Profile of cardiac disease in Cameroon and impact on health care services
Introduction
Cameroon, a country in Central Africa is also called “Africa in Miniature”, because almost 90% of the African ecosystems are represented. It is situated in the Golf of Guinea, extending from the Atlantic Ocean in the south to Lake Chad in the north. The Country is rich in natural, agricultural, forestry, water and mining resources (1).
The population of Cameroon is estimated at 19,294,149 inhabitants (CIA fact book, 2010) with the majority of the population (70%) employed in the agriculture sector. The population is made up of various ethnic groups. The largest group is the Cameroon highlanders who comprise 31% of the population. Other major groups are the Equatorial Bantu (19%), Kirdi (11%), Fulani (10%) and the Northwestern Bantu (9%). The largest urban agglomeration and capital city is Yaoundé. The official languages are French and English, but local languages are highly prevalent. The life expectancy at birth for males and females is 53.2 and 54.9 years, respectively (2).
Health care system and health workforce
The epidemiologic profile of Cameroon is dominated by transmissible diseases, subsequently, leading causes of death in Cameroon includes: HIV/AIDS, lower respiratory infections, malaria, diarrheal diseases, perinatal conditions. However, the prevalence of non-communicable disease and in particular cardiovascular diseases (CVD) is increasing (3).
The Cameroonian national health system consists of various public and private entities, institutions, and organizations that provide health services, under the regulation of the Ministry of Public Health. The system is pyramidal with three levels: central (strategic), intermediary (technical) and peripheral (operational). The country has 178 health districts, with 162 districts hospitals among which only 154 are operational. Additionally, Cameroon has 2,043 public medical structures, mainly concentrated in urban zones (4). Cameroon as most developing countries has extensively used public resources to support health system. However, because of the recessions in the 1980s and early 1990s, there was a decline in the resources available for financing publicly provided services, including health. This is reflected in the health workforce.
There are only 1,555 physicians in Cameroon, representing 0.8 physicians per 10,000 inhabitants. In other words, there is only one doctor for 12,500 people. This ratio is one of the lowest in the world. Cameroon is presently facing a growing crisis in the medical field due to an acute shortage of qualified personnel, especially medical doctors (5). The causes for the shortages of health workers are multi-factorial including brain drain to the private sector and other countries, low salaries, poor working conditions and insufficient training capacities.
Health insurance practically does not exist in Cameroon. Generally, family members cover for the cost of treatments. This often puts significant financial burden on the family members not infrequently resulting in the accumulation of huge debts and financial difficulties. Paying for health care often competes with financial commitments for education for children, shortage of food, and potentially a loss of home. The Government has recently attempted to put in place a healthcare plan for its civil servants, which would cover a fraction of the healthcare costs incurred by civil servants who fell ill.
Since 2001, a number of health policies relevant to chronic diseases management, as well as those addressing standards and norms for a primary health care and community care have been formulated and adopted by the Cameroonian Ministry of Public Health. The baseline Cameroon Burden of Diabetes (CAMBoD) survey provided new scientific knowledge that guided health policy and the implementation of a diabetes and hypertension program. Diabetes and hypertension were recognized as emerging public-health problems, and incorporated into a national 10-year plan for health promotion. This lead to the creation of two bodies within the Ministry of Public Health: the Department of Applied Research; and the Department of Disease Control that focuses on non-communicable diseases (6).
Africa increasingly bears a significant proportion of the global burden of chronic diseases, along with poor countries of Asia and Latin America. The World Health Organization projects that over the next ten years the continent will experience the largest increase in death rates from CVD, cancer, respiratory disease and diabetes (7). The relative and absolute importance of CVD in children and adults in countries of sub-Saharan Africa is assumed to be increasing in urban areas, but information on prevalence in rural area is scant (8,9). This paper is to investigate the readiness of services for care of patients presenting with CVD, also the profile and the management of these diseases in St. Elizabeth catholic general hospital Shisong, cardiac centre.
Material and methods
Patients and screening
The study was approved by the Ethics Committee of St. Elizabeth Catholic General Hospital. Between November 2009 and November 2011, a population of 8,389 adults and 706 children consulted the referral cardiac centre of St. Elizabeth Catholic General Hospital. The patient’s age was between 5 days and 103 years, with a mean of 48.7±18 years old. Female represents 54.2% of the total population. Blood pressure was recorded on the right arm in a seated subject after 10-minute rest, using an automated blood pressure device (OMRON® M4) and appropriate cuff sizes. The average of two measurements taken at two minutes interval was recorded. Hypertension was defined as systolic blood pressure ≥140 mmHg or diastolic blood pressure ≥90 mmHg, or use of antihypertensive drugs irrespective of the blood pressure. Congestive heart failure was defined according to the modified Framingham criteria for the diagnosis of heart failure (10). The following criteria for heart failure were used. Major criteria: paroxysmal nocturnal dyspnoea raised jugular venous pressure, clinical cardiomegaly, basal crepitations, S3 gallop, clinical acute pulmonary oedema, pulmonary upper lobe blood diversion on chest X-ray (or pulmonary oedema on chest X-ray). Minor criteria: tachycardia, orthopnoea, exertional dyspnoea, nocturnal cough, hepatomegaly, pleural effusion, diuretic use. Heart failure was diagnosed if the patient had two major and one minor or one major and two minor criteria. Severity of heart failure on admission was assessed using the New York Heart association (NYHA) functional classification. Arrhythmia was diagnosed based on symptoms and confirmed by the electrocardiogram. Also, detailed history including patients’ socio-demographic characteristics, past medical history, and drug history were obtained through a standard questionnaire.
Diagnostic investigations
A complete clinical assessment and 12 lead electrocardiograms (ECG) were performed. Complementary investigations used to confirm and establish the aetiology of the disease included chest X-ray, electrocardiography, and bi-dimensional Doppler echocardiography then, a comprehensive transthoracic Doppler-echocardiogram (TTE) according to the recommendations of the American Society of cardiology were performed using commercially available echocardiography equipment (Acuson Sequoia, Acuson Co, Mountain View, USA) with a 4-7 Megahertz transducer. The TTE indices analyzed included the left ventricle end systolic diameter (LVESD), the left ventricle end diastolic diameter (LVEDD) using the parasternal long axis position in M mode, and the ejection fraction (EF). Post rheumatic valvulopathy was defined by the presence of any definite evidence of mitral or aortic valve regurgitation seen in two planes by the TTE, accompanied by at least two of the following three morphologic abnormalities of the regurgitating valve: restricted leaflet mobility, focal or generalised valvular thickening, and abnormal subvalvular thickening (11).
Data analysis
Values are expressed as mean ± the standard deviation (SD) and statistical analysis were performed using the Student’s t-test. The SPSS 11 statistical analysis software was used for all analysis. The chi squared test was used to test for association between categorical variables. The student t-test was used to compare means of two variables, whilst the ANOVA was used to compare more than two variables. The level of significance was set at P<0.05, and a 95% confidence interval was applied to the numerical variables which are normally distributed.
Results
Clinical diagnosis (Figure 1)
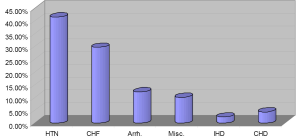
Hypertension
Hypertension was diagnosed in 41.5% of patients. Isolated systolic hypertension was rarely found. According to the JNC7 classification, 45.2% patients were in class II. Hypertension was associated with diabetes in 11% cases. Patients with hypertensive encephalopathy represented 5.2% of the population. Complications of hypertension included neurological complications in 8.2% (cardiovascular accident with limbs paralysis or paresis), renal impairment in 2.3%, and hypertensive retinopathy in 1.1%.
Congestive heart failure
CHF was diagnosed in 29.6% of patients. CHF was predominantly due to left ventricular systolic dysfunction (87.2%), compared a significantly percentage of diastolic dysfunction (12.8%), (P<0.05). Forty-four percent of patients were in class III of the NYHA and 7% in class IV. Dyspnoea was highly prevalent (95.2%) and frequently associated to paroxysmal nocturnal dyspnoea (68.1%). Lower limbs oedema and hepatomegaly were frequent physical findings (41.9%).
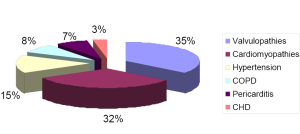
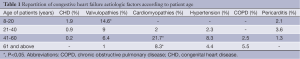
In the entire population etiology of CHF (Figure 2) were predominantly valvulopathies (35%) and cardiomyopathies (32%). Other causes included hypertension (15%), pericarditis (7%), chronic obstructive pulmonary disease (8%) and congenital heart diseases (3%). In elderly (>60 years old) with cardiomyopathies, hypertension and chronic obstructive pulmonary disease were more frequently diagnosed (Table 1).
Full table
Arrhythmia
Cardiac arrhythmias were seen in 12.2% of patients, and included atrial fibrillation in 35.2%, followed by ventricular ectopic beats in 20.3%, atrial flutter, and atrial ectopic beats. Atrioventricular block I, II and III degree were identified in 40.5%, 38.1% and 21.4%., respectively
Ischemic heart disease
Patients with ischemic heart disease represented 0.02‰ of the population (n=17).
Miscellaneous
Other pathologies including acute pulmonary artery embolism, lower limbs venous insufficiency, thrombophlebitis, were diagnosed in 10%
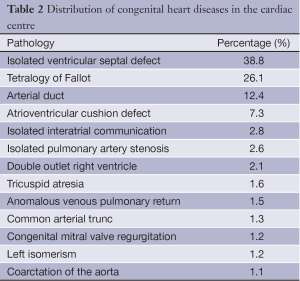
Congenital heart disease
In children, congenital heart diseases were identified in 4.3% as shown in Table 2. The most diagnosed pathology was isolated ventricular septal defect, then tetralogy of Fallot.
Full table
Results of diagnostic studies
Trans-thoracic Doppler echocardiography
Patients with dilated cardiomyopathy showed diffuse dilatation of the cardiac chambers and in particular of the left ventricle (mean LVEDD: 68.2±2.5 mm). Left ventricular function was significantly reduced (EF 32%±6%). Functional mitral valve regurgitation related to mitral valve annulus dilatation was frequently seen
In subjects with chronic obstructive disease of the lungs, the right atrium and ventricle were significantly dilated with associated moderate to severe tricuspid regurgitation and systolic pulmonary artery hypertension (mean estimated systolic pulmonary pressure 84.4±14 mmHg, ranging between 70 and 114 mmHg).
Patients with post rheumatic valvulopathies showed fibrotic destruction of the mitral valve and aortic valves, calcified leaflets, abnormal subvalvular thickening rigid opening with coaptation default in patients with regurgitation and poor opening in patients with stenosis. Complications of rheumatic heart disease included secondary pulmonary hypertension in 11.8%, and functional tricuspid regurgitation was seen in 21.9% of patients.
In patients with hypertension, we observed a concentric hypertrophy of the left ventricle with conserved systolic function but poor diastolic function.
Management of the diseases
Patients with severe hypertension, CHF, symptomatic arrhythmias were admitted for further investigations and initial care. The mean hospital stay for our patients was 13±7 days (the range was 7 to 21 days). In the newly open cardiac centre Shisong, 110 patients benefited from a mechanical valve replacement, valvuloplasty was performed in eight cases, and congenital heart diseases were corrected in 105 cases. Eight open arterial ducts were closed with a device and two stents were implanted in patients with myocardial infarction. Fifteen pace makers (ten dual chamber and five single chamber systems) were implanted. The costs of procedures were covered totally by patients. On the surgical waiting list are still more than 150 cases. Pericardial tap in patients with tamponade was done with success in 78% cases. Five percent of patients presented after failed consultation with traditional healers. These subjects came frequently with skin infections after scarifications, refractory lower limbs edemas, prolonging their stay in the hospital. Sometimes, because of the patient’s poverty, the cardiologist is obliged to prioritize among medications, and choose a single of few medications.
Discussion
Health care in Cameroon is characterized by a high mortality due to infectious diseases, poor organization of the health system characterized by absence of health insurance, and lack of health care professionals.
Non-communicable disease and specifically cardiovascular disease is of increasing importance in sub-saharan Africa. Studies conducted in Cameroon in 1994 and 1998 showed increases in obesity, hypertension and hyperglycemia (12,13). In 1994 the prevalence rates of hypertension and diabetes in the adult population were 8.3% and 1.1%, respectively. In 1998 these rates increased to 17.6% (hypertension) and 6.2% (diabetes) for urban men (7). In our centre, located in a rural area, hypertension was the most diagnosed non communicable disease in 2010, having a prevalence of 46.5%. Rapid urbanization and transition from agrarian life to the wage-earning economy of city life continue to fuel increases in average blood pressure levels and prevalence of hypertension. Although the true burden of high blood pressure in sub-Saharan Africa remains largely unmeasured, compelling preliminary evidence suggests that it is the foundation for epidemic cardiovascular disease in Africa and already contributes substantively to death and disability from stroke, heart failure, and kidney failure in this region (14). There is clear evidence that Africa is undergoing an epidemiological transition to CVD, with a central role of hypertension (15).
Post rheumatic valvulopathies and congenital heart diseases are the predominant aetiological factors of CHF in young patients. Our data confirms the fact that RHD still accounts for a major proportion of all CVD in children and young adults in African countries (16). Although many cases of rheumatic valvular abnormalities in children may resolve spontaneously, many will develop to clinically manifest disease in young adulthood. In our experience, the causes of heart failure in sub-saharan African remain largely nonischemic and predominantly caused by valvulopathies. Our data are quite different from those reported by Mayosi BM in South Africa and by Onwuchekwa C and Asekomeh GE in urban Nigeria. Those authors reported an high incidence of hypertension as the dominant cause of heart failure (17,18). Also, coronary angiography was not available in our hospital during the time of the study. We believe that more cases of ischemic dilated cardiomyopathy could have been diagnosed by using an invasive approach.
Despite the increasing role of non-communicable cardiovascular disease, it is important to discuss the impact of HIV, tuberculosis and wood burning on heart disease in our milieu. These data are confirmed by the studies of Magulaa NP, Mayosi BM (19,20) demonstrating that cardiac involvements in human immunodeficiency virus (HIV) infection, with cor pulmonale, and pericarditis contribute to over 20% of cases of heart failure. In our study, performed in a rural area, we have shown cor pulmonale as an aetiologic factor of heart failure due to indoor pollution. Approximately half the world’s population and up to 90% of rural households in developing countries still rely on unprocessed biomass fuels in the form of wood, dung and crop residues. This is associated with high levels of indoor air pollution, to which women, especially those responsible for cooking, and their young children, are most heavily exposed. In Cameroon unprocessed biomass fuels are also used in houses for heating purposes (21,22).
Similar to the studies by Bannerman [1998] and el Hag [1994] (23,24), we found that the most frequent congenital pathologies were isolated ventricular septal defect and tetralogy of Fallot. Ejim et al. [2009], also showed that isolated ventricular septal defect was the most prevalent pathology diagnosed in 70% of all the cases of congenital heart diseases studied (25). Cushion defects were mostly diagnosed in patients with trisomy 21. Because of high cost, the majority of patients cannot afford treatment. Limited access to health care is associated with late presentations to practitioners. In a previous study late presentation to practitioners was observed in 79.3% of patients (25). Both limited access to health care and the high costs of treatments also explain the very high incidence of late presentations (68.2%) recorded in Bannerman’s study [1998] in Zimbabwe (23). We diagnosed a perimembranous ventricular septal defect and a tetralogy of Fallot in a 13- and 16-year-old boy and girl, respectively. Adults with congenital heart diseases were found in 1.5% of cases. Heart failure has emerged as an important form of cardiovascular disease in Africa. It has great social and economic relevance owing to its high prevalence, mortality and impact on young, economically active individuals. Concerning treatment three major trends emerge from few studies that have addressed the issue of management of heart failure: first of all underutilization of medications with proven efficacy such as angiotensin-converting enzyme inhibitors (ACEI) and beta blockers because of poverty. For example, in a study from Nigeria, only 65% of heart failure patients were on ACEI (26,27). In another study from Cameroon, only 19% of patients with heart failure were on beta blockers. Second, when medications are appropriately prescribed, this is not always followed by patient compliance (28). Finally, traditional treatments often delay diagnosis and proper therapy. It’s important to mention that except for hypertension, and ischemic heart disease, other common cardiovascular pathology is often related to infectious disease. For example, rheumatic heart disease, and dilated cardiomyopathy are frequently complication of B haemolytic streptococcal infection and myocarditis respectively (29). Congenital heart disease can be related to maternal infection during pregnancy. It is clear that Cameroon is at the transition from the stage of receding pandemics into the stage of non-communicable diseases. Recent improvement in our centre with the construction of a fully equipped operating theatre and a cardiac catheterization laboratory with capabilities for electrophysiology and percutaneous treatment of heart diseases will increase treatment possibilities for heart diseases in our country (30), but access to such facilities remains challenging
Conclusions
- There is a high prevalence of hypertension in Cameroon which highlights the urgent need to implement a new national program targeting risk factors and community awareness;
- There is an increased incidence of hypertension;
- Congestive heart failure mainly due to post rheumatic valvulopathies is common amongst the young in our centre;
- Isolated ventricular septal defect the pathology the most encountered in children;
- We are proud of the accomplishments of the Shisong cardiac centre in fighting against cardiovascular mortality, with a high number of cardiovascular surgicalinterventions in Cameroon.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Poverty Reduction Strategy Paper (PRSP) for Cameroon. Progress Report PRSP, IMF International Monetary Fund. IMF Country Report No. 08/1, 2009.
- CIA factbook. Retrieved, June 21st, 2010. Available online: https://www.cia.gov/library/publications/the-world-factbook/geos/cm.html, 2010.
- The World Health Report 2006: Working Together For Health. Geneva: World Health Organization; Available online: http://www.who.int/whr/2006, accessed 10 June 2010.
- Ministère de la Santé Publique du Cameroun. Stratégie sectorielle de santé. unpublished, 2010.
- Abena Obama MT, Nko’o Amvene S, Afane Ze E, et al. La migration du personnel de la santé qualifié dans la region Afrique: Le cas du Cameroun. Health Science & Disease 2003;4:22-7.
- Echouffo-Tcheugui JB, Kengne AP. Chronic non-communicable diseases in Cameroon - burden, determinants and current policies. Global Health 2011;7:44. [PubMed]
- de-Graft Aikins A, Unwin N, Agyemang C, et al. Tackling Africa’s chronic disease burden: from the local to the global. Global Health 2010;6:5. [PubMed]
- Razum O. Monitoring cardiovascular disease in Zimbabwe: a review of needs and options. Cent Afr J Med 1996;42:120-4. [PubMed]
- Kengne AP, Awah PK, Fezeu L, et al. The burden of high blood pressure and related risk factors in urban sub-Saharan Africa: evidences from Douala in Cameroon. Afr Health Sci 2007;7:38-44. [PubMed]
- Braunwald E, Zipes DP, Libby P. eds. Heart Disease. A Textbook of Cardiovascular Medicine. 6th ed. Volume 1. Philadelphia: WB Saunders, 2001:554-5.
- Prendergast BD, Banning AP, Hall RJ. Valvular heart disease: recommendations for investigation and management. Summary of guidelines produced by a working group of the British Cardiac Society and the Research Unit of the Royal College of Physicians. J R Coll Physicians Lond 1996;30:309-15. [PubMed]
- Mbanya JC, Ngogang J, Salah JN, et al. Prevalence of NIDDM and impaired glucose tolerance in a rural and an urban population in Cameroon. Diabetologia 1997;40:824-9. [PubMed]
- Mbanya JC, Minkoulou EM, Salah JN, et al. The prevalence of hypertension in rural and urban Cameroon. Int J Epidemiol 1998;27:181-5. [PubMed]
- Cooper RS, Amoah AG, Mensah GA. High blood pressure: the foundation for epidemic cardiovascular disease in African populations. Ethn Dis 2003;13:S48-52. [PubMed]
- Unwin N. Non-communicable disease and priorities for health policy in sub-Saharan Africa. Health Policy Plan 2001;16:351-2. [PubMed]
- Amoah AG, Kallen C. Aetiology of heart failure as seen from a National Cardiac Referral Centre in Africa. Cardiology 2000;93:11-8. [PubMed]
- Mayosi BM. Contemporary trends in the epidemiology and management of cardiomyopathy and pericarditis in sub-Saharan Africa. Heart 2007;93:1176-83. [PubMed]
- Onwuchekwa AC, Asekomeh GE. Pattern of heart failure in a Nigerian teaching hospital. Vasc Health Risk Manag 2009;5:745-50. [PubMed]
- Magula NP, Mayosi BM. Cardiac involvement in HIV-infected people living in Africa: a review. Cardiovasc J S Afr 2003;14:231-7. [PubMed]
- Mayosi BM, Burgess LJ, Doubell AF. Tuberculous pericarditis. Circulation 2005;112:3608-16. [PubMed]
- Naeher LP, Brauer M, Lipsett M, et al. Woodsmoke health effects: a review. Inhal Toxicol 2007;19:67-106. [PubMed]
- Ezzati M, Kammen DM. The health impacts of exposure to indoor air pollution from solid fuels in developing countries: knowledge, gaps, and data needs. Environ Health Perspect 2002;110:1057-68. [PubMed]
- Bannerman CH, Mahalu W. Congenital heart disease in Zimbabwean children. Ann Trop Paediatr 1998;18:5-12. [PubMed]
- el Hag AI. Pattern of congenital heart disease in Sudanese children. East Afr Med J 1994;71:580-6. [PubMed]
- Ejim EC, Ike SO, Anisiuba BC, et al. Ventricular septal defects at the University of Nigeria Teaching Hospital, Enugu: a review of echocardiogram records. Trans R Soc Trop Med Hyg 2009;103:159-61. [PubMed]
- Marelli AJ, Mackie AS, Ionescu-Ittu R, et al. Congenital heart disease in the general population: changing prevalence and age distribution. Circulation 2007;115:163-72. [PubMed]
- Adewole AD, Ikem RT, Adigun AQ, et al. A three year clinical review of the impact of angiotensin converting enzyme inhibitors on the intra hospital mortality of congestive heart failure in Nigerians. Cent Afr J Med 1996;42:253-5. [PubMed]
- Bhagat K, Mazayi-Mupanemunda M. Compliance with medication in patients with heart failure in Zimbabwe. East Afr Med J 2001;78:45-8. [PubMed]
- Kingue S, Dzudie A, Menanga A, et al. A new look at adult chronic heart failure in Africa in the age of the Doppler echocardiography: experience of the medicine department at Yaounde General Hospital. Ann Cardiol Angeiol (Paris) 2005;54:276-83. [PubMed]
- Budzee A, Tantchou Tchoumi JC, Ambassa JC, et al. The Cardiac Center of Shisong Hospital: the first cardio-surgical center in West and Central Africa is inaugurated in Cameroon. Pan Afr Med J 2010;4:4. [PubMed]


