence and risk of recurrence in acute coronary syndrome patients: a meta-analytic review. PLoS One 2012;7:e38915. [Crossref] [PubMed]
- Lane DA, Lip GY, Millane TA. Quality of life in adults with congenital heart disease. Heart 2002;88:71-5. [Crossref] [PubMed]
- Moons P, Van Deyk K, Marquet K, et al. Individual quality of life in adults with congenital heart disease: a paradigm shift. Eur Heart J 2005;26:298-307. [Crossref] [PubMed]
- Apers S, Kovacs AH, Luyckx K, et al. Quality of life of adults with congenital heart disease in 15 countries: evaluating country-specific characteristics. J Am Coll Cardiol 2016;67:2237-45. [Crossref] [PubMed]
- Eslami B, Sundin Ö, Macassa G, et al. Anxiety, depressive and somatic symptoms in adults with congenital heart disease. J Psychosom Res 2013;74:49-56. [Crossref] [PubMed]
- Moons P, Kovacs AH, Luyckx K, et al. Patient-reported outcomes in adults with congenital heart disease: Inter-country variation, standard of living and healthcare system factors. Int J Cardiol 2018;251:34-41. [Crossref] [PubMed]
- van Rijen EH, Utens EM, Roos-Hesselink JW, et al. Medical predictors for psychopathology in adults with operated congenital heart disease. Eur Heart J 2004;25:1605-13. [Crossref] [PubMed]
- Styron T, Janoff-Bulman R. Childhood attachment and abuse: Long-term effects on adult attachment, depression, and conflict resolution. Child Abuse Negl 1997;21:1015-23. [Crossref] [PubMed]
- Agid O, Kohn Y, Lerer B. Environmental stress and psychiatric illness. Biomed Pharmacother 2000;54:135-41. [Crossref] [PubMed]
- Lichtman JH, Froelicher ES, Blumenthal JA, et al. Depression as a risk factor for poor prognosis among patients with acute coronary syndrome: systematic review and recommendations: a scientific statement from the American Heart Association. Circulation 2014;129:1350-69. [Crossref] [PubMed]
- Park JH, Tahk SJ, Bae SH. Depression and anxiety as predictors of recurrent cardiac events 12 months after percutaneous coronary interventions. J Cardiovasc Nurs 2015;30:351-9. [Crossref] [PubMed]
- Watkins LL, Koch GG, Sherwood A, et al. Association of anxiety and depression with all-cause mortality in individuals with coronary heart disease. J Am Heart Assoc 2013;2:e000068. [Crossref] [PubMed]
- Celano CM, Millstein RA, Bedoya CA, et al. Association between anxiety and mortality in patients with coronary artery disease: A meta-analysis. Am Heart J 2015;170:1105-15. [Crossref] [PubMed]
- Holbein CE, Fogleman ND, Hommel K, et al. A multinational observational investigation of illness perceptions and quality of life among patients with a Fontan circulation. Congenit Heart Dis 2018;13:392-400. [Crossref] [PubMed]
- Oris L, Luyckx K, Rassart J, et al. Illness identity in adults with a chronic illness. J Clin Psychol Med Settings 2018;25:429-40. [Crossref] [PubMed]
- Van Bulck L, Goossens E, Luyckx K, et al. Illness Identity: A Novel Predictor for Healthcare Use in Adults With Congenital Heart Disease. J Am Heart Assoc 2018;7. [Crossref] [PubMed]
- Helgeson VS, Reynolds KA, Tomich PL. A meta-analytic review of benefit finding and growth. J Consult Clin Psychol 2006;74:797-816. [Crossref] [PubMed]
- van Rijen EH, Utens EM, Roos-Hesselink JW, et al. Longitudinal development of psychopathology in an adult congenital heart disease cohort. Int J Cardiol 2005;99:315-23. [Crossref] [PubMed]
- Kovacs AH, Bandyopadhyay M, Grace SL, et al. Adult Congenital Heart Disease-Coping And REsilience (ACHD-CARE): Rationale and methodology of a pilot randomized controlled trial. Contemp Clin Trials 2015;45:385-93. [Crossref] [PubMed]
- Kovacs AH, Grace SL, Kentner AC, et al. Feasibility and outcomes in a pilot randomized controlled trial of a psychosocial intervention for adults with congenital heart disease. Can J Cardiol 2018;34:766-73. [Crossref] [PubMed]