Very large left atrial myxoma: an unusual differential diagnosis of bronchial hyper-reactivity
Introduction
Intra- and paracardiac tumors are rare (incidence in autopsies ca. 0.06%), whereas secondary manifestations of extracardiac masses are more frequent (incidence in autopsies ca. 1.2%) (1). With the exception of paraganglioma, clinical symptoms are typically secondary to mechanical effects of the mass (2).
Case report
A 53-year-old female (body mass index 21.3, body surface area 1.63 m2) had been suffering from occasional dyspnea, atypical angina pectoris, and a decrease in performance. Her primary care physician had initiated treatment for suspected recurrent lower airway infections. This suspicion was supported by a positive methacholine challenge, which was ordered by the consulting pulmonologist and suggested bronchial hyper-reactivity. Subsequently a chest X-ray showed left-atrial enlargment and a questionable mass (Figure 1A). This was confirmed by an echocardiogram ordered by the consulting cardiologist demonstrating a large tumor filling almost the entire left atrium. The mass intermittently prolapsed through the mitral valve orifice. The following transesophageal echocardiography confirmed a combined mitral valve defect (medium transvalvular gradient 11 mmHg and an excentric regurgitation °II. The latter also identified the tumors origin from the interatrial septum (Figure 1B). The added cardiovascular magnetic resonance (CMR) demonstrated a well vascularized mass measuring 67 mm × 46 mm suggesting a myxoma in its typical location (Figure 1C). Finally, pre-operatively performed invasive coronary angiography excluded coronary artery disease and confirmed the tumor by its vascular ‘blush’ supplied by the proximal and distal circumflex coronary artery (Figure 1D). Hemodynamic measurements demonstrated a significantly increased v-wave (48 mmHg) supporting the imaging findings of significant mitral stenosis (Figure E).
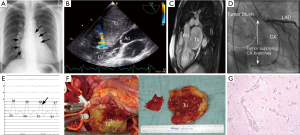
Because of the risk of intermittent mitral valve obstruction, and thrombembolism (3), the mass was resected within two days (Figure 1F) and histologically classified as myxoma (Figure 1G). Ten days after cardiac surgery the patient suffered from third-degree atrioventricular block requiring pacemaker implantation.
Conclusions
Even a very large left-atrial tumor causing intermittent, partial obstruction of the mitral valve, may initially present with mild unspecific symptoms. Delayed diagnosis may increase the risk of complications, including frequently associated thromboembolism.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Lam KY, Dickens P, Chan AC. Tumors of the heart. A 20-year experience with a review of 12,485 consecutive autopsies. Arch Pathol Lab Med 1993;117:1027-31. [PubMed]
- Lamba G, Frishman WH. Cardiac and pericardial tumors. Cardiol Rev 2012;20:237-52. [PubMed]
- Engberding R, Daniel WG, Erbel R, et al. Diagnosis of heart tumours by transoesophageal echocardiography: a multicentre study in 154 patients. European Cooperative Study Group. Eur Heart J 1993;14:1223-8. [PubMed]


