
Reclassification of coronary heart disease risk in a primary prevention setting: traditional risk factor assessment vs. coronary artery calcium scoring
Introduction
In the last 50 years, improved understanding and treatment of the atherosclerotic risk factors have resulted in significant improvements in cardiovascular (CV) mortality (CVD) (1,2). This has resulted in development of various coronary heart disease (CHD) risk prediction scores that allow recognition of individuals at risk of future events (3-8). Many of the currently recommended risk assessment tools use traditional risk factors such as the recently developed atherosclerotic cardiovascular disease (ASCVD) risk calculator which relies upon age, gender, smoking status, diabetes, hyperlipidemia and race, parameters which were identified in the seminal Framingham study (4,6). Other studies have shown that family history of premature CHD and vascular inflammation are also crucial in risk prediction of future events. As a result, other tools such as the Reynolds Risk Score (RRS) have been developed which incorporate these predictors, and have been shown to further help in reducing residual risk of future events; in both men and women (7,8). However, despite these advances and our improved ability to identify those at increased risk of CV events, a substantial group of individuals still develop CHD events despite the absence of conventional CV risk factors. For instance, in a pooled analysis of 122,458 patients from 14 international randomized controlled trials 19% men and 15% women with a CHD event lacked traditional risk factors (9).
On the other hand, based on the recent ASCVD risk calculator, it is estimated that 45 million middle-aged adults in the United States without known CVD could potentially qualify for statin therapy (4). This widening of the scope of statin therapy has spawned a significant amount of debate because of the concerns that a significant proportion of subjects would not accrue a larger absolute reduction in CVD risk, due to the fact that net treatment benefit is directly proportional to the absolute risk (4,10). Hence, it is crucial to optimize strategies that accurately assign future risk of CHD, in order to avoid over/under prescription of preventive CV therapies. Coronary artery calcium score (CACS), quantified using non-contrast cardiac computed tomography is an excellent tool to estimate the burden of coronary atherosclerosis, providing incremental utility in risk stratification of subjects without documented CHD (11,12). An elevated CACS is associated with a 10-fold higher risk of adverse CVD events, while the absence of CAC in an asymptomatic adult confers a very low risk for future CVD events (13,14). This can potentially allow us to further tailor treatment strategies, above and beyond that accorded by traditional risk stratification. Hence, in a primary prevention screening program of asymptomatic middle-aged subjects, we sought to assess the degree of risk-reclassification provided by CACS in addition to traditional risk assessment.
Methods
Study cohort
This was an observational cohort study of 1,806 consecutive, asymptomatic subjects presenting for a comprehensive evaluation in the primary prevention clinic at our tertiary care center between 3/2016 and 9/2017. Participants were self-referred, and were evaluated by primary care providers specializing in primary prevention in an outpatient ambulatory setting. This evaluation consisted of a detailed history, physical examination and an extensive laboratory evaluation. As part of the evaluation, all subjects also underwent routine CACS. All subjects were asymptomatic and free of documented CVD (including coronary artery disease, arrhythmic disease, peripheral arterial disease, cerebrovascular disease, aortic disease or valvular heart disease). The current study cohort is part of a primary prevention registry which is approved by the Institutional Review Board with waiver of individual informed consent.
Prior to CACS, each patient participated in a structured complete history taking including review of available medical records to document lack of symptoms, cardiac risk factors, past medical history, family history of premature CHD and medication use. Diabetes was defined as self-reported diabetes, or use of hypoglycemic drugs. Hypertension was defined as untreated blood pressure >140/90 mmHg, or use of antihypertensive medication. Smoking was defined as current or prior use of cigarettes. Fasting total cholesterol, high density lipoprotein, low density lipoprotein cholesterol, triglyceride and high-sensitivity C-reactive protein (CRP) levels were obtained using an enzymatic assay with an automated chemistry analyzer. Appropriate standardization of the assays was performed during the time interval of the study in compliance with quality control measures. Using this data, we calculated the ASCVD and RRS in every patient, according to previously published formulae (4,6-8).
Coronary artery calcium scoring
CACS was calculated from prospectively triggered axial non-contrast chest computed tomographic scans (Siemens Somatom Definition or Force dual source scanners, Erlangen, Germany) ranging from the base of the great vessels to the diaphragm. Agatston CACS was subsequently calculated, according to recommendations. Based on this, we also calculated the MESA-CAC risk score, according to previously published formulae (10).
Statistical analysis
Continuous variables are expressed as mean ± standard deviation and/or median with interquartile range (IQR) and compared using analysis of covariance or Mann-Whitney test, as appropriate. Categorical data is expressed as percentage and compared using chi-square. Spearman correlation coefficient was used to assess correlation between continuous variables. Statistical analysis was performed using SPSS version 11.5 (SPSS Inc., Chicago, Illinois). A P value of <0.05 was considered significant.
Results
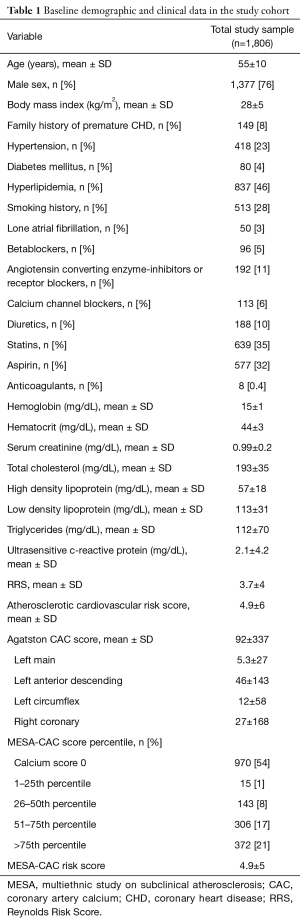
The clinical data is shown in Table 1. As would be expected from this cohort free of known cardiovascular disease, the proportion of traditional risk factors was in the low-intermediate range and medication use was relatively lower. As a result, the mean/median RRS, ASCVD and MESA-CAC scores (as a % of 10-year risk) were in the intermediate range. There was only a modest correlation between MESA-CAC score and ASCVD score (r=0.62, R2=0.40, P<0.001) and RRS (r=0.65, R2=0.43, P<0.001), respectively. We further divided the patients into different subgroups of 10-year risk (<1%, 1–4.9%, 5–9.9% and ≥10%), based on ASCVD, RRS and MESA-CAC scores. The proportions are shown in Table 2.
Full table
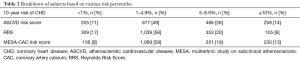
Full table
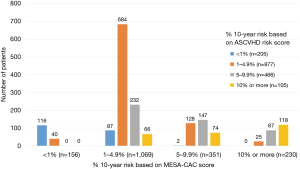
Subsequently, we studied the potential redistribution of subjects into different risk categories (ASCVD and RRS), using MESA-CAC score as the gold standard. As shown in Figure 1, 346 (19%) subjects would get a 1 ASCVD risk category downgrade (40 from 2nd to 1st category, 232 from 3rd to 2nd category and 74 from 4th to 3rd category) and 66 (4%) would get a 2 ASCVD risk category downgrade (from 4th to 2nd category), if MESA-CAC risk categorization was utilized instead of ASCVD (resulting in a total of 23% subjects within the downgraded risk category). Similarly, 302 (17%) would get a 1 ASCVD risk category upgrade (87 from 1st to 2nd category, 128 from 2nd to 3rd category and 87 from 3rd to 4th category) and 27 (1%) would get a 2 ASCVD risk category upgrade (2 from 1st to 3rd category and 25 from 2nd to 4th category), if MESA-CAC risk categorization was utilized instead of ASCVD (resulting in a total of 18% subjects with a upgrade in the risk category). As a result, 41% subjects within the current study cohort, would potentially have an upgrade or downgrade of ASCVD risk category if MESA-CAC was used instead. On the other hand, there were 431 subjects with ASCVD score ≥7.5% and LDL levels between 70–189 mg/dL, where the guidelines would recommend statin therapy (4). However, of these 105 (24%) had zero CACS.
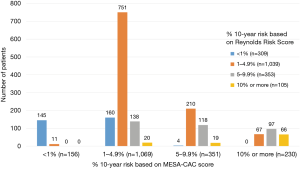
Similarly, as shown in Figure 2, 168 (9%) subjects would get a 1 RRS risk category downgrade (11 from 2nd to 1st category, 138 from 3rd to 2nd category and 19 from 4th to 3rd category) and 20 (1%) would get a 2 RRS risk category downgrade (from 4th to 2nd category), if MESA-CAC risk categorization was utilized instead of RRS (resulting in a total of 10% subjects with downgraded risk category). Similarly, 467 (26%) would get a 1 RRS risk category upgrade (16o from 1st to 2nd category, 210 from 2nd to 3rd category and 97 from 3rd to 4th category) and 71 (4%) would get a 2 RRS risk category upgrade (4 from 1st to 3rd category and 67 from 2nd to 4th category), if MESA-CAC risk categorization was utilized instead of RRS (resulting in a total of 30% subjects with upgraded risk category). In total, of the current study cohort, 40% subjects would potentially have an upgrade or downgrade of RRS risk category if MESA-CAC was used instead.
Discussion
In this large cohort of 1,806 consecutive asymptomatic subjects (majority of whom were free of traditional risk factors) undergoing a comprehensive preventive cardiovascular evaluation, we demonstrate that addition of CAC scoring to standard risk prediction scores resulted in improved stratification of future CVD risk. There was only a modest correlation between MESA-CAC score and ASCVD score as well as RRS, suggesting that addition of CAC scoring to traditional risk prediction models provided synergistic value. In the current study sample, we also demonstrate that if we utilized MESA-CAC score (which combines traditional risk stratification and CAC scoring), ~40% subjects had an upgrade or downgrade of their ASCVD risk category. The findings were similar even if RRS score was utilized instead of ASCVD score. Additionally, almost a quarter of the subjects who would have been recommended for long-term statin therapy, based on ASCVD risk score ≥7.5%, had zero CACS.
In the last 50 years, despite significant improvements in ASCVD mortality, in part due to the improved understanding and treatment of the risk factors, a significant proportion of individuals develop cardiac events despite the absence of conventional CV risk factors (9). This has given rise to the concept of residual cardiovascular risk, which is, at least in part, is believed to be due to residual inflammation. This has resulted in development of more comprehensive tools such as the RRS which identifies residual risk of future events; in both men and women (7,8). However, there is belief that direct assessment of coronary plaque burden (e.g., using CACS) would provide further incremental benefit in asymptomatic individuals in terms of future risk stratification. CACS measurement has been previously demonstrated to be a significantly better prognosticator of future coronary events as compared to traditional risk factor assessment, CRP or indirect measures like ankle brachial index or carotid intima thickness (13,15). Indeed, as demonstrated in the current study, because there is only a modest association between standard risk factor assessment (including risk scores that incorporate inflammation, like RRS) and CAC, it would make intuitive sense that using these prognosticators in combination would provide synergistic as opposed to competing information.
To put it in context for the practicing cardiologist, addition of MESA-CAC score can help in different ways in patients with either high or low RRS/ASCVD scores. For instance, if there is a high-risk asymptomatic RRS/ASCVD patient with a zero MESA-CAC score, we can downgrade the risk of a longer-term event. This might come into account in patients who have statin intolerance or are unwilling to take longer-term therapies. On the other side, if there is a patient with a low risk ASCVD/RRS score (especially someone who would not meet criteria for statin therapy) and a very elevated MESA-CACS score, then we could potentially identify an individual who would benefit from longer-term primary prevention therapy, including statins. Also, as described in previous reports, incorporating CACS into risk stratification algorithms could potentially reduce the number of subjects who would be recommended long-term statin therapy on the basis of higher traditional risk, but could get by without statin therapy in the setting of a zero CACS.
There are a number of important limitations that must be consider in the current study. This is an observational study from a large tertiary care center with its inherent biases. Whether our results may be generalized to other populations will require further study. The current study did not test outcomes or causality, but focused on reclassification of potential risk. We have to acknowledge the potential for an increase in downstream costs related to unnecessary testing and harm from unnecessary invasive procedures that could be associated with such primary prevention programs. However, the results could help guide physicians to manage higher-risk individuals with aggressive primary prevention strategies, including medial therapy, exercise prescription, weight loss and risk factor/stress control. On the other hand, improved risk classification could also reduce excess long-term statin use in patients who have no documented CACS.
Conclusions
In a primary prevention screening program of asymptomatic middle-aged subjects, RRS overestimates and ASCVHD underestimates 10-year CHD risk vs. MESA-CAC score. Addition of CAC scoring results in significant risk reclassification. Incorporation of CACS information could also further streamline utilization of long-term statin therapy.
Acknowledgments
None.
Footnote
Conflicts of Interest: Dr. Desai is supported by the Haslam Family endowed chair in cardiovascular medicine and Khouri Family philanthropic gift to study prediction of premature coronary artery disease. The other authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Institutional Review Board (IRB number: 16-967) with waiver of individual informed consent.
References
- Nabel EG, Braunwald E. A tale of coronary artery disease and myocardial infarction. N Engl J Med 2012;366:54-63. [Crossref] [PubMed]
- Benjamin EJ, Virani SS, Callaway CW, et al. Heart Disease and Stroke Statistics-2018 Update: A Report From the American Heart Association. Circulation 2018;137:e67-492. [Crossref] [PubMed]
- Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA 2001;285:2486-97. [Crossref] [PubMed]
- Stone NJ, Robinson JG, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2014;63:2889-934. [Crossref] [PubMed]
- Perk J, De Backer G, Gohlke H, et al. European Guidelines on cardiovascular disease prevention in clinical practice (version 2012). The Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts). Eur Heart J 2012;33:1635-701. [Crossref] [PubMed]
- Goff DC Jr, Lloyd-Jones DM, Bennett G, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2014;63:2935-59. [Crossref] [PubMed]
- Ridker PM, Paynter NP, Rifai N, et al. C-reactive protein and parental history improve global cardiovascular risk prediction: the Reynolds Risk Score for men. Circulation 2008;118:2243-51. [Crossref] [PubMed]
- Ridker PM, Buring JE, Rifai N, et al. Development and validation of improved algorithms for the assessment of global cardiovascular risk in women: the Reynolds Risk Score. JAMA 2007;297:611-9. [Crossref] [PubMed]
- Khot UN, Khot MB, Bajzer CT, et al. Prevalence of conventional risk factors in patients with coronary heart disease. JAMA 2003;290:898-904. [Crossref] [PubMed]
- Nasir K, Bittencourt MS, Blaha MJ, et al. Implications of Coronary Artery Calcium Testing Among Statin Candidates According to American College of Cardiology/American Heart Association Cholesterol Management Guidelines: MESA (Multi-Ethnic Study of Atherosclerosis). J Am Coll Cardiol 2015;66:1657-68. [Crossref] [PubMed]
- Detrano R, Guerci AD, Carr JJ, et al. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med 2008;358:1336-45. [Crossref] [PubMed]
- Erbel R, Mohlenkamp S, Moebus S, et al. Coronary risk stratification, discrimination, and reclassification improvement based on quantification of subclinical coronary atherosclerosis: the Heinz Nixdorf Recall study. J Am Coll Cardiol 2010;56:1397-406. [Crossref] [PubMed]
- Blaha MJ, Budoff MJ, DeFilippis AP, et al. Associations between C-reactive protein, coronary artery calcium, and cardiovascular events: implications for the JUPITER population from MESA, a population-based cohort study. Lancet 2011;378:684-92. [Crossref] [PubMed]
- Sarwar A, Shaw LJ, Shapiro MD, et al. Diagnostic and prognostic value of absence of coronary artery calcification. JACC Cardiovasc Imaging 2009;2:675-88. [Crossref] [PubMed]
- Yeboah J, McClelland RL, Polonsky TS, et al. Comparison of novel risk markers for improvement in cardiovascular risk assessment in intermediate-risk individuals. JAMA 2012;308:788-95. [Crossref] [PubMed]


