Compliance of pharmacological treatment for non-ST-elevation acute coronary syndromes with contemporary guidelines: influence on outcomes
Introduction
Non-ST-elevation acute coronary syndromes (NSTE-ACS) are associated with an increase risk of death and several other cardiovascular complications (1). However, over the last years, advances in cardiovascular care have resulted in a decline in mortality and morbidity associated with NSTE-ACS (2-4). Strong evidence shows that the best therapeutic strategies for these patients are not always followed, suggesting that outcomes of NSTE-ACS patients are not as good as they could be with better translation of the best scientific knowledge into clinical practice (5). This reality has been well demonstrated in the CRUSADE initiative (6) and in the Euro Heart Survey ACS (7). Thus, NSTE-ACS remains an important cause of premature mortality and morbidity with a considerable economic impact due to both direct and indirect costs.
The successful implementation of clinical guidelines, incorporating new treatments into practice, has been challenging and the adherence to the evidence-based treatment and its implications after ACS are poorly defined (8-11).
The aim of this study is to assess the compliance of NSTE-ACS patients with management Guidelines and to evaluate its impact on hospital outcomes.
Methods
Study design and population
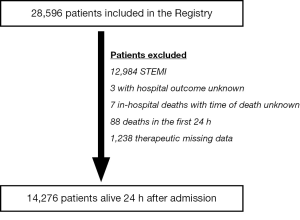
All consecutive patients included in the Portuguese Registry on Acute Coronary Syndromes (ProACS) between January 1, 2002 and August 31, 2011 were eligible. This is a continuous, prospective and observational registry, with 46 participating centres that are cardiology departments of hospitals in the main land territory, and the Madeira and Azores islands (12,13). For the purpose of the present study, only patients with NSTE-ACS were included. A diagnosis of non-ST-elevation myocardial infarction (NSTEMI) was established according to the universal definition criteria for type 1 myocardial infarction (14). Those patients who died during the first 24 hours of hospitalization were excluded because of their intrinsic low likelihood of receiving certain evidence-based therapies, such as beta-blockers and angiotensin converting enzyme (ACE) inhibitors.
Data collected
All data were registered in a dedicated computer database, including demographic, clinical, patient management-related characteristics, as well as clinical outcomes. Compliance with Guidelines for the management of NSTE-ACS (15) was classified according to the value of a therapeutic score (ThSc) based on the recommended pharmacological therapies received during hospitalization. This guideline-adherence score comprised the following treatments: aspirin, clopidogrel, heparin, beta-blocker, ACE-inhibitor and statin. For each of these drugs one point was assigned if taken and zero if not. Total therapeutic compliance was defined as a ThSc of six points (i.e., highest possible score). All decisions regarding the patient management strategy, including referral for coronary angiography and performance of myocardial revascularization, via percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG), were left to the discretion of the attending physician and the site-specific protocols. All-cause death during the index hospitalization was used to assess the prognostic value of compliance with guideline-based treatment of NSTE-ACS.
Statistical analysis
Means and standard deviations (mean ± SD) were used to describe continuous variables with normal distribution, and percentages for categorical variables. Normality was tested with the Kolmogorov-Smirnov test. Differences between baseline characteristics and outcomes were evaluated with the chi-square test (or Fisher’s exact test, when appropriate) for categorical variables and the t-test for continuous variables. Adjusted risk estimates were obtained from a Cox logistic regression model (goodness of fit by Hosmer and Lemeshow test), which included all demographic (age; gender), clinical (atherothrombotic risk factors; prior history of myocardial infarction, PCI or CABG; prior stroke or transient ischemic attack; clinical peripheral arterial disease; baseline Killip-Kimball class), electrocardiographic (ST-segment depression on presentation) and biochemical marker (NSTEMI diagnosis) variables with a potential impact on the study endpoint. In the Cox model, the model assumptions (i.e., proportional hazards, linearity of continuous covariates, and lack of interactions) were found to be valid. Receiver operator characteristic (ROC) curve analysis (c-statistic) was used to identify the predictive accuracy of the ThSc for in-hospital death with determination of the area under the curve (AUC), sensitivity and specificity. Two-tailed tests of significance are reported. For all comparisons, a P value <0.05 was considered statistically significant. When appropriate, 95% confidence intervals (CI) were calculated. Statistical analysis was performed with SPSS version 19.0 (SPSS Inc., Chicago, IL, USA).
Results
Of the 28,596 patients included in the Registry during the study period, 14,083 were excluded. The final analysis comprised a total of 14,276 patients (Figure 1).
Baseline characteristics of the study cohort are shown in the Table 1. The mean age is 67.6±12.3 years, most patients are male (67.1%) and the presence of atherothrombotic risk factors and clinically overt cardiovascular disease is common: over two thirds have a history of hypertension and a quarter of myocardial infarction; 16.4% have undergone myocardial revascularization via PCI or CABG. Prior use of aspirin, beta-blocker, ACE-inhibitor, and statin is relatively low.
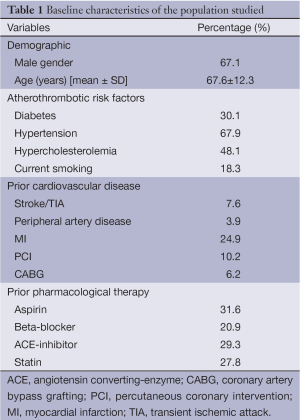
Full table
Regarding the clinical presentation at hospital admission, almost half of the patients (45.5%) were symptomatic with typical chest pain at rest on admission, 77.5% referred at least one episode of angina at rest lasting more than 20 minutes and 34.4% referred recurrent episodes of angina. Physical signs of heart failure (Killip-Kimball class >1) were present in 19.2% patients at admission. The most common type of NSTE-ACS was NSTEMI (77.4%): ST-segment depression was detected on the baseline electrocardiogram (ECG) in 36.6% patients.
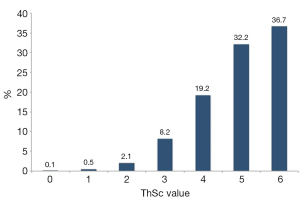
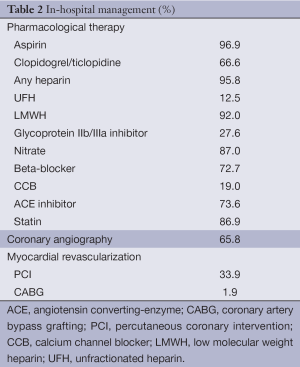
In-hospital management is described in Table 2. A heparin was prescribed in 95.8% patients, aspirin in 96.9%, a thienopyridine in 66.6%, a beta-blocker in 72.7%, an ACE-inhibitor in 73.6% and a statin in 86.8%. The mean ThSc was 4.9±1.1 and 36.7% patients had total compliance (i.e., ThSc =6).
Full table
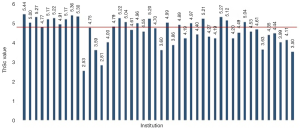
Figure 2 shows the distribution of all patients according to the ThSc value. Figure 3 presents the mean value of ThSc per study site. The mean ThSc was significantly higher in sites with PCI capacity (5.0±1.0 vs. 4.8±1.1, P<0.001) as was the rate of total compliance (41.1% vs. 30.8%, P<0.001). Coronary angiography was performed in 66.8% patients and 35.8% underwent myocardial revascularization (PCI 33.9% and CABG 1.9%) during the index hospitalization.
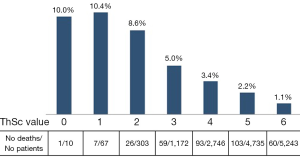
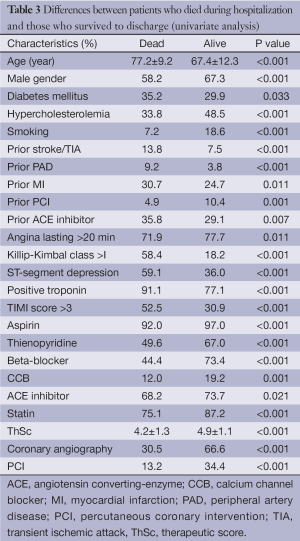
The incidence of in-hospital death was 2.4% (354 deaths). Patients who survived to hospital discharge differed significantly from those who died with respect to clinical characteristics (Table 3). Mean ThSc was higher among patients who survived (4.9±1.1 vs. 4.2±1.3, P<0.001). In-hospital mortality was inversely distributed according to the value of ThSc (Figure 4) and was similar in sites with and without PCI capacity (2.3% vs. 2.7%, P=0.107).
Full table
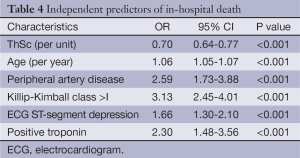
Table 4 shows the results of the multivariable analysis for identifying the independent predictors of in-hospital mortality. ThSc was independently associated with higher in-hospital survival (OR 0.70, 95% CI, 0.64-0.77; P<0.001). Age, peripheral artery disease, Killip-Kimball class >I, ECG with ST-segment depression and positive troponin were independent predictors of in-hospital death.
Full table
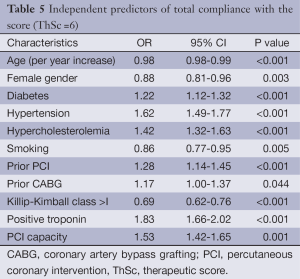
In a ROC curve analysis, ThSc showed a good predictive accuracy for the occurrence of in-hospital death: AUC =0.82 (95% CI, 0.80-0.84; P<0.001), sensitivity 71.6%, and specificity 78.0%. Table 5 presents the independent predictors of total compliance with the score of recommended therapies (ThSc =6). Among these are the majority of the traditional cardiovascular risk factors, previous myocardial revascularization, positive troponin, and admission to a site with PCI capacity. Older patients, women, smokers and patients with heart failure at admission (Killip-Kimball class >I) were less likely to be associated with total compliance with the score.
Full table
Discussion
The present study shows that compliance with evidence-based medical therapy in patients admitted with NSTE-ACS is strongly associated with lower hospital mortality. For each evidence-based drug class included in the management of the patient, hospital mortality was 30% lower than in patients who did not receive the drug. Patients receiving all recommended therapies had the highest rate of survival to discharge. Yet, this latter group comprised only 36.7% of patients, thus showing that recommended therapy is not delivered to the majority of NSTE-ACS patients.
Over the past years, the use of evidence-based therapies with proven efficacy in reducing morbidity and mortality in patients with cardiovascular diseases has increased significantly (16-18), yet large room for improvement persists. In the setting of ACS, adherence to evidence-based therapies is lower in patients with NSTEMI compared to those with ST-elevation myocardial infarction (19). Guidelines on NSTE-ACS have undergone several revisions since 2002, when this registry began including patients. Nevertheless, the six pharmacological interventions used in the present score were already recommended in the Guidelines of European Society of Cardiology (20).
Better quality of care is expected to favorably impact on the economic and social burdens of ischemic heart disease (21). Data regarding the association between clinical performance and outcomes are limited. Peterson et al. (22) showed in ACS patients that every 10% increase in composite adherence at a hospital was independently associated with an analogous 10% decrease in the patients’ likelihood of in-hospital mortality. As in the study by Roe MT et al. (23), in our experience, patients with highest risk are less likely to receive guideline-recommended therapies and interventions. Such patients include those with heart failure manifestations at admission, older patients and smokers. Patients with a higher baseline risk of adverse outcomes are expected to have a greater absolute benefit from aggressive therapies. Women and elderly patients were also less likely to receive evidence-based therapies, as demonstrated in the CRUSADE Quality Improvement Initiative (24). Several factors may explain this finding in these subgroups of patients, namely the higher frequency of comorbidities, contra-indications for drug therapy and atypical symptoms. In our study, centres with PCI capacity showed better adherence to guideline recommendations, a finding also previously reported (24).
Our data also suggest that the use of guideline-based process measures may be an important means of assessing quality of care, and this hypothesis deserves further study. Nevertheless, there is considerable debate regarding the ideal methodologies for assessing clinical performance (25). Quality of care may be improved by the use of tools that facilitate the implementation of guideline recommendations at different levels, namely the institution, the care provider, and the patient (26). Quality of care can be evaluated in three domains: structure (aspects that exist independently of the patient), process (actions performed in delivering care), and outcomes (events that occur as a result of the disease process and/or care provided) (27). Several indicators are recommended to measure and improve the quality of care for this patient population, indicators that should be reliable and feasible to use, with clear and concise definitions (25). Among the criteria used, some authors advocate that patient outcomes, as in-hospital death defined in our study, should be the standard and preferential criteria for assessing hospital quality. Ideally, multiple metrics will be needed to characterize hospital performance, depending and adjusted to the target population and the specifications of each institution.
Our study has some limitations. This is an observational and nonrandomized study. Data on potential contraindications to guideline recommendations and previously experienced untoward reactions to therapy were not collected, and both conditions may have influenced treatment choices and patient outcomes. Nevertheless, it should be noted that certain drugs are often not prescribed because of comorbidities, despite the available evidence of benefit in their presence. The prognostic impact of evidence-based care was assessed at the individual patient level, but practice patterns tend to cluster at the institutional level. Additionally, this study is focused on pharmacological therapies with prognostic impact, and does not assess compliance with respect to recommendations on the use of coronary angiography and myocardial revascularization, which are also known to modify outcomes when appropriate.
In conclusion, our study in a large population included in a national registry shows that current NSTE-ACS care is not perfect and guideline-based therapy is associated with improvement in hospital outcomes. In addition to several patient related-characteristics, process care and institutional related-variables influence the prognosis. Some of the patients with highest mortality risk were less likely to receive guideline-recommended therapies. These findings highlight the need to promote using the guideline and to develop approaches for quality improvement in this subset of patients. Although the improvement in guideline adherence over the last years, continuous quality assessment policies are needed to overcome the gap between evidence and practice.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Lloyd-Jones D, Adams R, Carnethon M, et al. Heart disease and stroke statistics-2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 2009;119:480-6. [PubMed]
- Yeh RW, Sidney S, Chandra M, et al. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med 2010;362:2155-65. [PubMed]
- Fox KA, Eagle KA, Gore JM, et al. The Global Registry of Acute Coronary Events, 1999 to 2009--GRACE. Heart 2010;96:1095-101. [PubMed]
- Terkelsen CJ, Lassen JF, Norgaard BL, et al. Mortality rates in patients with ST-elevation vs. non-ST-elevation acute myocardial infarction: observations from an unselected cohort. Eur Heart J 2005;26:18-26. [PubMed]
- Peterson ED, Roe MT, Mulgund J, et al. Association between hospital process performance and outcomes among patients with acute coronary syndromes. JAMA 2006;295:1912-20. [PubMed]
- Hoekstra JW, Pollack CV Jr, Roe MT, et al. Improving the care of patients with non-ST-elevation acute coronary syndromes in the emergency department: the CRUSADE initiative. Acad Emerg Med 2002;9:1146-55. [PubMed]
- Mandelzweig L, Battler A, Boyko V, et al. The second Euro Heart Survey on acute coronary syndromes: characteristics, treatment, and outcome of patients with ACS in Europe and the Mediterranean Basin in 2004. Eur Heart J 2006;27:2285-93. [PubMed]
- Vikman S, Airaksinen KE, Peuhkurinen K, et al. Gap between guidelines and management of patients with acute coronary syndrome without persistent ST elevation. Finnish prospective follow-up survey. Scand Cardiovasc J 2003;37:187-92. [PubMed]
- Fermann GJ, Raja AS, Peterson ED, et al. Early treatment for non-ST-segment elevation acute coronary syndrome is associated with appropriate discharge care. Clin Cardiol 2009;32:519-25. [PubMed]
- Spinler SA. Managing acute coronary syndrome: evidence-based approaches. Am J Health Syst Pharm 2007;64:S14-24. [PubMed]
- Vikman S, Airaksinen KE, Tierala I, et al. Improved adherence to practice guidelines yields better outcome in high-risk patients with acute coronary syndrome without ST elevation: findings from nationwide FINACS studies. J Intern Med 2004;256:316-23. [PubMed]
- Ferreira J, Monteiro P, Mimoso J. National registry of acute coronary syndromes: results of the hospital phase in 2002. Rev Port Cardiol 2004;23:1251-72. [PubMed]
- Santos JF, Aguiar C, Gavina C, et al. Portuguese registry of acute coronary syndromes: seven years of activity. Rev Port Cardiol 2009;28:1465-500. [PubMed]
- Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction. Eur Heart J 2012;33:2551-67. [PubMed]
- Hamm CW, Bassand JP, Agewall S, et al. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. The Task Force for the management of acute coronary syndromes (ACS) in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 2011;32:2999-3054. [PubMed]
- Eagle KA, Moyntoye CK, Riba AL, et al. Guidelines-based standardized care is associated with substantially lower mortality in medicare patients with acute myocardial infarction: the American College of Cardiology’s Guidelines Applied in Practice (GAP) Projects in Michigan. J Am Coll Cardiol 2005;46:1242-8. [PubMed]
- Higashi T, Shekelle PG, Adams JL, et al. Quality of care is associated with survival in vulnerable older patients. Ann Intern Med 2005;143:274-81. [PubMed]
- Amsterdam EA, Peterson ED, Ou FS, et al. Comparative trends in guidelines adherence among patients with non-ST-segment elevation acute coronary syndromes treated with invasive versus conservative management strategies: Results from the CRUSADE quality improvement initiative. Am Heart J 2009;158:748-754.e1.
- Roe MT, Parsons LS, Pollack CV Jr, et al. Quality of care by classification of myocardial infarction treatment patterns for st-segment elevation vs non-ST-segment elevation myocardial infarction. Arch Intern Med 2005;165:1630-6. [PubMed]
- Bertrand ME, Simoons ML, Fox KA, et al. Management of acute coronary syndrome in patients presenting without persistent ST-segment elevation. Eur Heart J 2002;23:1809-40. [PubMed]
- Liu JL, Maniadakis N, Gray A, et al. The economic burden of coronary heart disease in the UK. Heart 2002;88:597-603. [PubMed]
- Peterson ED, Roe MT, Mulgund J, et al. Association between hospital process performance and outcomes among patients with acute coronary syndromes. JAMA 2006;295:1912-20. [PubMed]
- Roe MT, Peterson ED, Newby LK, et al. The influence of risk status on guideline adherence for patients with non-ST-segment elevation acute coronary syndromes. Am Heart J 2006;151:1205-13. [PubMed]
- Tricoci P, Peterson ED, Roe MT, et al. Patterns of guideline adherence and care delivery for patients with unstable angina and non-ST-segment elevation myocardial infarction (from the CRUSADE Quality Improvement Initiative). Am J Cardiol 2006;98:30Q-35Q. [PubMed]
- Tu JV, Khalid L, Donovan LR, et al. Indicators of quality of care for patients with acute myocardial infarction. CMAJ 2008;179:909-15. [PubMed]
- Milani RV, Lavie CJ, Dornelles AC. The impact of achieving perfect care in acute coronary syndrome: the role of computer assisted decision support. Am Heart J 2012;164:29-34. [PubMed]
- Spertus JA, Radford MJ, Every NR, et al. Challenges and opportunities in quantifying the quality of care for acute myocardial infarction: summary from the Acute Myocardial Infarction Working Group of the American Heart Association/American College of Cardiology First Scientific Forum on Quality of Care and Outcomes Research in Cardiovascular Disease and Stroke. Circulation 2003;107:1681-91. [PubMed]