
Comparison of long-term outcomes of medical therapy and successful recanalisation for coronary chronic total occlusions in elderly patients: a report of 1,294 patients
Introduction
Percutaneous coronary intervention (PCI) of coronary chronic total occlusion (CTO) has remained a challenge despite the great progress in devices and skills. CTOs have been identified in up to 18% of all patients referred for diagnostic angiography and the prevalence of CTO rises with age (1,2). Most observational studies have shown that successful CTO-PCI was associated with an improvement of symptoms, left ventricular function, quality of life, and an increase in long-term survival compared with failed CTO-PCI (3-6). However, only approximately 10–20.7% of CTOs are currently undergoing attempted CTO-PCI (1,7), mainly because CTO-PCI procedures may be with lower procedural success rate, a higher expense and risk of procedural complication when compared with non-CTO elective PCI (8,9). Indeed, a substantial portion of CTO patients are treated with medical therapy (MT) instead of PCI (10,11).
In recent decades, life expectancy is increasing and the proportion of elderly people in the general population is growing. Elderly patients have a greater incidence of complex coronary arterial disease and other co-morbidities and a higher risk of postoperative complications (12). Therefore, elderly patients with CTOs were often treated by MT alone, and several studies also reported older patients have the lowest rates of revascularization (13,14). However, to date, elderly patients are regularly excluded from registries and randomized trials relevant to CTO and the clinical outcomes of successful CTO-PCI compared with MT for elderly CTO patients are limited (13). Moreover, most studies compared the outcomes of patients with successful versus unsuccessful procedures, rather than comparisons of successful CTO-PCI versus MT (15). Therefore, we investigated the long-term clinical outcomes of successful CTO-PCI versus MT in elderly patients with CTOs excluding patients with failed CTO-PCI.
Methods
Study population
This was a retrospective observational study. We consecutively enrolled 1,534 patients with at least one CTO from 2007 to 2016 at our institute. Among the patients, those who underwent failed CTO-PCI were excluded, and 1,294 patients were finally included in this analysis. Patients were grouped into the older group (≥65 years) and the younger group (<65 years). Each study group was divided according to the treatment strategy selected for the CTO: optimal MT versus successful CTO-PCI. Initial revascularization or MT was selected according to the presence of symptoms, viability in the CTO related territory, co-morbidity or high risk for revascularization, and the suitability of the target distal vessel for revascularization (diameter >2.5 mm); Canadian Cardiovascular Society (CCS) angina class of the patients were obtained to assess angina burden; myocardial viability and ischemia were assessed by two-dimensional echocardiography, cardiac magnetic resonance (CMR) or single-photon emission computed tomography (SPECT), which were reported in our previous published articles (16,17). Medical records and coronary angiography were reviewed to give the clinical, angiographic and procedural characteristics. We acquired the follow-up data through medical chart reviews or telephone interviews. The study outcomes will not affect the future management of the patients. The institutional review board approved the present study. The patient’s personal data have been secured.
Treatment strategy
MT comprised the use of β-blockers, angiotensin-converting enzyme inhibitor (ACEI) or angiotensin receptor blocker (ARB), nitrate and statins in addition to antiplatelets. Coronary interventions were performed using contemporary techniques. All patients without contraindications were given a loading dose of 300 mg of aspirin, 600 mg of clopidogrel before PCI. For patients with more than one CTO, only one CTO vessel was targeted and no further attempt was made during the study period. The choice of opening for CTO artery was based on localization of the occlusion and ischemia/viability in the CTO related territory by operators. After intervention, patients received and maintained dual-antiplatelet therapy for at least 12 months. All patients underwent two-dimensional echocardiography.
Definitions and study outcomes
A “CTO lesion” was defined as 100% stenosis with anterograde thrombolysis in myocardial infarction (MI) 0 flow for >3 months (3). Duration was estimated based on the onset of symptoms, history of MI consistent with the location of the occlusion or angiography or coronary CT. The “primary efficacy endpoint” was cardiac mortality. The “secondary outcome” was the incidence of major adverse cardiac event (MACE), including cardiac death, MI, and target vessel revascularization (TVR). Definitions of PCI success, cardiac death, MI, TVR and chronic kidney disease (CKD) had been described in our previous published article (16).
Statistical analysis
Continuous variables were presented as the mean ± standard deviation or median and quartile (25–75%) and compared with the Student’s t-test or Mann-Whitney U test. Categorical data were presented as percentages and were compared using the chi-square test or Fisher’s exact test. The Kruskal-Wallis test was used to compare non-parametric data. Propensity matching was performed to minimize any selection bias and maintain a balance in covariates between the two groups. The propensity scores were calculated by the using of a multivariable logistic regression model. Event-free survival during follow-up was evaluated according to the Kaplan-Meier method and survival among groups was compared using the log-rank test. Cox proportional hazards methods were used to estimate the independent effect of multiple independent variables on the risk of MACE. All univariate variables with P values <0.05 were included in the multivariate model. Stata Version 15.1 (StataCorp LLC, TX, USA) was used for all statistical analyses. For all tests, a P value of <0.05 was considered statistically significant.
Results
Characteristics of the study patients
Of the 1,294 patients with 1,520 CTOs, the younger group (age <65 years) included 664 (51.3%) patients, and the older group (age ≥65 years) included 630 (48.7%) patients. In the older group, they were divided into two groups: 421 in the MT group and 209 patients in the successful CTO-PCI group. In the younger group, they were divided into two groups: 379 patients in the MT group and 285 patients in the successful CTO-PCI group. There were five CTO-dedicated operators during this period.
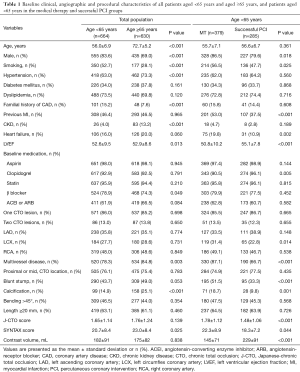
The baseline characteristics of the study population are described in Tables 1 and 2. Compared to patients <65 years, patients in the older group included more women and fewer smokers, and had more hypertension, CKD, multivessel disease and calcification; and were less likely to have familial history of coronary artery disease (CAD), with high SYNTAX score. As for medication, elderly patients were less often had taking β-blocker (Table 1).
Full table
Full table
In the younger group, male patients, smokers, previous MI, heart failure, CTO of left circumflex coronary artery (LCX), multivessel disease, blunt stump, calcification, high Japanese-chronic total occlusion (J-CTO) score and SYNTAX score were more prevalent in the MT group than in the successful CTO-PCI group, whereas high left ventricular ejection faction (LVEF) and taking clopidogrel were more common in the successful CTO-PCI (Table 1).
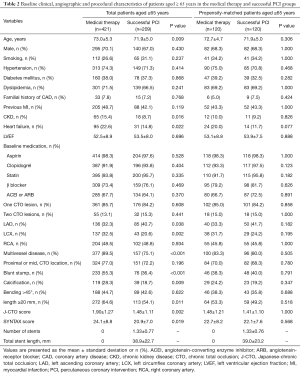
In the older group, patients in the MT group were older and more often had CKD and heart failure compared to the successful CTO-PCI group. As for lesion characteristics, CTO of LCX, multivessel disease, blunt stump, calcification, high J-CTO score and SYNTAX score were more frequently in the MT group than in the successful CTO-PCI group. CTO of the left anterior descending coronary artery were presented more frequently in patients in the successful CTO-PCI group compared with patients in the MT group (Table 2).
There were 120 matched pairs of patients after undertaking propensity score matching. No statistically significant differences were observed in clinical and lesion characteristics in the propensity score matched population between the MT and successful CTO-PCI groups (Table 2).
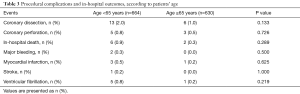
As for procedural complications and in-hospital outcomes, there were no significant differences in the prevalence of coronary dissection, coronary perforation, major bleeding, in-hospital death, MI, stroke and ventricular fibrillation (Table 3).
Full table
Clinical outcomes
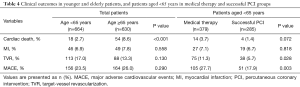
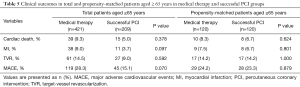
The median overall follow-up duration was 3.6 (IQR, 2.1–5.0) years. The cardiac death rate was higher in the older patients than in the younger patients (older vs. younger: 8.6% vs. 2.7%, P<0.001), but the MACE rate (older vs. younger: 26.0% vs. 23.5%, P=0.290) was comparable between the two groups. In the younger group, the occurrence of cardiac death (successful CTO-PCI vs. MT: 1.4% vs. 3.7%, P=0.072) was similar between the two groups, whereas the MACE rate (successful CTO-PCI vs. MT: 17.9% vs. 27.7%, P=0.003) was significantly higher in MT group (Table 4) (Figure 1).
Full table
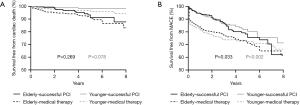
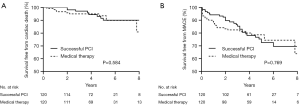
In the older group, no significant differences were observed between the successful CTO-PCI and MT groups in terms of cardiac death (successful CTO-PCI vs. MT: 5.0% vs. 9.3%, P=0.378) and MACE (15.1% vs. 28.3%, P=0.070). In propensity-matched patients, no significant differences were observed between the two groups in terms of cardiac death (successful CTO-PCI vs. MT: 6.7% vs. 8.3%, P=0.624) and MACE (23.3% vs. 24.2%, P=0.879) (Table 5) (Figures 1 and 2).
Full table
No significant interaction existed between age and treatment strategy with regarding to cardiac mortality (P=0.292). The cardiovascular survival benefit after successful CTO-PCI was similar in younger and older patients (Figure 3).
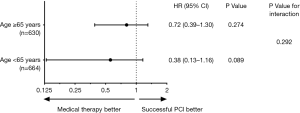
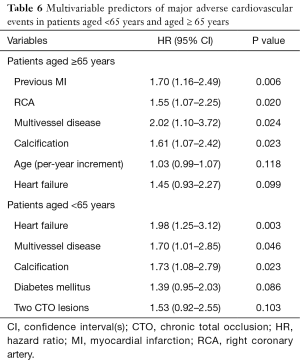
Table 6 shows independent predictors of MACE in elderly and younger patients. After multivariate analysis, previous MI [hazard ratio (HR) 1.70, 95% confidence interval (CI): 1.16–2.46, P=0.006], right coronary artery (HR 1.55, 95% CI: 1.07–2.25, P=0.020), multivessel disease (HR 2.02, 95% CI: 1.10–3.72, P=0.024) and calcification (HR 1.61, 95% CI: 1.07–2.42, P=0.023) were independent predictors of MACE in the elderly.
Full table
Discussion
We evaluated the long-term cardiovascular survival of MT versus successful CTO-PCI in elderly patients with CTOs. Several major findings emerge from this study: (I) elderly patients more often had CKD, calcification of CTO lesions and complex lesions; (II) successful CTO-PCI did not reduce cardiovascular mortality or MACE compared with MT alone in elderly patients with CTOs; (III) successful CTO-PCI was associated with a reduction in MACE in younger patients.
To the best of our knowledge, this is one of the largest observational studies reporting the effect of MT in unselected CTO patients aged ≥65 years. CTO is more commonly seen in the older population, and these patients often have multiple comorbidities, including CKD, peripheral artery disease and stroke, which increase the risks associated with PCI (1,12,18). In addition, elderly patients are known to have more extensive CAD, tortuosity and severe calcification of vessels (19,20). This increases the complexity of PCI and the risk of periprocedural complications (21). Interventional cardiologists are often reluctant to perform complex CTO-PCI in elderly patients because of the perception of poor clinical outcomes in this high-risk population even though the development of equipment and techniques has greatly improved the success rate of CTO-PCI. In our study, elderly patients indeed more often had CKD, calcification of CTO lesions and complex lesions compared with younger group, and these differences may result in a decreased CTO-PCI in elderly CTO patients.
In the Trial of Invasive versus Medical therapy in Elderly patients (TIME) trial conducted in patients with chronic stable angina, long-term survival, relief of angina and quality of life were similar for elderly patients assigned to invasive and medical treatment (22). Moreover, according to the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial, relief of angina and quality of life were also similar for elderly patients with chronic stable angina who were treated by MT and those who underwent PCI (23). Similarly, our study also suggested that PCI was not superior to MT in elderly patients with CTOs.
Most previous literature focused on the association of successful CTO revascularization with clinical outcome compared with failed CTO-PCI in patients who underwent PCI, and have shown a better efficacy in term of successful CTO-PCI (24,25). However, these studies did not include patients managed medically without a CTO-PCI attempt (15). Therefore, compared to previous studies, the strengths of our study may better reflect the clinical significance of PCI compared with MT alone in elderly patients with CTOs.
Until now, there is no widely accepted guideline or consensus on treating elderly CTO patients, and clinical outcome of CTO-PCI in this population is unknown. In the present study, we performed the propensity score matching to maintain a balance in covariates and reduce potential confounding factors and we found that successful CTO-PCI did not reduce the prevalence of cardiac death or MACE, as compared with MT alone among elderly patients with CTOs, consistent with the finding of Lee and his colleagues (26). Our previous studies also suggested that successful CTO-PCI was not associated with reduced MACE or cardiac death compared with MT (27,28). Hence, aggressive CTO-PCI in elderly patients with coronary CTOs should be determined carefully considering multiple comorbidities, lesional complexities and operative complications.
Study limitations
This study is limited by its observational nature, even though we have performed the propensity score matching to maintain a balance in covariates
Conclusions
In the treatment of elderly patients with CTOs, successful CTO-PCI is not associated with reduced the risk of cardiac death or MACE compared with MT alone. Aggressive CTO-PCI should be considered carefully among this population. Well-designed, large randomized clinical trials are needed to support this finding.
Acknowledgments
Funding: This work was supported by the China Cardiovascular Disease Alliance VG Youth Fund Project (No. 2017-CCA-VG-046), Beijing United Heart Foundation (No. BJUHFCSOARF201801-02) and Beijing Lisheng Cardiovascular Health Foundation (No. LHJJ20158521).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The institutional review board approved the present study.
References
- Fefer P, Knudtson ML, Cheema AN, et al. Current perspectives on coronary chronic total occlusions: the Canadian Multicenter Chronic Total Occlusions registry. J Am Coll Cardiol 2012;59:991-7. [Crossref] [PubMed]
- Grantham JA, Marso SP, Spertus J, et al. Chronic total occlusion angioplasty in the United States. JACC Cardiovasc Interv 2009;2:479-86. [Crossref] [PubMed]
- Sianos G, Werner GS, Galassi AR, et al. Recanalisation of chronic total coronary occlusions: 2012 consensus document from the EuroCTO club. EuroIntervention 2012;8:139-45. [Crossref] [PubMed]
- Sirnes PA, Myreng Y, Mølstad P, et al. Improvement in left ventricular ejection fraction and wall motion after successful recanalization of chronic coronary occlusions. Eur Heart J 1998;19:273-81. [Crossref] [PubMed]
- George S, Cockburn J, Clayton TC, et al. Long-term follow-up of elective chronic total coronary occlusion angioplasty: analysis from the U.K. Central Cardiac Audit Database. J Am Coll Cardiol 2014;64:235-43. [Crossref] [PubMed]
- Kirk Christensen M, Freeman PF, Rasmussen JG, et al. Chronic total coronary occlusion: treatment results. Scand Cardiovasc J 2017;51:197-201. [Crossref] [PubMed]
- Ladwiniec A, Allgar V, Thackray S, et al. Medical therapy, percutaneous coronary intervention and prognosis in patients with chronic total occlusions. Heart 2015;101:1907-14. [Crossref] [PubMed]
- Rathore S, Matsuo H, Terashima M, et al. Procedural and in-hospital outcomes after percutaneous coronary intervention for chronic total occlusions of coronary arteries 2002 to 2008: impact of novel guidewire techniques. JACC Cardiovasc Interv 2009;2:489-97. [Crossref] [PubMed]
- Gada H, Whitlow PL, Marwick TH. Establishing the cost-effectiveness of percutaneous coronary intervention for chronic total occlusion in stable angina: a decision-analytic model. Heart 2012;98:1790-7. [Crossref] [PubMed]
- Azzalini L, Jolicoeur EM, Pighi M, et al. Epidemiology, management strategies, and outcomes of patients with chronic total coronary occlusion. Am J Cardiol 2016;118:1128-35. [Crossref] [PubMed]
- Tomasello SD, Boukhris M, Giubilato S, et al. Management strategies in patients affected by chronic total occlusions: results from the Italian Registry of Chronic Total Occlusions. Eur Heart J 2015;36:3189-98. [Crossref] [PubMed]
- Formiga F, Ferrer A, Sanz H, et al. Patterns of comorbidity and multimorbidity in the oldest old: the Octabaix study. Eur J Intern Med 2013;24:40e44.
- Zhang HP, Ai H, Zhao Y, et al. Effect of Chronic Total Occlusion Percutaneous Coronary Intervention on Clinical Outcomes in Elderly Patients. Am J Med Sci 2018;355:174-82. [Crossref] [PubMed]
- Rosengren A, Wallentin L, Simoons M, et al. Age, clinical presentation, and outcome of acute coronary syndromes in the Euroheart acute coronary syndrome survey. Eur Heart J 2006;27:789-95. [Crossref] [PubMed]
- Godino C, Bassanelli G, Economou FI, et al. Predictors of cardiac death in patients with coronary chronic total occlusion not revascularized by PCI. Int J Cardiol 2013;168:1402-9. [Crossref] [PubMed]
- Guo L, Wu J, Zhong L, et al. Two-year clinical outcomes of medical therapy vs. revascularization for patients with coronary chronic total occlusion. Hellenic J Cardiol 2019. [Epub ahead of print]. [Crossref] [PubMed]
- Guo L, Lv HC, Zhong L, et al. Gender differences in long-term outcomes of medical therapy and successful percutaneous coronary intervention for coronary chronic total occlusions. J Interv Cardiol 2019. [Epub ahead of print]. [Crossref] [PubMed]
- Saltzman AJ, Stone GW, Claessen BE, et al. Long-term impact of chronic kidney disease in patients with ST-segment elevation myocardial infarction treated with primary percutaneous coronary intervention: The HORIZONS-AMI (Harmonizing Outcomes With Revascularization and Stents in Acute Myocardial Infarction) trial. JACC Cardiovasc Interv 2011;4:1011-9. [Crossref] [PubMed]
- Behan M, Dixon G, Haworth P, et al. PCI in octogenarians: Our centre ‘real world’experience. Age Ageing 2009;38:469-73. [Crossref] [PubMed]
- Hsu JT, Kyo E, Chu CM, et al. Impact of calcifcation length ratio on the intervention for chronic total occlusions. Int J Cardiol 2011;150:135-41. [Crossref] [PubMed]
- André R, Dumonteil N, Lhermusier T, et al. In-hospital and long-term outcomes after percutaneous coronary intervention for chronic total occlusion in elderly patients: A consecutive, prospective, single-centre study. Arch Cardiovasc Dis 2016;109:13-21. [Crossref] [PubMed]
- Pfisterer M. Long-term outcome in elderly patients with chronic angina managed invasively versus by optimized medical therapy: Four-year follow-up of the randomized Trial of Invasive versus Medical therapy in Elderly patients (TIME). Circulation 2004;110:1213-8. [Crossref] [PubMed]
- Boden WE, O’Rourke RA, Teo KK, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med 2007;356:1503-16. [Crossref] [PubMed]
- Tanaka Y, Takeshita S, Takahashi S, et al. Comparison of short- and long-term outcomes of percutaneous coronary intervention for chronic total occlusions between patients aged ≥75 years and those aged <75 years. Am J Cardiol 2013;112:761-6. [Crossref] [PubMed]
- Hoebers LP, Claessen BE, Dangas GD, et al. Long-term clinical outcomes after percutaneous coronary intervention for chronic total occlusions in elderly patients (≥75 years): five-year outcomes from a 1,791 patient multi-national registry. Catheter Cardiovasc Interv 2013;82:85-92. [Crossref] [PubMed]
- Lee SH, Yang JH, Choi SH, et al. Long-term clinical outcomes of medical therapy for coronary chronic total occlusions in elderly patients (≥75 years). Circ J 2015;79:1780-6. [Crossref] [PubMed]
- Guo L, Zhang SF, Wu J, et al. Successful recanalisation of coronary chronic total occlusions is not associated with improved cardiovascular survival compared with initial medical therapy. Scand Cardiovasc J 2019;53:305-11. [Crossref] [PubMed]
- Guo L, Zhong L, Chen K, et al. Long-term clinical outcomes of optimal medical therapy vs. successful percutaneous coronary intervention for patients with coronary chronic total occlusions. Hellenic J Cardiol 2018;59:281-7. [Crossref] [PubMed]


