A case of acute aortic insufficiency due to severe rheumatoid arthritis, showing progression in two weeks
Introduction
Rheumatoid arthritis is well known as an important risk factor for heart valve disease, but we experienced a rare case of aortic insufficiency that was detected in the very acute phase.
Case report
A 74-year-old woman with a history of myocardial infarction and severe rheumatoid arthritis on immunosuppressants (5 mg prednisolone, 100 mg mizoribine, and 80 mg tocilizumab) was referred to our hospital because of nausea and tooth pain. Her blood test, electrocardiogram, and chest radiogram showed no abnormalities. The echocardiogram showed an akinetic left ventricular anterior wall, which was thought to be the result of an old myocardial infarction, and normally functioning valves.
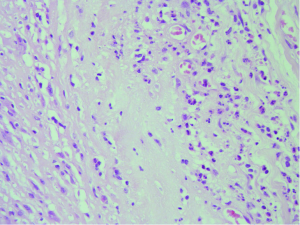
Two weeks after the first assessment, she was referred to our hospital again because of tooth pain and dyspnea. Her blood test results showed a white blood cell count of 4,600/m3, C-reactive protein level of 0.02 mg/dL, procalcitonin level of <0.05 ng/mL, and brain natriuretic peptide level of 294 pg/mL. Her chest radiograph showed congestive heart failure, and the echocardiogram showed severe aortic insufficiency, which was not identified in the previous examination (Figures 1,2). She was diagnosed with congestive heart failure caused by acute aortic insufficiency and was put on diuretics and inotropic agents. She continued therapy with 5 mg prednisolone and 100 mg mizoribine and discontinued therapy with the monoclonal antibody agent 80 mg tocilizumab, which causes poor wound healing. Ten days after the therapy, the patient underwent an aortic valve replacement with a bioprosthetic valve. All three aortic valve leaflets were severely shrunken and thickened, with no coaptation (Figure 3). There was no evidence of infective endocarditis in the aortic valve leaflets, such as perforation, avulsion, or vegetation. On pathological examination of the valve leaflets, fibrosis and inflammatory changes with infiltration of inflammatory cells were observed (Figure 4). There were no specific changes in the pathology of the aortic wall other than atherosclerosis, and we did not find any granulomatous changes (1,2).
She was discharged on postoperative day 16 without any complications.
Discussion
Rheumatoid arthritis is known to be one of the causes of heart valve destruction, leading to both valve stenosis and valve insufficiency (3). There are several case reports on aortic insufficiency caused by rheumatoid arthritis (4-6), but in almost all cases, aortic insufficiency progressed chronically, not acutely.
In this case, it was difficult to confirm the relationship between rheumatoid arthritis activity and acute aortic insufficiency because three kinds of immunosuppressants were prescribed that might suppress the anti-inflammatory response. The C-reactive protein, white blood cell count, and antinuclear antibody values were normal throughout her hospital stay, and her joint pain was controlled. Therefore, we could not use a clinical scoring system such as the 28-joint disease activity score (DAS28) or health assessment questionnaire (HAQ) to evaluate the severity of the rheumatoid arthritis. However, the thickening and shrunken heart valve was one of the well-known features of this disease and she had no other evidence which induced valve was a well-known feature of this disease, and she had no evidence of other factors that would induce valve malfunction; therefore, we considered this condition to be acute aortic insufficiency induced by rheumatoid arthritis.
With regard to acute aortic insufficiency, Aziz et al. (7) reported a case that showed disease progression within 1 month and Mannaerts et al. (8) reported a case that showed disease progression within 2 years. We report here a rare case in which inflammation of the cardiac valves progressed to the acute phase within just 2 weeks, appearing as valvular shrinkage, which induced acute aortic insufficiency. In general, inflammatory changes occurring in collagen diseases show chronic progression, but not in our case. We need to be aware of the possibility of acute aortic insufficiency induced by rheumatoid arthritis.
Conclusions
We report a case of acute aortic insufficiency induced by severe rheumatoid arthritis. We need to recognize rheumatoid arthritis as one of the important risk factors for acute heart valve deterioration.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Shingaki M, Kobayashi Y, Suzuki H. A case of acute aortic insufficiency due to severe rheumatoid arthritis, showing progression in two weeks. Asvide 2014;1:239.
- Shingaki M, Kobayashi Y, Suzuki H. A case of acute aortic insufficiency due to severe rheumatoid arthritis, showing progression in two weeks. Asvide 2014;1:240.
- Corrao S, Messina S, Pistone G, et al. Heart involvement in rheumatoid arthritis: systematic review and meta-analysis. Int J Cardiol 2013;167:2031-8. [PubMed]
- Roldan CA, DeLong C, Qualls CR, et al. Characterization of valvular heart disease in rheumatoid arthritis by transesophageal echocardiography and clinical correlates. Am J Cardiol 2007;100:496-502. [PubMed]
- Uusimaa P, Krogerus ML, Airaksinen J, et al. Aortic valve insufficiency in patients with chronic rheumatic diseases. Clin Rheumatol 2006;25:309-13. [PubMed]
- Minematsu N, Yoshikai M, Kamohara K, et al. Aortic valve regurgitation associated with rheumatoid arthritis; report of a case. Kyobu Geka 2004;57:391-4. [PubMed]
- Aziz S, Sohail M, Murphy G. Acute aortic regurgitation due to necrotizing granulomatous inflammation of the aortic valve in a patient with rheumatoid arthritis. Circulation 2012;126:e106-7. [PubMed]
- Mannaerts HF, May JF, Vierboom MA, et al. Rapidly progressive aortic insufficiency in a female patient with rheumatoid arthritis. Ned Tijdschr Geneeskd 1994;138:618-21. [PubMed]





