Traumatic right atrial pseudoaneurysm
Case report
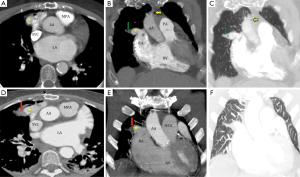
A previously healthy 75-year-old unrestrained motor vehicle driver was brought to the Emergency Department following a motor vehicle accident with complains of chest, back and hip pain. On examination, multiple areas of superficial bruising and local tenderness on right chest and lower spine were noted. The respiratory and cardiac examination was unremarkable. Laboratory results revealed mildly elevated Troponin T and creatine kinase MB (CKMB) while electrocardiogram (ECG) showed sinus tachycardia without ST/T wave changes. An urgent bedside echocardiogram was also done for this patient along with Focussed Assessment Sonography for Trauma (FAST) due to mild elevation of cardiac enzymes. The echocardiogram was unremarkable with no wall motion abnormality or abnormal wall echogenicity. Given the suspicion of lung and cardiac injury, ECG-gated contrast enhanced computed tomography (CECT) was done. The CECT (Figure 1A-C) of chest revealed a focal contrast filled out pouching from the free wall of the right atrium (RA) (star, Figure 1A,B) consistent with pseudoaneurysm with adjacent right lung contusion (green arrow, Figure 1B,C). Additionally, tiny pneumomediastinum (orange arrow, Figure 1B,C), multiple rib, spine and pelvic fractures (not shown) were seen. In the absence of active contrast extravasation from the pseudoaneurysm and with other bony injuries that required immediate attention, patient was conservatively managed with respect to the standpoint of cardiac pseudoaneurysm. Early interval follow up was obtained by ECG-gated CECT (Figure 1D-F, Figure 2) (1) on day 2 that revealed partial peripheral thrombosis (Figure 1D-F) of the right atrial pseudoaneurysm (star, Figure 1D,E). 3D volume-rendered reconstructed computed tomography (CT) image (Figures 3,4) (2) provided excellent demonstration of the relationship of partially thrombosed (red arrow, Figure 1F) pseudoaneurysm (star, Figure 1F) with adjacent structures.



Discussion
Right atrial pseudoaneurysm is an extremely rare manifestation of blunt injury to the chest. In patients with blunt injury to chest, there may be injury to cardiac chambers in approximately 0.3-0.5% of cases (3). Amongst the cardiac chambers, right atrium is involved in approximately 40% of patients with blunt cardiac injury, due to its thin wall and anterior location (4). Fortunately, the atrial rupture is less devastating as compared to typical fatal course of ventricular rupture. Unlike patients with left ventricular (LV) pseudoaneurysm that may have diffuse ST segment elevation in 20% cases, ECG is non-contributory in patients with atrial pseudoaneurysm (5). Electrocardiography (ECG)-gated MDCT is an extremely useful imaging tool for evaluating the cardiac chambers post trauma especially since transthoracic echocardiogram may be unrevealing. Transthoracic echocardiogram could not identify the pseudoaneurysm in our case due to its location. In addition to morphological information, CT images can also be post-processed to evaluate hemodynamic parameters like dynamic pressure and wall shear stress within vascular structures by using computational fluid dynamics technique (6). These hemodynamic parameters can guide further treatment in these patients.
Depending on the hemodynamic status, initially either surgical repair or conservative management may be performed in these patients but eventually surgical repair is required in most patients. Based on Laplace law [Wall stress = (pressure/2) × (radius/wall thickness)], the blood pressure control is the most important conservative strategy for pseudoaneurysm management to decrease the chances of rupture (7,8). Permissive hypotension with goal mean arterial pressure (MAP) of 50 mm Hg has shown promise in patients that are in hemorrhagic shock or at high risk of bleeding (9). Conservative management with permissive hypotension (goal mean arterial pressure: 50 mmHg) was done in our case due to pseudoaneurysm and other fractures that required immediate intervention.
Although the imaging of pseudoaneurysm in body has been extensively described in literature, the uncommon location of the pseudoaneurysm from right atrium and demonstration of rapid partial thrombosis on conservative management makes our case extremely rare. The case also highlights the role of ECG-gating in post-traumatic patients with high suspicion of cardiac/proximal aortic injury.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Nagpal P, Saboo SS, Khandelwal A, et al. Axial contrast enhanced ECG-gated CT images obtained two days after the presentation showing persistent right atrial pseudoaneurysm (arrow) with thrombus in its periphery. Asvide 2015;2:018. Available online: http://www.asvide.com/articles/472
- Nagpal P, Saboo SS, Khandelwal A, et al. 3D-Volume rendered images showing relationship of the pseudoaneurysm (arrow) and the thrombus with the adjacent cardiovascular structures. Asvide 2015;2:019. Available online: http://www.asvide.com/articles/473
- Martin TD, Flynn TC, Rowlands BJ, et al. Blunt cardiac rupture. J Trauma 1984;24:287-90. [PubMed]
- Brathwaite CE, Rodriguez A, Turney SZ, et al. Blunt traumatic cardiac rupture. A 5-year experience. Ann Surg 1990;212:701-4. [PubMed]
- Frances C, Romero A, Grady D. Left ventricular pseudoaneurysm. J Am Coll Cardiol 1998;32:557-61. [PubMed]
- Karmonik C, Partovi S, Schmack B, et al. Comparison of hemodynamics in the ascending aorta between pulsatile and continuous flow left ventricular assist devices using computational fluid dynamics based on computed tomography images. Artif Organs 2014;38:142-8. [PubMed]
- Restrepo CS, Gutierrez FR, Marmol-Velez JA, et al. Imaging patients with cardiac trauma. Radiographics 2012;32:633-49. [PubMed]
- Hulten EA, Blankstein R. Pseudoaneurysms of the heart. Circulation 2012;125:1920-5. [PubMed]
- Morrison CA, Carrick MM, Norman MA, et al. Hypotensive resuscitation strategy reduces transfusion requirements and severe postoperative coagulopathy in trauma patients with hemorrhagic shock: preliminary results of a randomized controlled trial. J Trauma 2011;70:652-63. [PubMed]


