Predictive value of exercise myocardial perfusion imaging in the Medicare population: the impact of the ability to exercise
Background
With the advent of effective medical therapy and sophisticated percutaneous and surgical coronary revascularization techniques, life expectancy of patients with coronary artery disease (CAD) has dramatically improved (1). Consequently, more Medicare patients are being referred for ECG gated single photon emission computed tomography myocardial perfusion imaging (MPI) studies using exercise (eMPI) and pharmacologic (pMPI) stress to evaluate the presence and extent of underlying atherosclerotic CAD.
In the United States, the proportion of the population over the age of 65 years is projected to increase from 12.4% in 2000 to 19.6% in 2030 (2). Although the elderly represent only 13% of the population, they consume approximately 36% of health care expenditures (3). Despite being major consumers of the health care dollar, the Medicare population has been under-represented in clinical trials assessing the utility of interventional and diagnostic strategies (4).
In this age of increasing Medicare costs, the role of non-invasive stress testing remains poorly defined in the elderly. A previous study demonstrated that exercise stress testing provides different prognostic information in middle aged vs. elderly men over the age of 75 years (5), and elderly patients are often unable to exercise or have contraindications to exercise stress testing (6-8). Several recent studies have combined both eMPI and pMPI test types in their outcomes evaluation in elderly patients (9-17); However, end systolic volume (ESV), stress ejection fraction (EF), functional capacity, and the impact of downstream revascularization were not consistently measured and analyzed. Therefore, it is unknown how functional capacity, EF, ESV, and the presence of ischemia interact to predict risk in elderly patients. We sought to determine the value of exercise MPI and clinical variables in predicting mortality in a large, diverse elderly patient population who underwent gated eMPI. Furthermore, we sought to assess the rate of downstream revascularization and outcomes in this large cohort.
Methods
Our institution’s IRB approved nuclear cardiology database prospectively records variables on all patients referred for MPI. A 17-segment model is used to semiquantitatively score rest and stress perfusion, EF, wall motion score and the subjective presence of left and right ventricular (RV) dilation are recorded (18).
A retrospective analysis of this database was performed to identify all patients who underwent adenosine pharmacological and exercise gated MPI between October 2004 and January 2008. The choice of MPI testing was made by the referring physician.
Clinical variables [age, gender, smoking history, diabetes, insulin use, hypertension, and history of coronary artery bypass grafting (CABG)], nuclear variables [stress EF, summed difference score (SDS), summed rest score (SRS), stress ESV, RV dilation, and the overall physician’s result of the test (abnormal, equivocal, or normal)] were recorded. All revascularization procedures [percutaneous intervention (PCI) or CABG] found within 90 days of the index MPI study were analyzed.
Gated MPI stress protocol
Patients undergoing eMPI were subjected to an appropriate exercise protocol guided by the individual patient’s functional capacity. Heart rate, blood pressure, and ECG were continuously monitored throughout both study types. All protocols, acquisition, processing, and display were performed in accordance with the Imaging Guidelines of the American Society of Nuclear Cardiology (19).
Stress and rest perfusion images were semi-quantitatively scored using a 17-segment model of the left ventricle using 4DMMPI software (Invia, Ann Arbor, Michigan) (18). Global summed stress score (SSS) and SRS were calculated by adding the scores of the 17 segments in the stress and resting images, respectively. Each segment was scored by an experienced physician certified by the Certification Board of Nuclear Cardiology or the American Board of Nuclear Medicine using a 5-point scoring system (0, normal; 1, equivocal; 2, moderate reduction of isotope uptake; 3, severe reduction of uptake; and 4, absence of detectable tracer uptake in a segment). On the basis of the number and severity of segments with scores >2, the observers judged the study results as normal, abnormal, or equivocal/non-diagnostic (20). Studies were deemed non-diagnostic due to poor study quality despite re-scanning and/or multiple reiterations due to severe attenuation artifacts, poor count statistics, significant adjacent gastro-intestinal activity, or motion artifacts causing image degradation.
Statistical analysis
The primary end-point was all-cause mortality (21). Continuous data are expressed as means ± standard deviation. Wilcoxon rank sum tests were used to analyze group differences for the continuous data. Categorical data are displayed as frequencies and percentages, and comparisons are made using Chi-square tests (Fisher exact tests if appropriate). Results were analyzed in three groups (normal, abnormal and equivocal). Transformations of the continuous measures (i.e., logarithmic, inverse, exponential) were assessed for proper calibration of risk factors with respect to outcome.
Overall and stratified nonparametric survival estimates were obtained by the Kaplan-Meier method. A parametric method was used to resolve the number of phases of instantaneous risk for death (hazard function) and to estimate the shaping parameters. Due to the quite constant phase of events following MPI, final multivariable models were created and presented using Cox proportional hazard models. In the mortality analyses, interactions of ESV with gender, age, and test result were all tested to assess any subgroup differences.
Bootstrap bagging with automated re-sampling and stepwise selection was used to determine reliable risk factors of mortality (22). Factors occurring in 50% or more of the bootstrap models were retained to form a final multivariable risk factor model. All variables were considered for the initial mortality analysis using 200 bootstrap runs. Mean imputation was used for missing data values. A second bootstrap analysis was done (200 additional runs) after excluding the individual segment scores to avoid confounding and focus on the summary scores for prediction. Statistical analyses were performed using SAS® version 9.1.
Follow-up
The average follow-up was 2.4±0.9 years (median 2.4 years). We searched the Social Security Death Index to identify deaths that occurred after the index MPI study during follow-up. All-cause mortality has been shown to be a more objective and unbiased endpoint than “cardiac mortality” (21). Furthermore, competing non-cardiovascular mortality risk in this elderly population is important. We also looked at 90-day percutaneous or surgical revascularization for the whole group.
Results
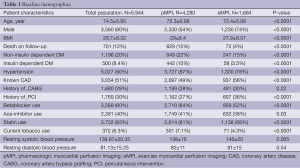
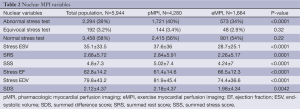
The clinical and MPI findings and characteristics for the overall study population are listed in Tables 1 and 2. There were 1,644 patients in our study population that underwent eMPI (74% male and a mean age of 72.4±5.1 years). Amongst the patients that underwent exercise MPI, there were 103 deaths during the follow-up time (See Table 1).
Full table
Full table
There were 573 (34%) total abnormal exercise MPI studies, and 48 (3%) equivocal studies. Subsequent revascularization was performed on 121/573 (21%) patients with abnormal exercise MPI and 15/1,043 (1%) in the normal exercise MPI group within 90 days (Figure 1).
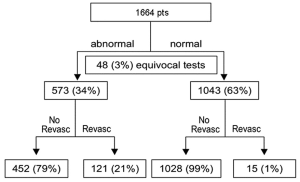
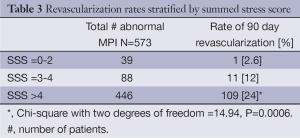
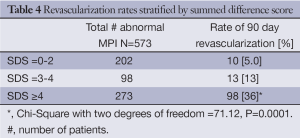
The rates of revascularization based on reported SSS and SDS is summarized in Tables 3 and 4. It is clear that the size of the perfusion defect as assessed by SDS and SSS influenced down stream revascularization.
Full table
Full table
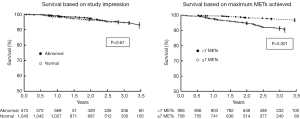
There was no difference in mortality in patients with abnormal MPI vs. those with normal perfusion studies (Figure 2). The standard MPI variables, except for ESV, failed to risk-stratify elderly patients who were able to exercise. The maximum METs ranged from 2.4 to 14.5 (25% of the patients achieved <6.3 METs, and 25% achieved >8.7 METs), with a mean of 7.4±1.8 METs in this population.
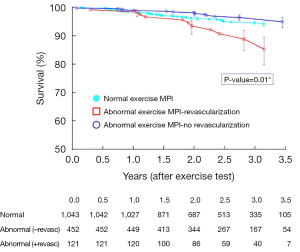
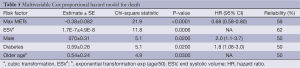
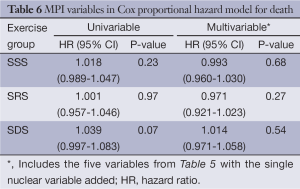
The maximum METs achieved was the most powerful predictor of death amongst patients who were able to exercise. Patients who were able to exercise ≤7 METs (n=758) had significantly worse survival compared those who were able to exercise >7 METs (n=906) (log-rank P<0.0001) (Figure 2). Patients with abnormal scans who underwent subsequent revascularization had worse survival compared to those who had abnormal scans but were not revascularized at 2.4 years of follow-up (Figure 3; log rank P-value =0.01). The independent predictors of survival for patients undergoing MPI are listed in Table 5. A high ESV, male gender, diabetes, and older age were also independently associated with worse survival. No other nuclear variables were independent predictors of mortality. Table 6 lists the MPI variables in Cox proportional hazard model for death, which were not significantly associated with mortality in our study.
Full table
Full table
Discussion
In this study, we evaluated the prognostic value of clinical and MPI variables in elderly patients undergoing MPI as well as the rates and outcomes of subsequent revascularization. Our study is the a large observational study in the modern era of medical therapy that shows that elderly patients (mean age 75) who are able to exercise have excellent prognosis, despite an abnormal MPI test result. The only MPI variable that predicted mortality in this group was a higher ESV. Furthermore, patients who achieved greater than seven METs had significantly improved outcomes compared to those who achieved ≤7 METs. However, the overall MPI test result when dichotomized into normal vs. abnormal did not provide any further risk stratification in those with less functional capacity.
Our study also demonstrated that as expected when patients have a larger perfusion defect, a higher rate of revascularization was seen. For instance patients with limited or no ischemia had only 5% chance of revascularization at 90 days versus a 36% chance when the amount of ischemia was large (Table 4). However, a limited impact of revascularization on short-term mortality was observed, particularly in patients who can exercise. In fact, patients with abnormal exercise MPI who subsequently underwent revascularization had worse outcomes than those who did not, suggesting that the early procedural hazard was not associated with downstream survival benefit at the time of follow up.
MPI in the middle-aged population has been shown to provide incremental prognostic value for predicting cardiac events and death in patients with known or suspected CAD. One meta-analysis demonstrated that both age and the inability to complete an exercise test are independent and negative prognostic indicators in patients with CAD (23). These data cannot be translated to the Medicare population given the co-morbidities present as well as the competing mortality risk from other disease processes. A recent study of elderly patients undergoing MPI demonstrated the utility of MPI in elderly patients over the age of 75 years (13). However, this retrospective study analyzed patients who underwent MPI between 1991 and 1999, and it is unclear if these patients were treated with modern medical therapy. Furthermore, the study population had relatively mild perfusion defects, and the study did not distinguish between differences in outcomes after subsequent revascularization based on the type of stress testing (exercise vs. pharmacologic), or functional capacity. Several smaller studies have also examined the prognostic value of MPI in the elderly (9-12,15,16,24,25); however, our study is novel in that it demonstrates the neutralizing effect of the ability to exercise in patients with abnormal MPI in an older patient population.
We also demonstrated that maximum METs achieved was the most powerful independent predictor of mortality, even more powerful than age and abnormal MPI findings, in this patient population. This finding contradicts previous smaller studies and conventional thinking that MPI findings should provide incremental information over functional capacity in this patient population (9,11,23,25). However, our findings are supported by three other studies. The first examined the utility of MPI as well as exercise treadmill testing (ETT) in 626 outpatients age 65 and older, mean age 70.7 years. This study found that age, gender, exercise tolerance, and ischemia were independent predictors of death (25). ROC curve analysis in this study for the prediction of future events demonstrated the area under the curve to be 0.659 for patient age and sex; 0.715 for age, sex, and treadmill time (P=0.048 vs. age and sex); and 0.721 for age, sex, treadmill time, and MPI ischemia (P=0.027 vs. age and sex but P=NS vs. age, sex, and treadmill time). Therefore, this suggests that after age, sex, and exercise tolerance were determined, the addition of ischemia of assessment by MPI offered relatively small incremental value. The other evaluated 514 elderly patients (≥65 yrs) who underwent ETT and demonstrated that workload alone was the only ETT variable that was independently associated with outcomes (26). Furthermore, Sui et al. evaluated a cohort of 2,603 patients over the age of 60 years and found that poor cardiorespiratory fitness was a powerful predictor of mortality (27).
Our study demonstrates that traditionally accepted prognostic nuclear variables are not as useful in the Medicare population undergoing MPI. Clinical variables, ESV, and functional capacity provided the most prognostic information in terms of all-cause mortality. It is important to note that ESV was the only MPI variable that was predictive of survival, which was also recently demonstrated in a recent study by Doyle et al. (28).
Older patients with stable CAD who undergo interventions represent a substantial expenditure without proof of benefit (29). As the population continues to age, the potential financial burden of increasing nuclear imaging studies and possible subsequent interventions may be significant. Therefore, the prognostic benefit needs to be closely scrutinized. Our study again raises the question of prognostic benefit of such procedures, particularly in older patients who can exercise. With recent studies such as the COURAGE trial (30), the there is little justification for spending resources on stress imaging to guide subsequent revascularizations in elderly patients with stable CAD. The randomized Trial of Invasive versus Medical therapy in Elderly patients (TIME) trial demonstrated only a significant reduction in anginal symptoms and subsequent hospitalizations, but no significant improvement in mortality, in patients who were revascularized versus those who were treated medically (31). Therefore, in older patients without symptoms, stress imaging and subsequent revascularization for abnormal findings may not provide any prognostic benefit. Furthermore, in patients who are able to exercise, an abnormal MPI does not appear to impact survival or provide any further risk stratification. In an era of increasing Medicare and budgetary financial constraints and with the explosion of proven pharmaceutical therapeutic primary and secondary prevention tools (Asprin, betablockers, ACE inhibitors, Clopidogrel and statins), the utility of non-invasive stress testing in the Medicare population needs to be further scrutinized.
Limitations
Selection bias may be a significant limitation in our study. Our patients were referred for MPI at a tertiary-care medical center, and may have more co-morbidities than the typical patient of similar age, however we included all patients (both ambulatory and hospitalized patients) who presented for evaluation. Subsequent myocardial infarction and cardiac hospitalization were not recorded in this study. Another limitation is that 90-day revascularization status was based upon knowledge of CABG and PCI performed at our institution. Active follow-up was not used in the analysis of revascularization; however, from our clinical practice patterns, we assume that >90% of this patient cohort would have returned here for care and only a few early interventions would have been missed. Statistical comparisons and long-term evaluation of the effect of revascularization would need active follow-up and a more appropriate competing risk analysis.
Conclusions
In our study population, perfusion defects on MPI lacked the ability to provide incremental risk stratification. The ability to exercise and the number of METs achieved seem to neutralize the impact of MPI results on mortality. In this setting, patients who are able to exercise have excellent outcomes, despite abnormal MPI findings. As expected, the results of MPI influenced the rate of revascularization. However, revascularization in patients who can exercise even when faced with an abnormal MPI failed to be protective. The assumption that MPI in older patients can be further risk stratify patients beyond exercise capacity in the modern era needs to be tested in a prospective trial.
Acknowledgements
DHK, PH, and WAJ had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Disclosure: Dr. Kwon is a consultant for Astellas. Dr. Manuel Cerqueira is on the Scientific Advisory Board and Speakers Bureau for Astellas Pharma USA. None of the other authors have conflicts of interests that would bias the analysis of our study.
References
- Foot DK, Lewis RP, Pearson TA, et al. Demographics and cardiology, 1950-2050. J Am Coll Cardiol 2000;35:66B-80B. [PubMed]
- Konstam MA, Patten RD, Thomas I, et al. Effects of losartan and captopril on left ventricular volumes in elderly patients with heart failure: results of the ELITE ventricular function substudy. Am Heart J 2000;139:1081-7. [PubMed]
- Senior R, Basu S, Kinsey C, et al. Carvedilol prevents remodeling in patients with left ventricular dysfunction after acute myocardial infarction. Am Heart J 1999;137:646-52. [PubMed]
- Weintraub WS, Boden WE, Zhang Z, et al. Cost-effectiveness of percutaneous coronary intervention in optimally treated stable coronary patients. Circ Cardiovasc Qual Outcomes 2008;1:12-20. [PubMed]
- Kwok JM, Miller TD, Hodge DO, et al. Prognostic value of the Duke treadmill score in the elderly. J Am Coll Cardiol 2002;39:1475-81. [PubMed]
- Fletcher GF, Balady GJ, Amsterdam EA, et al. Exercise standards for testing and training: a statement for healthcare professionals from the American Heart Association. Circulation 2001;104:1694-740. [PubMed]
- Gibbons RJ, Balady GJ, Bricker JT, et al. ACC/AHA 2002 guideline update for exercise testing: summary article. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1997 Exercise Testing Guidelines). J Am Coll Cardiol 2002;40:1531-40. [PubMed]
- Gibbons RJ, Balady GJ, Beasley JW, et al. ACC/AHA Guidelines for Exercise Testing. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Exercise Testing). J Am Coll Cardiol 1997;30:260-311. [PubMed]
- De Winter O, Velghe A, Van de Veire N, et al. Incremental prognostic value of combined perfusion and function assessment during myocardial gated SPECT in patients aged 75 years or older. J Nucl Cardiol 2005;12:662-70. [PubMed]
- Lima RS, De Lorenzo A, Pantoja MR, et al. Incremental prognostic value of myocardial perfusion 99m-technetium-sestamibi SPECT in the elderly. Int J Cardiol 2004;93:137-43. [PubMed]
- Valeti US, Miller TD, Hodge DO, et al. Exercise single-photon emission computed tomography provides effective risk stratification of elderly men and elderly women. Circulation 2005;111:1771-6. [PubMed]
- Zafrir N, Mats I, Solodky A, et al. Characteristics and outcome of octogenarian population referred for myocardial perfusion imaging: comparison with non-octogenarian population with reference to gender. Clin Cardiol 2006;29:117-20. [PubMed]
- Hachamovitch R, Kang X, Amanullah AM, et al. Prognostic implications of myocardial perfusion single-photon emission computed tomography in the elderly. Circulation 2009;120:2197-206. [PubMed]
- Kawamura M, Ohta Y, Katoh K, et al. Medium- to long-term prognostic impact of dipyridamole thallum-201 myocardial single-photon emission computed tomography in elderly patients. Circ J 2003;67:913-7. [PubMed]
- Nagao T, Chikamori T, Hida S, et al. Quantitative gated single-photon emission computed tomography with (99m)Tc sestamibi predicts major cardiac events in elderly patients with known or suspected coronary artery disease: the QGS-Prognostic Value in the Elderly (Q-PROVE) Study. Circ J 2007;71:1029-34. [PubMed]
- Schinkel AF, Elhendy A, Biagini E, et al. Prognostic stratification using dobutamine stress 99mTc-tetrofosmin myocardial perfusion SPECT in elderly patients unable to perform exercise testing. J Nucl Med 2005;46:12-8. [PubMed]
- Johnson NP, Schimmel DR Jr, Dyer SP, et al. Survival by stress modality in patients with a normal myocardial perfusion study. Am J Cardiol 2011;107:986-9. [PubMed]
- Cerqueira MD, Weissman NJ, Dilsizian V, et al. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Int J Cardiovasc Imaging 2002;18:539-42. [PubMed]
- Berman DS, Kiat H, Friedman JD, et al. Separate acquisition rest thallium-201/stress technetium-99m sestamibi dual-isotope myocardial perfusion single-photon emission computed tomography: a clinical validation study. J Am Coll Cardiol 1993;22:1455-64. [PubMed]
- Berman DS, Hachamovitch R, Kiat H, et al. Incremental value of prognostic testing in patients with known or suspected ischemic heart disease: a basis for optimal utilization of exercise technetium-99m sestamibi myocardial perfusion single-photon emission computed tomography. J Am Coll Cardiol 1995;26:639-47. [PubMed]
- Lauer MS, Blackstone EH, Young JB, et al. Cause of death in clinical research: time for a reassessment? J Am Coll Cardiol 1999;34:618-20. [PubMed]
- Efron B, Tibshirani RJ. eds. An Introduction to the Boostrap. New York: Chapman and Hall/CRC, 1998.
- Navare SM, Mather JF, Shaw LJ, et al. Comparison of risk stratification with pharmacologic and exercise stress myocardial perfusion imaging: a meta-analysis. J Nucl Cardiol 2004;11:551-61. [PubMed]
- Curtis JP, Ko DT, Wang Y, et al. The prognostic value of vasodilator myocardial perfusion imaging in octogenarians. Am J Geriatr Cardiol 2004;13:239-45. [PubMed]
- Steingart RM, Hodnett P, Musso J, et al. Exercise myocardial perfusion imaging in elderly patients. J Nucl Cardiol 2002;9:573-80. [PubMed]
- Goraya TY, Jacobsen SJ, Pellikka PA, et al. Prognostic value of treadmill exercise testing in elderly persons. Ann Intern Med 2000;132:862-70. [PubMed]
- Sui X, LaMonte MJ, Laditka JN, et al. Cardiorespiratory fitness and adiposity as mortality predictors in older adults. JAMA 2007;298:2507-16. [PubMed]
- Doyle M, Weinberg N, Pohost GM, et al. Left ventricular energy model predicts adverse events in women with suspected myocardial ischemia: results from the NHLBI-sponsored women’s ischemia syndrome evaluation (WISE) study. Cardiovasc Diagn Ther 2013;3:64-72. [PubMed]
- Agarwal S, Banerjee S, Tuzcu EM, et al. Influence of age on revascularization related costs of hospitalization among patients of stable coronary artery disease. Am J Cardiol 2010;105:1549-54. [PubMed]
- Boden WE, O’Rourke RA, Teo KK, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med 2007;356:1503-16. [PubMed]
- Pfisterer M. Trial of Invasive versus Medical therapy in Elderly patients Investigators. Long-term outcome in elderly patients with chronic angina managed invasively versus by optimized medical therapy: four-year follow-up of the randomized Trial of Invasive versus Medical therapy in Elderly patients (TIME). Circulation 2004;110:1213-8. [PubMed]