
Epicardial and thoracic fat - Noninvasive measurement and clinical implications
Introduction
It has been shown in the past two decades that regional visceral fat distribution may contribute to an unfavorable metabolic and cardiovascular risk profile (1). Epicardial fat, the local visceral fat depot enclosed by the visceral pericardial sac, surrounds the coronary arteries for most of their course. It has been postulated that epicardial fat may contribute to the development of coronary atherosclerosis through local production of inflammatory cytokines (2,3). In recent years, several studies which measured epicardial fat volume noninvasively have shown a relationship of increased epicardial fat volume with coronary artery disease, with the presence and progression of coronary plaque burden as measured by the coronary calcium score (4-8), adverse cardiovascular events (9-11), myocardial ischemia (12,13) and atrial fibrillation (14,15). In these studies, epicardial fat volume remained significantly associated with coronary and non-coronary heart disease even after adjusting for obesity measures (weight or body mass index) and traditional cardiovascular risk factors. This review summarizes the current methods for noninvasive measurement of epicardial fat, the clinical implications of increased epicardial fat, and discusses simple methods of its reduction such as weight loss.
Noninvasive measurement of epicardial and thoracic fat
Definition
Epicardial fat is the fat depot around the heart and enclosed by the visceral pericardium. It has been previously described in the literature as “pericardial” and “paracardial” fat. Extra-pericardial thoracic fat, outside the visceral pericardium, has also been described as intra-thoracic fat. Thoracic fat (fat within the inner thoracic cavity) therefore includes both epicardial and extra-pericardial fat, and correlates strongly with epicardial fat (typically R >0.85) (5).
Measurement from CT
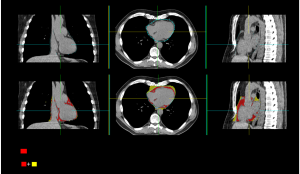
Due to distinct attenuation values of fat on CT, fat around the heart is readily identified by chest or cardiac CT, both with and without contrast. ECG-gated cardiac CT for both coronary calcium scoring and coronary CT angiography, with its attendant high spatial resolution, allows accurate measurement of epicardial and thoracic fat distances and volumes. Volumetric quantification of epicardial fat and thoracic fat require the following processing steps: identification of the limits of the heart, and tracing of the inner thoracic cavity and pericardium, which can be manual (4,6) or semi-automated (5). The superior heart limit slice is typically chosen at the split of the pulmonary artery. The anatomic landmark for the inferior limit of the heart is typically the most inferior slice of the myocardium (9) or the most inferior slice with the posterior descending artery (12). With our semi-automated measurement, pericardial fat contours are generated by spline interpolation through several control points which are placed manually on the visceral pericardium (5), and the inner thoracic cavity is segmented automatically (16). The typical processing time for the semi-automated method is 7-10 minutes (5); however, preliminary fully automated algorithms have been reported by our group for segmentation of the heart and pericardium in CT scans, which show promising results when compared with an expert reader (17). Standard fat attenuation values are used to define fat attenuation by CT; for non-contrast CT typically an attenuation range of (–30, –190) Hounsfield Units is used. Fat voxels within this attenuation range within the visceral pericardium are classified as epicardial fat, and within the inner thoracic cavity classified as thoracic fat (Figure 1). We have shown that interscan reproducibility for the semi-automated method for measurement of epicardial and thoracic fat is high, with correlation coefficients ≥0.98 for the same multidetector CT scanner (18).
Measurement from Ultrasound and Magnetic Resonance Imaging (MRI)
With transthoracic echocardiography, epicardial adipose tissue thickness can be measured (19) and has been used in clinical studies (20-23). Subjects are positioned in the left lateral decubitus position and the echocardiograms are recorded during several cardiac cycles. The epicardial adipose tissue is visible as an echo free space. Since the right ventricle is accessible from both parasternal long- and short axis views and contains the highest adipose tissue thickness, measurements of epicardial adipose tissue are typically made on the free wall of the right ventricle. While low intra- and inter-observer correlations [0.63 (95% CI, 0.40-0.77) and 0.61 (95% CI, 0.37-0.75), respectively] have been reported in one study (24), another study indicated good reproducibility with a coefficient of variation between two sonographers of 3% (19). Of note, epicardial fat is prominent near the interventricular and the atrioventricular grooves. The greatest amount of epicardial fat can be found at the lateral right ventricular wall, followed by the anterior wall (25,26). Moreover, the distribution of epicardial fat seems to show considerable individual differences. Therefore, it is unclear whether thickness of right ventricular epicardial fat measured at a single point correlates well with the volumetric amount of epicardial fat. The two-dimensional echocardiographic approach has the limitation of not being truly volumetric. A few recent studies have used cardiac MRI as a tool to measure epicardial adipose tissue (15,27). Similar to CT, with MRI the contours of the epicardial adipose tissue are traced on short axis slices and adipose tissue voxels are added to calculate epicardial adipose tissue volume. There is a high correlation between epicardial adipose tissue on echocardiography and cardiovascular magnetic resonance imaging (CMR) (20). Furthermore, inter-observer variability and reproducibility with MRI are higher for the volumetric approach compared to measurement of the epicardial adipose tissue thickness (28).
Measure distance or volume?
Measurements of volumetric and distance of epicardial fat have been compared in 45 patients who underwent CT imaging and invasive coronary angiography (29). Volumetric measurement showed higher reproducibility and inter-observer agreement (correlation coefficient 0.96) compared to distance measurements (0.58 for average epicardial fat thickness). Patients with significant coronary artery stenosis had significantly greater epicardial fat volumes (154.58±58.91 cm3) than those without significant arterial stenosis (120.94±81.85 cm3, P=0.016); while epicardial fat distance failed to show a significant difference between the two patient groups.
Clinical implications of measured epicardial and thoracic fat
Relationship with coronary atherosclerosis and its progression
It has been hypothesized that paracrine effects of the epicardial and pericoronary adipose tissue (fat directly surrounding the coronary arteries) may be potent determinants of coronary plaque development and progression; and this has been demonstrated by several studies whose findings can be classified into two main groups. First, adipose tissue directly surrounding the coronary arteries has been found to contain higher levels of inflammatory markers than subcutaneous fat. Second, increased epicardial and pericoronary adipose tissue has been found to be associated with several measures of coronary atherosclerosis (both luminal stenosis and plaque). Mazurek et al. elegantly showed in 42 patients undergoing elective bypass surgery that adipose tissue adjacent to the right coronary artery contained significantly higher expression of interleukin-1β, interleukin-6, monocyte chemotactic protein, and tumor necrosis factor, and retained a greater number of inflammatory cells that subcutaneous adipose tissue; irrespective of clinical risk factors or plasma concentrations of circulating biomarkers (3). Similar findings have been substantiated in subsequent studies (30-32). A three-dimensional ultrasound study has demonstrated that eccentric atherosclerotic plaques develop with a spatial orientation suggestive of a relationship with epicardial fat (33). Further, autopsy evidence has shown that coronary arteries with large necrotic cores have more macrophages in the periadventitial fat than in vessels without a lipid core (34). A recent study examined epicardial fat measured by MRI in relation to coronary microavscular response in young healthy subjects, and found that a high epicardial fat volume is associated with a lower coronary microvascular response, suggesting that epicardial fat could early influence endothelial function (27).
Multiple studies have implicated the role of epicardial fat quantified by cardiac CT in the pathophysiology of coronary atherosclerosis. Table 1 lists the studies from prospective registries of asymptomatic patients who underwent coronary calcium scoring, which demonstrate that epicardial or thoracic fat volume are independently associated with the presence of coronary calcium (4-6). From 1,155 participants in the Framingham Heart Study, Rosito et al. found that epicardial and thoracic fat are associated with vascular calcification (coronary and abdominal aortic calcification respectively), after multivariable adjustment of traditional risk factors and visceral abdominal fat, suggesting that these fat depots may exert local toxic effects on the vasculature (4). From 201 participants in the Early Identification of Subclinical Atherosclerosis by Noninvasive Imaging Research (EISNER) registry, we found that epicardial and thoracic fat volume were associated with the presence of coronary calcium (5). Gorter et al. examined CT-measured epicardial fat volume in relation with diagnostic invasive coronary angiography (35) and observed that for patient’s body mass index (BMI) <27 kg/m2, epicardial fat volume was related to the severity of coronary artery disease and also to the degree of coronary artery calcium. In patients who underwent coronary CT angiography, Kim et al. observed that CT-measured epicardial fat volume was related to the presence of significant coronary stenosis (>50%) (36). In patients who underwent coronary calcium scoring, Ahmadi et al. found that CT-measured epicardial fat volume was higher for both males and females with higher CCS (37). In 171 patients referred for coronary CT angiography, Konishi et al. found that epicardial fat volume was significantly associated with the presence of nonstenotic and noncalcified coronary plaques, after adjusting for measures of abdominal obesity; their results suggested that epicardial fat is more strongly associated with early development of coronary artery disease than measures of abdominal obesity (38). Alexopoulous et al. observed on coronary CT angiography a significant increase in epicardial fat volume with increasing coronary luminal stenosis; epicardial fat volume was also larger in patients with mixed or noncalcified plaques (39). Greif et al. have shown that increased thoracic fat volumes are associated with coronary atherosclerosis, inflammation and low adiponectin (40). In 78 patients referred for coronary CT angiography, Mahabadi et al. demonstrated that pericoronary fat is independently associated with the presence of coronary plaque, irrespective of plaque type (noncalcified or calcified, P<0.01 for all).
Table 1
| n | Fat measure from CT | Outcome measure | Odds ratio for presence of coronary calcium | |
|---|---|---|---|---|
| Framingham (4) | 1,155 | Epicardial fat volume | CCS > 0 | OR 1.27 (95% CI, 1.06-1.52) |
| EISNER (5) | 201 | Epicardial fat volume | CCS > 0 | OR 2.4 (95% CI, 1.2-4.8) |
| MESA (6) | 159 | Thoracic fat volume slab (4.5 cm-thick about Left Main Origin) | CCS > 0 | OR 2.24 (95% CI, 1.38-3.64) |
CCS: Agatston Coronary Calcium Score; EISNER: Early Identification of Subclinical Atherosclerosis by Noninvasive Imaging Research; MESA: Multi-Ethnic Study of Atherosclerosis
Increased epicardial fat volume has recently also been linked to high-risk plaques as assessed by coronary CT angiography. In 357 patients undergoing coronary CT angiography, Oka et al. recently found that epicardial fat volume is an independent predictor of low-density noncalcified plaque with positive remodeling, after adjusting for risk factors, BMI, visceral fat and coronary calcium (41). Further, a recent study by Schlett et al. found that in 358 patients admitted to the emergency department with acute chest pain and undergoing coronary CT angiography, epicardial fat volume was significantly elevated in 13 patients with high-risk coronary lesions (characterized by >50% luminal stenosis and at least 2 of the following adverse plaque characteristics: positive remodeling, low-density plaque and spotty calcification) (42); in multivariable analysis, this association persisted independent of traditional risk factors and BMI.
Recent studies have also shown that increased epicardial fat volume is an independent predictor of progression of subclinical coronary atherosclerosis in asymptomatic subjects. In 333 asymptomatic diabetic subjects without prior history of coronary artery disease, who underwent coronary calcium scoring and a repeat scan after 2.7±0.3 years, CT-measured epicardial fat volume was an independent marker for the presence and severity of coronary calcium burden and also identified individuals at increased risk of coronary calcium progression (7). We have recently shown from the EISNER study that increase in epicardial fat volume is associated with greater progression of coronary calcium over 3-5 years in asymptomatic subjects with intermediate cardiovascular risk (8).
Prediction of adverse cardiovascular outcomes
Epicardial fat has also been linked to the development of major adverse cardiovascular events (MACE). Table 2 shows studies from prospective registries of asymptomatic patients who underwent coronary calcium scoring, which demonstrate that epicardial or thoracic fat volume are independent predictors of MACE. Mahabadi et al. studied the relationship between epicardial, thoracic and visceral fat measured from non-contrast CT with subsequent participants of the Framingham Heart Study (10). In this study, after adjustment for standard clinical measures and BMI and waist circumference, epicardial fat was more strongly associated with subsequent events than abdominal visceral fat. Interestingly, epicardial fat was predominantly associated with MACE, whereas only abdominal visceral fat was associated with stroke. These findings suggest the two fat beds may impact atherogenesis differently, with abdominal visceral fat exerting a more systematic effect and epicardial fat a more local paracrine effect. In a matched case-control study from the EISNER registry, we found that asymptomatic patients who experienced MACE had greater epicardial fat volume when compared with event-free subjects; and the addition of epicardial fat volume to conventional clinical risk stratification and coronary calcium score improved prediction of MACE (9). Interestingly, in the studies reported by Cheng et al. and Mahabadi et al., extra-pericardial thoracic fat volume did not show significant relationship to MACE or cardiovascular disease burden (9,10), further augmenting the hypothesis that epicardial fat exerts a local pathogenic effect on the coronary arteries. Further, two studies have investigated the relationship of epicardial fat volume to inducible myocardial ischemia by SPECT and PET and found that increased epicardial fat volume was strongly associated with ischemia (12,13). Interestingly, Tamarappoo et al. also found that addition of extra-pericardial thoracic fat, which is further away from the coronary arteries, did not add to epicardial fat volume in the prediction of ischemia (non-significant increase in the area-under Receiver-Operator Characteristic curve) (12). In 92 consecutive patients without known coronary artery disease who underwent PET, coronary calcium scoring and invasive coronary angiography within 6 months, we showed that epicardial fat volume measured from CT significantly predicted the presence of both ischemia and significant stenosis (43). Epicardial fat volume has been shown to be reduced in patients with congestive heart failure in comparison with stable controls (44). Khawaja et al. recently examined the role of epicardial fat volume measured from low-dose CT in 381 consecutive patients undergoing assessment of cardiac function with echocardiography (45). They observed that epicardial fat volume decreased persistently with impaired cardiac function, decreasing stepwise in patients with normal ejection fraction (no history of heart failure or left ventricular dysfunction), moderate left ventricular dysfunction (ejection fraction 35-55%) and severe left ventricular dysfunction (ejection fraction <35%). Interestingly, no relation was found between epicardial fat volume and coronary calcium in this patient population. The decrease in epicardial fat with impaired cardiac function and congestive heart failure imply a complex interaction of regulatory pathways between epicardial fat and the dysfunctional myocardium; suggesting that in advanced heart failure, as the myocardium alters in structure and function, and develops abnormal metabolic needs, the role of epicardial fat as a source of cytokine homeostasis may decrease (45).
Table 2
| N | Outcome variable | Fat measure from CT | Odds ratio (95% CI) |
|---|---|---|---|
| Framingham (8)*, 1,267 patients | Coronary Heart Disease (Myocardial infarction, angina, coronary insufficiency) | Epicardial fat volume | 1.92 (1.23-3.02), over visceral fat |
| Myocardial infarction | Epicardial fat volume | 1.37 (1.03-1.82), over visceral fat | |
| Stroke | Visceral fat | 1.83 (1.01-3.30), EFV not significant | |
| EISNER (7)*, Matched study 232 patients (from registry of 2,751 patients) | MACE (Cardiac death, myocardial infarction, stroke, late revascularization) | Epicardial fat volume | 1.74 (1.03-2.95), over Framingham Risk Score and CCS |
| Thoracic fat volume | 1.78 (1.01-3.14), over Framingham Risk Score and CCS | ||
| MESA (9), Matched study 998 patients (from registry of 6,814 patients) | Coronary Heart Disease (Cardiac death, myocardial infarction, resuscitated cardiac arrest, angina) | Thoracic fat volume slab (4.5 cm-thick about Left Main Origin). Adjusted for gender, risk factors and CRP |
OR 1.26 (1.01-1.59), over BMI and waist circumference |
*: Extra-pericardial thoracic fat volume did not show significant relationship to adverse cardiovascular outcomes, suggesting a local effect.
Relationship with non-atherosclerotic heart disease
Studies have shown association of epicardial fat with non-atherosclerotic heart disease, including association with atrial fibrillation (14,15,46). In a study of 273 patients, Al Chekakie et al. showed that patients with paroxysmal atrial fibrillation had significantly larger epicardial fat volume than those in sinus rhythm; epicardial fat volume was associated with paroxysmal and persistent atrial fibrillation, independent of age, gender, hypertension, left atrial enlargement, valvular heart disease, left ventricular ejection fraction, diabetes mellitus, and BMI. Wong et al. recently showed that epicardial fat volume is associated with the presence and severity of atrial fibrillation, left atrial volumes and poorer outcomes after atrial fibrillation ablation, independent of systematic measures of adiposity (15). Further, in a study of 169 consecutive patients undergoing coronary CT angiography, Batal et al. found that posterior left atrial epicardial fat pad thickness measured between the left atrium and esophagus was significantly associated with atrial fibrillation burden, and this relationship persisted independent of age, BMI or left atrial area (47).
Normal upper threshold for epicardial and thoracic fat
For cohort studies, it would be useful to know the upper threshold above which epicardial fat volume can be considered “abnormal” or “high”. While data regarding this is still limited, a few studies have attempted to establish an upper threshold for epicardial fat volume. From 3,312 participants of the community-based Framingham Heart Study, high epicardial fat volumes were defined by the 90th percentile in a healthy sample to be 139.4 cm3 for men and 119.0 cm3 for women (48). From our prognostic study from the EISNER registry, upper cutoff values for epicardial fat volume was determined to be 125.0 cm3 from patients free of MACE events (9). In a recent publication, we have further derived a upper normal threshold from a low-risk healthy population from the EISNER registry (226 healthy asymptomatic non-diabetic nonsmokers, with a low Framingham Risk Score, no known cardiovascular disease, a coronary calcium score of 0, and low risk factors) (49). From this new cohort of healthy subjects, the upper threshold was also determined to be 125 cm3 and was not significantly affected by age or gender. When indexed to Body Surface Area (BSA), the BSA-indexed upper threshold of epicardial fat volume corresponded to 68.1 cm3/m2; this value was further validated by our prognostic data in (9) to show that indexed epicardial fat volume values greater than this upper threshold significantly predicted MACE after adjusting for confounders (Odds Ratio 2.8, 95% confidence interval 1.3-6.4, P=0.012) (49).
Reduction of epicardial fat
The scientific evidence to date indicates that increased epicardial fat is associated with coronary atherosclerosis and adverse cardiovascular outcomes. One important question is that can this visceral fat depot be reduced? While this is a subject of ongoing research, preliminary studies have indicated that substantial weight loss in severely obese patients following bariatric surgery or marked calorie intake reduction may be accompanied by a corresponding decrease in epicardial fat volume (50,51). Two prior studies using transthoracic echocardiography provided initial evidence that marked weight loss may reduce epicardial fat burden. Iacobellis et al. showed a decrease in epicardial fat thickness in obese subjects who underwent an aggressive 6-month long weight loss program (mean 20 kg) by adhering to a very low-calorie diet (900 kcal/day) (50). Similarly, in severely obese patients, Willens et al. reported that weight loss after bariatric surgery (average weight loss of 40 kg) was associated with a decrease in epicardial adipose tissue thickness (51). While this observation suggests that epicardial fat volume may be modifiable, it is unknown whether weight fluctuations have a similar effect in subjects who are not enrolled in an intensive weight-loss program. In a recent study, we assessed the relationship of epicardial fat volume to weight, BMI and waist circumference, and evaluated whether changes in these parameters over a four-year period influence epicardial fat volume measured by non-contrast CT in a relatively healthy asymptomatic population (52). In 374 asymptomatic patients undergoing 2 coronary calcium scoring scans at a mean interval of 4.1 years, we found that weight, BMI and waist circumference demonstrated moderate cross-sectional relationships to epicardial fat volume, and that changes in these parameters were related to epicardial fat volume change. Our study indicated that reduction in total body weight (>5%) is associated with stabilization or reduction in epicardial fat burden, whereas weight gain is associated with greater epicardial fat progression. Importantly, whereas the prior studies of Iacobellis et al. and Willens et al. found reduction in epicardial fat volume associated with major weight loss, our study showed that epicardial fat volume decrease can also accompany relatively minor weight reduction (<5% change in body weight). We also observed that hypertension was an independent predictor of epicardial fat volume change. It may be that in future larger studies, hypertension could emerge as a predictor of increase in epicardial fat volume.
Summary
In summary, epicardial fat is independently associated with coronary atherosclerosis, adverse cardiovascular events, myocardial ischemia and non-coronary heart disease. Although epicardial fat volume correlates with abdominal visceral fat, results of several studies suggest that the two fat beds may impact atherogenesis differently, with abdominal visceral fat exerting a more systemic effect in promoting insulin resistance and epicardial fat a local pathogenic effect on the coronary arteries and on the heart. While the exact mechanisms are yet not fully understood, the evidence to date suggests that the inflammatory properties of epicardial fat depot may play an important role in cardiovascular disease. Quantitative measurement of epicardial fat volume from noninvasive imaging modalities such as CT and MRI are feasible, and may play a clinical role in cardiovascular risk assessment. The intriguing scientific evidence to date warrants larger and longitudinal cohort studies to further investigate the role of epicardial fat as an imaging marker with prognostic importance.
Acknowledgements
Disclosure: The authors declare no conflict of interest relative to this work.
References
- Iacobellis G, Pistilli D, Gucciardo M, et al. Adiponectin expression in human epicardial adipose tissue in vivo is lower in patients with coronary artery disease. Cytokine 2005;29:251-5. [PubMed]
- Iacobellis G, Corradi D, Sharma AM. Epicardial adipose tissue: anatomic, biomolecular and clinical relationships with the heart. Nat Clin Pract Cardiovasc Med 2005;2:536-43. [PubMed]
- Mazurek T, Zhang L, Zalewski A, et al. Human epicardial adipose tissue is a source of inflammatory mediators. Circulation 2003;108:2460-6. [PubMed]
- Rosito GA, Massaro JM, Hoffmann U, et al. Pericardial fat, visceral abdominal fat, cardiovascular disease risk factors, and vascular calcification in a community-based sample: the Framingham Heart Study. Circulation 2008;117:605-13. [PubMed]
- Dey D, Wong ND, Tamarappoo B, et al. Computer-aided non-contrast CT-based quantification of pericardial and thoracic fat and their associations with coronary calcium and Metabolic Syndrome. Atherosclerosis 2010;209:136-41. [PubMed]
- Ding J, Kritchevsky SB, Harris TB, et al. The association of pericardial fat with calcified coronary plaque. Obesity (Silver Spring) 2008;16:1914-9. [PubMed]
- Yerramasu A, Dey D, Venuraju S, et al. Increased volume of epicardial fat is an independent risk factor for accelerated progression of sub-clinical coronary atherosclerosis. Atherosclerosis 2012;220:223-30. [PubMed]
- Nakanishi R, Rajani R, Cheng VY, et al. Increase in epicardial fat volume is associated with greater coronary artery calcification progression in subjects at intermediate risk by coronary calcium score: a serial study using non-contrast cardiac CT. Atherosclerosis 2011;218:363-8. [PubMed]
- Cheng VY, Dey D, Tamarappoo B, et al. Pericardial fat burden on ECG-gated noncontrast CT in asymptomatic patients who subsequently experience adverse cardiovascular events. JACC Cardiovasc Imaging 2010;3:352-60. [PubMed]
- Mahabadi AA, Massaro JM, Rosito GA, et al. Association of pericardial fat, intrathoracic fat, and visceral abdominal fat with cardiovascular disease burden: the Framingham Heart Study. Eur Heart J 2009;30:850-6. [PubMed]
- Ding J, Hsu FC, Harris TB, et al. The association of pericardial fat with incident coronary heart disease: the Multi-Ethnic Study of Atherosclerosis (MESA). Am J Clin Nutr 2009;90:499-504. [PubMed]
- Tamarappoo B, Dey D, Shmilovich H, et al. Increased pericardial fat volume measured from noncontrast CT predicts myocardial ischemia by SPECT. JACC Cardiovasc Imaging 2010;3:1104-12. [PubMed]
- Janik M, Hartlage G, Alexopoulos N, et al. Epicardial adipose tissue volume and coronary artery calcium to predict myocardial ischemia on positron emission tomography-computed tomography studies. J Nucl Cardiol 2010;17:841-7. [PubMed]
- Al Chekakie MO, Welles CC, Metoyer R, et al. Pericardial fat is independently associated with human atrial fibrillation. J Am Coll Cardiol 2010;56:784-8. [PubMed]
- Wong CX, Abed HS, Molaee P, et al. Pericardial fat is associated with atrial fibrillation severity and ablation outcome. J Am Coll Cardiol 2011;57:1745-51. [PubMed]
- Dey D, Suzuki Y, Suzuki S, et al. Automated quantitation of pericardiac fat from noncontrast CT. Invest Radiol 2008;43:145-53. [PubMed]
- Dey D, Ramesh A, Slomka PJ, et al. Automated algorithm for atlas-based segmentation of the heart and pericardium from non-contrast CT. Proc SPIE 2010;7623:762337. [PubMed]
- Nakazato R, Shmilovich H, Tamarappoo BK, et al. Interscan reproducibility of computer-aided epicardial and thoracic fat measurement from noncontrast cardiac CT. J Cardiovasc Comput Tomogr 2011;5:172-9. [PubMed]
- Iacobellis G, Assael F, Ribaudo MC, et al. Epicardial fat from echocardiography: a new method for visceral adipose tissue prediction. Obes Res 2003;11:304-10. [PubMed]
- Iacobellis G, Ribaudo MC, Assael F, et al. Echocardiographic epicardial adipose tissue is related to anthropometric and clinical parameters of metabolic syndrome: a new indicator of cardiovascular risk. J Clin Endocrinol Metab 2003;88:5163-8. [PubMed]
- Ahn SG, Lim HS, Joe DY, et al. Relationship of epicardial adipose tissue by echocardiography to coronary artery disease. Heart 2008;94:e7. [PubMed]
- Chaowalit N, Somers VK, Pellikka PA, et al. Subepicardial adipose tissue and the presence and severity of coronary artery disease. Atherosclerosis 2006;186:354-9. [PubMed]
- Eroglu S, Sade LE, Yildirir A, et al. Epicardial adipose tissue thickness by echocardiography is a marker for the presence and severity of coronary artery disease. Nutr Metab Cardiovasc Dis 2009;19:211-7. [PubMed]
- Saura D, Oliva MJ, Rodríguez D, et al. Reproducibility of echocardiographic measurements of epicardial fat thickness. Int J Cardiol 2010;141:311-3. [PubMed]
- Tansey DK, Aly Z, Sheppard MN. Fat in the right ventricle of the normal heart. Histopathology 2005;46:98-104. [PubMed]
- Schejbal V. Pneumologie 1989;43:490-9. [Epicardial fatty tissue of the right ventricle--morphology, morphometry and functional significance]. [PubMed]
- Gaborit B, Kober F, Jacquier A, et al. Epicardial Fat Volume Is Associated With Coronary Microvascular Response in Healthy Subjects: A Pilot Study. Obesity (Silver Spring) 2011. [Epub ahead of print].
- Flüchter S, Haghi D, Dinter D, et al. Volumetric assessment of epicardial adipose tissue with cardiovascular magnetic resonance imaging. Obesity (Silver Spring) 2007;15:870-8. [PubMed]
- Bastarrika G, Broncano J, Schoepf UJ, et al. Relationship between coronary artery disease and epicardial adipose tissue quantification at cardiac CT: comparison between automatic volumetric measurement and manual bidimensional estimation. Acad Radiol 2010;17:727-34. [PubMed]
- Baker AR, Silva NF, Quinn DW, et al. Human epicardial adipose tissue expresses a pathogenic profile of adipocytokines in patients with cardiovascular disease. Cardiovasc Diabetol 2006;5:1. [PubMed]
- Yudkin JS, Eringa E, Stehouwer CD. “Vasocrine” signalling from perivascular fat: a mechanism linking insulin resistance to vascular disease. Lancet 2005;365:1817-20. [PubMed]
- Hirata Y, Tabata M, Kurobe H, et al. Coronary atherosclerosis is associated with macrophage polarization in epicardial adipose tissue. J Am Coll Cardiol 2011;58:248-55. [PubMed]
- Prati F, Arbustini E, Labellarte A, et al. Eccentric atherosclerotic plaques with positive remodelling have a pericardial distribution: a permissive role of epicardial fat? A three-dimensional intravascular ultrasound study of left anterior descending artery lesions. Eur Heart J 2003;24:329-36. [PubMed]
- Vela D, Buja LM, Madjid M, et al. The role of periadventitial fat in atherosclerosis. Arch Pathol Lab Med 2007;131:481-7. [PubMed]
- Gorter PM, de Vos AM, van der Graaf Y, et al. Relation of epicardial and pericoronary fat to coronary atherosclerosis and coronary artery calcium in patients undergoing coronary angiography. Am J Cardiol 2008;102:380-5. [PubMed]
- Kim TH, Yu SH, Choi SH, et al. Pericardial fat amount is an independent risk factor of coronary artery stenosis assessed by multidetector-row computed tomography: the Korean Atherosclerosis Study 2. Obesity (Silver Spring) 2011;19:1028-34. [PubMed]
- Ahmadi N, Nabavi V, Yang E, et al. Increased epicardial, pericardial, and subcutaneous adipose tissue is associated with the presence and severity of coronary artery calcium. Acad Radiol 2010;17:1518-24. [PubMed]
- Konishi M, Sugiyama S, Sugamura K, et al. Association of pericardial fat accumulation rather than abdominal obesity with coronary atherosclerotic plaque formation in patients with suspected coronary artery disease. Atherosclerosis 2010;209:573-8. [PubMed]
- Alexopoulos N, McLean DS, Janik M, et al. Epicardial adipose tissue and coronary artery plaque characteristics. Atherosclerosis 2010;210:150-4. [PubMed]
- Greif M, Becker A, von Ziegler F, et al. Pericardial adipose tissue determined by dual source CT is a risk factor for coronary atherosclerosis. Arterioscler Thromb Vasc Biol 2009;29:781-6. [PubMed]
- Oka T, Yamamoto H, Ohashi N, et al. Association between epicardial adipose tissue volume and characteristics of non-calcified plaques assessed by coronary computed tomographic angiography. Int J Cardiol 2012;161:45-9. [PubMed]
- Schlett CL, Ferencik M, Kriegel MF, et al. Association of pericardial fat and coronary high-risk lesions as determined by cardiac CT. Atherosclerosis 2012;222:129-34. [PubMed]
- Nakazato R, Dey D, Cheng VY, et al. Epicardial fat volume and concurrent presence of both myocardial ischemia and obstructive coronary artery disease. Atherosclerosis 2012;221:422-6. [PubMed]
- Doesch C, Haghi D, Flüchter S, et al. Epicardial adipose tissue in patients with heart failure. J Cardiovasc Magn Reson 2010;12:40. [PubMed]
- Khawaja T, Greer C, Chokshi A, et al. Epicardial fat volume in patients with left ventricular systolic dysfunction. Am J Cardiol 2011;108:397-401. [PubMed]
- Thanassoulis G, Massaro JM, O’Donnell CJ, et al. Pericardial fat is associated with prevalent atrial fibrillation: the Framingham Heart Study. Circ Arrhythm Electrophysiol 2010;3:345-50. [PubMed]
- Batal O, Schoenhagen P, Shao M, et al. Left atrial epicardial adiposity and atrial fibrillation. Circ Arrhythm Electrophysiol 2010;3:230-6. [PubMed]
- Thanassoulis G, Massaro JM, Hoffmann U, et al. Prevalence, distribution, and risk factor correlates of high pericardial and intrathoracic fat depots in the Framingham heart study. Circ Cardiovasc Imaging 2010;3:559-66. [PubMed]
- Shmilovich H, Dey D, Cheng VY, et al. Threshold for the upper normal limit of indexed epicardial fat volume: derivation in a healthy population and validation in an outcome-based study. Am J Cardiol 2011;108:1680-5. [PubMed]
- Iacobellis G, Singh N, Wharton S, et al. Substantial changes in epicardial fat thickness after weight loss in severely obese subjects. Obesity (Silver Spring) 2008;16:1693-7. [PubMed]
- Willens HJ, Byers P, Chirinos JA, et al. Effects of weight loss after bariatric surgery on epicardial fat measured using echocardiography. Am J Cardiol 2007;99:1242-5. [PubMed]
- Nakazato R, Rajani R, Cheng VY, et al. Weight change modulates epicardial fat burden: a 4-year serial study with non-contrast computed tomography. Atherosclerosis 2012;220:139-44. [PubMed]


