
Impact of paroxysmal versus non-paroxysmal atrial fibrillation on outcomes in patients undergoing transcatheter mitral valve repair
Introduction
Transcatheter mitral valve repair (TMVR) has emerged as a promising treatment option for symptomatic patients with chronic severe primary mitral regurgitation for patients at higher surgical risk (1,2). The MitraClip® device system is now approved for repair of both degenerative and functional MR in US and has been proven to be effective in reducing MR, symptoms of heart failure, and left ventricular remodeling (3,4).
Atrial fibrillation (AF) significantly increases the risk of cardioembolic events and heart failure (5). It has been categorized as paroxysmal (returns to sinus rhythm within 7 days), non-paroxysmal (returns to sinus rhythm after 7 days), or permanent (does not return to sinus rhythm) (6). Almost half of the patients with degenerative MR have AF at 10 years (7). Patients with degenerative MR and AF had higher risks of stroke, bleeding, death and HF hospitalizations, after TMVR. Previous studies have shown that non-paroxysmal AF is associated with higher rate of stroke and mortality when compared to paroxysmal AF (8). Whether any difference exists in the impact of paroxysmal versus non-paroxysmal AF on post-TMVR outcomes remains a subject of interest. Our goal is to explore this impact based on 2016 Nationwide Readmission Database (NRD) for patients undergoing transcatheter MV repair.
Methods
Study population
Patients were selected from Nationwide Readmission Database (NRD) for year 2016. Patients 18 years and older in age who underwent TMVR procedure and had a concurrent ICD-10 diagnosis of either paroxysmal (I48.0) or non-paroxysmal AF (I48.1 and I48.2) were included. Diagnoses and procedures were found using ICD-10 codes. Patients were categorized into non-paroxysmal and paroxysmal AF groups.
To ensure complete 30-day follow-up for a calendar year, discharges were limited to January-November. Discharges in December were excluded. Further exclusion criteria included patients with ICD-10 procedure codes. For the readmission outcome, patients were excluded if index admission had missing length of stay (LOS) or the patient died or left the hospital against medical advice.
Variable of interest
Outcomes of interest were in-hospital stroke, mortality, 30-day readmission, categorized as no admission, cardiac or non-cardiac admission, LOS, discharge disposition and a composite endpoint of mortality, readmission, or stroke during index hospitalization. The main predictor of interest was type of AF (paroxysmal versus non-paroxysmal). Covariates of interest were age, gender, income quartile, number of Elixhauser comorbidities, hospital size, and teaching status of hospital.
Statistical analysis
Statistical Analysis System (SAS) software 9.4 (TS1M5, SAS Institute Inc., Cary, North Carolina) was used for statistical analysis. Baseline characteristics were determined using SAS procedures designed to account for the complex sampling design of the NRD survey. Statistical analysis was appropriately weighted using the weights supplied by the NRD to produce nationally representative estimates. All analyses are performed on the weighted number of events in the cohort using complex survey procedures and domain analysis to ensure proper adjustment of standard errors. PROC SURVEYFREEQ, PROC SURVEYMEANS, and PROC SURVEYREG were used to determined baseline characteristics. Differences in baseline characteristics are evaluated using F-test results from a simple linear regression in PROC SURVEYREG for continuous variables (PROC SURVEYMEANS does not give P value of comparison groups, simple linear regression is an established workaround for this) and Rao Scott Chi-Square results from PROC SURVEYFREQ for categorical variables. Categorical variables are displayed as percent weighted visits with 95% confidence of these estimates. Continuous variables are displayed as median (interquartile range).
The association between type of AF and the binary outcomes (mortality, stroke, composite outcome) were analyzed using multivariable logistic regression using PROC SURVEYLOGISTIC. The association between type of AF and the multinomial (more than two levels) outcomes (readmission and discharge disposition) were analyzed using multivariable generalized logistic regression using PROC SURVEYLOGISTIC (logit). The association between type of AF and the continuous LOS outcome was analyzed using multivariable linear regression with PROC SURVEYREG. All models were adjusted for age, gender, number of Elixhauser comorbidities, income quartile, hospital size, and teaching status of hospital. Results are presented as odds ratios (95% confidence interval) for categorical outcomes (logistic models) and beta estimates for continuous outcomes (linear regression).
This study has been rendered exempt from ethics review.
Results
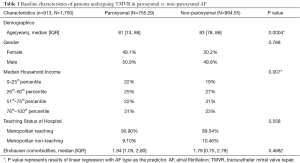
A total of 913 (weighted N=1,750) patients from Nationwide Readmission Database for 2016 who underwent TMVR in the US were selected. Of these, 510 (weighted N=994.55) or 57% patients had non-paroxysmal AF and 403 (weighted N=755.29) or 43% had paroxysmal AF (Table 1). Patients with non-paroxysmal AF were older (82.53 vs. 81.27, P=0.0004) when compared to paroxysmal AF. The median household income differed between the paroxysmal and non-paroxysmal AF groups (P=0.007). Otherwise, the groups were largely similar (Table 1). The Elixhauser comorbidity score was similar between the paroxysmal and non-paroxysmal AF groups as well.
Full table
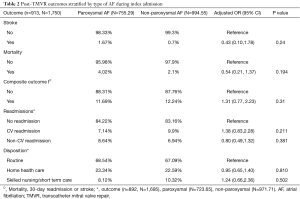
After adjustment, there was no statistical difference in the odds of stroke (OR 0.43; 95% CI: 0.10–1.78), mortality (OR 0.54; 95% CI: 0.21–1.37), composite outcome of stroke, readmission, and mortality (OR 1.31; 95% CI: 0.77–2.23), or median LOS (estimated beta −1.11, SE 0.675, P=0.101) between non-paroxysmal vs. paroxysmal AF (Table 2, Figure 1). A total of 892 (weighted N=1,695) patients were eligible for inclusion for discharge disposition and 30-day readmission analysis, of these 57% (weighted N=971.71) had non-paroxysmal AF and 43% (weighted N=723.65) had paroxysmal AF (Table 2). After adjustment, there was no statistical difference in the odds of cardiac readmission (OR 1.38; 95% CI: 0.83–2.28), non-cardiac readmission (OR 0.80; 95% CI: 0.49–1.32) and discharge to skilled nursing/short term care (OR 1.24; 95% CI: 0.66–2.36) between non-paroxysmal vs. paroxysmal AF patients (Table 2).
Full table

Discussion
In this analysis from the 2016 Nationwide Readmission Database (NRD) investigating patients undergoing TMVR, we did not find significant differences in outcomes (death, stroke, discharge disposition or 30-day readmissions) between those with either paroxysmal or non-paroxysmal AF. Baseline characteristics between the two groups were largely similar except for the age; Non-paroxysmal AF patients were older when compared to paroxysmal AF.
The onset of AF in patients with chronic severe primary MR with normal left ventricular function is a class II indication of surgical MV repair (1). The association of AF with poor outcomes in those undergoing mitral valve repair, by surgical or transcatheter route has been shown before. The association of AF with worse survival in the patients with surgical MV repair has been previously reported (9,10). In a recent analysis from the TVT registry, AF was associated with a longer LOS, and worse outcomes at one year with respect to a composite outcome of death or HF hospitalization, stroke and bleeding (11).
Although studies have investigated the impact of AF on TMVR outcomes, data investigating the impact of type of AF on outcomes after TMVR remains sparse. In the analysis from the TVT registry, those with non-paroxysmal AF were associated with a higher 30-day mortality or HF hospitalization than paroxysmal AF (10) but these differences were attenuated at 1-year. In this study from NRD, we did not find any meaningful differences in outcomes by type of AF. Surprisingly, those with paroxysmal AF had twice the stroke rate as compared with those with non-paroxysmal AF. It is possible that those who had paroxysmal AF were less likely to be on long-term anticoagulation. Unfortunately, we were limited by unavailability of medication data to further investigate this potential association.
Our study has several limitations. First, we did not have information on echocardiographic characteristics of patients. A previous study found that the combined residual MR and elevated MV pressure gradients after TMVR was associated with poor prognosis independent of presence of AF (11). Secondly, we did not have access to the anticoagulation status of the patients. Cardiac death in mitral valve repair patients was found to be predominantly due to cardioembolic events in AF patients in a previous study (12). The baseline characteristics that confer a high surgical risk and qualify patient for TMVR, for example by STS score, would also confer a high CHADSVASC score (stroke risk), and a high HAS-BLED score (bleeding risk), which could make anticoagulation decisions similarly difficult in these patients regardless of type of AF; and we could not adjust for the anticoagulation status. Finally, coding errors in NRD could affect the classification of patients into the different types of AF.
Conclusions
In-hospital and readmission outcomes did not differ among patients by type of AF following transcatheter mitral valve repair. Further studies are needed to confirm these findings, especially with respect to anticoagulation status, echocardiographic findings, and baseline characteristics. More research is needed to better understand the prognostic impact of atrial fibrillation on long term outcomes after TMVR.
Acknowledgments
None.
Footnote
Conflicts of Interest: Dr. Arora’s spouse has proprietary role in research EZ LLC.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study has been rendered exempt from ethics review.
References
- Nishimura RA, Otto CM, Bonow RO, et al. 2017 AHA/ACC Focused Update of the 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2017;70:252-89. [Crossref] [PubMed]
- Feldman T, Foster E, Glower DD, et al. Percutaneous repair or surgery for mitral regurgitation. N Engl J Med 2011;364:1395-406. [Crossref] [PubMed]
- Sorajja P, Vemulapalli S, Feldman T, et al. Outcomes With Transcatheter Mitral Valve Repair in the United States: An STS/ACC TVT Registry Report. J Am Coll Cardiol 2017;70:2315-27. [Crossref] [PubMed]
- Lim DS, Reynolds MR, Feldman T, et al. Improved functional status and quality of life in prohibitive surgical risk patients with degenerative mitral regurgitation after transcatheter mitral valve repair. J Am Coll Cardiol 2014;64:182-92. [Crossref] [PubMed]
- Pellman J, Sheikh F. Atrial fibrillation: mechanisms, therapeutics, and future directions. Compr Physiol 2015;5:649-65. [Crossref] [PubMed]
- Camm AJ, Al-Khatib SM, Calkins H, et al. A proposal for new clinical concepts in the management of atrial fibrillation. Am Heart J 2012;164:292-302.e1. [Crossref] [PubMed]
- Grigioni F, Avierinos JF, Ling LH, et al. Atrial fibrillation complicating the course of degenerative mitral regurgitation: determinants and long-term outcome. J Am Coll Cardiol 2002;40:84-92. [Crossref] [PubMed]
- Link MS, Giugliano RP, Ruff CT, et al. Stroke and Mortality Risk in Patients With Various Patterns of Atrial Fibrillation: Results From the ENGAGE AF-TIMI 48 Trial (Effective Anticoagulation With Factor Xa Next Generation in Atrial Fibrillation-Thrombolysis in Myocardial Infarction 48). Circ Arrhythm Electrophysiol 2017;10. [Crossref] [PubMed]
- Alexiou C, Doukas G, Oc M, et al. The effect of preoperative atrial fibrillation on survival following mitral valve repair for degenerative mitral regurgitation. Eur J Cardiothorac Surg 2007;31:586-91. [Crossref] [PubMed]
- Arora S, Vemulapalli S, Stebbins A, et al. The Prevalence and Impact of Atrial Fibrillation on 1-Year Outcomes in Patients Undergoing Transcatheter Mitral Valve Repair: Results From the Society of Thoracic Surgeons/American College of Cardiology Transcatheter Valve Therapy Registry. JACC Cardiovasc Interv 2019;12:569-78. [Crossref] [PubMed]
- Spieker M, Hellhammer K, Spiesshofer J, et al. Effect of Atrial Fibrillation and Mitral Valve Gradients on Response to Percutaneous Mitral Valve Repair With the MitraClip System. Am J Cardiol 2018;122:1371-8. [Crossref] [PubMed]
- Eguchi K, Ohtaki E, Matsumura T, et al. Pre-operative atrial fibrillation as the key determinant of outcome of mitral valve repair for degenerative mitral regurgitation. Eur Heart J 2005;26:1866-72. [Crossref] [PubMed]


