
Non-invasive functional assessment using computed tomography: when will they be ready for clinical use?
Rapid advances in multi-slice computed tomography (CT) imaging technology have facilitated rapidly increasing use of noninvasive coronary artery imaging, with an estimated annual 2.3 million coronary CT angiography examinations in U.S. alone (1). Currently available cardiac CT scanners have the ability to accurately image the entire coronary tree and provide information regarding the coronary lumen and vessel wall for coronary lesions. The diagnostic accuracy of coronary CT angiography for the identification of coronary artery disease (CAD) has been demonstrated in several studies, including recent multicenter trials (2-4). The consistently high sensitivity (94-99%) and negative predictive value (NPV, 97-99%) in individuals without known CAD highlight the ability of coronary CT angiography to detect and exclude obstructive coronary artery stenosis (2,3). Conversely, comparatively low specificity (64-83%) and positive predictive value (PPV, 48-86%) underscore an excessive rate of false-positive coronary CT angiography findings in which diameter stenosis severity is erroneously overestimated. Considering the role of coronary CT angiography as gatekeeper for invasive coronary angiography, these findings have raised concerns that false positive coronary CT angiography findings may precipitate unnecessary referral for invasive angiography and revascularization, resulting in substantial cost to the patient and healthcare system.
Anatomic and functional assessment
The anatomical assessment of a coronary stenosis as determined by coronary CT angiography correlates poorly with the hemodynamic significance of the stenosis (5). In a prospective study of 78 patients undergoing sequential coronary CT angiography, myocardial perfusion single-photon emission CT (SPECT), and invasive coronary angiography, the sensitivity and NPV for coronary CT angiography to detect any perfusion defect was high (94% for both), although the specificity and PPV were only 64% and 63% respectively (6). In a similar study of 79 patients undergoing coronary CT angiography and invasive angiography with fractional flow reserve (FFR) measurements, the sensitivity of coronary CT angiography by visual estimation to detect lesions with functional significance (FFR <0.75) was high (94%), while the specificity to detect such lesion was poor (40%) (5). Nevertheless, these findings did not reflect a failure of coronary CT angiography to accurately assess coronary artery stenosis, since invasive coronary angiography could not improve the diagnostic accuracy to detect myocardial ischemia (5,6). Rather, a high rate of false-positive results is seen by any method of anatomic evaluation, thus questioning the relevance of coronary stenosis detection by anatomic methods for identification of individuals who may most benefit from revascularization. Eventually, patients with obstructive CAD on coronary CT angiography need to be investigated by a subsequent functional test such as stress echocardiography, stress nuclear myocardial perfusion imaging, or magnetic resonance imaging.
Myocardial perfusion imaging with single-photon emission CT (SPECT) and positron emission tomography (PET) are well accepted and widely used to evaluate the functional significance of a CAD since they demonstrate stress-inducible perfusion defects. In appropriately selected patients, nuclear myocardial perfusion imaging has been shown to be an efficient and cost-effective strategy to avoid the use of unnecessary invasive angiography (7). However, normal myocardial perfusion does not exclude the presence of coronary atherosclerosis (8). In addition, due to limited spatial resolution, SPECT is not capable of detecting transmural differences in myocardial perfusion and has limited diagnostic performance in the setting of multivessel disease with balanced ischemia (9). Even with the improvements in spatial resolution, PET still falls short of enabling quantification of transmural extent of myocardial perfusion. Thus, there are strengths and limitations of both the SPECT and PET functional approaches and the anatomic approach of coronary CT angiography.
Alternatively, several recent studies have evaluated the feasibility of hybrid imaging by SPECT-CT or PET-CT, with aims to maximize the advantages of both functional and anatomic imaging methods (10,11). These early studies suggest enhanced diagnostic performance by hybrid imaging, as compared with functional or anatomic imaging alone, for the detection of “functionally significant” CAD. However, these modalities still require two separate imaging technologies, result in additional cost and time and significant increases in the overall radiation dose (10).
Novel technologies for non-invasive functional assessement using cardiac CT
On the basis of these considerations, several methods were developed and suggested to have the ability to combine anatomical data from coronary CT angiography together with the physiological significance during a single examination.
CT myocardial perfusion imaging
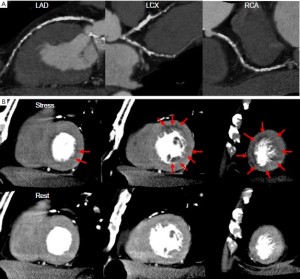
One strategy is to combine coronary CT angiography with CT perfusion imaging (Figure 1). Experimental work has revealed the feasibility of adenosine-augmented CT myocardial perfusion imaging for the detection of perfusion deficit during first-pass 64-detector CT imaging using a canine model (12). In this study, multidetector CT-based estimates of myocardial perfusion have been validated against microsphere-derived measurement of myocardial blood flow (12). Recently, several clinical trials have shown the feasibility and diagnostic accuracy of adenosine stress CT perfusion imaging for the detection of perfusion abnormalities, which is comparable to those of SPECT (13-15). George et al., studied 40 patients with abnormal SPECT perfusion imaging who underwent adenosine stress CT perfusion and coronary CT angiography (14). In a subset of 27 patients who underwent invasive coronary angiography, CT perfusion imaging, when combined with coronary CT angiography, accurately predicted coronary stenosis causing perfusion deficits as compared to the combination of quantitative coronary angiography and SPECT as a reference standard with sensitivity, specificity, PPV, and NPV of 86%, 92%, 92%, and 85%, respectively. In comparison to SPECT, CT has improved spatial resolution and is expected to be better at detecting small areas of ischemia or infarction. Importantly, in this study, CT perfusion imaging detected transmural differences in myocardial perfusion that can be accurately quantified as the transmural perfusion ratio (subendocardial/subepicardial attenuation density), and these differences were inversely related to the percentage of diameter stenosis measured at quantitative angiography (14). Furthermore, CT perfusion could offer improved accuracy for detecting multivessel disease because actual rather than relative blood flow patterns are assessed, thus avoiding false negatives that can occur in the setting of balanced myocardial ischemia.
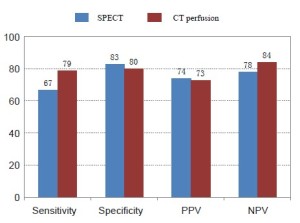
Blankstein et al. reported the diagnostic accuracy of adenosine stress CT perfusion for the identification of hemodynamically significant stenosis as compared with that of SPECT (15). The study included 34 patients who underwent SPECT and invasive coronary angiography. On a per-vessel basis, CT perfusion alone had a sensitivity of 79% and a specificity of 80% for the detection of stenosis ≥50%, while those for SPECT perfusion imaging were 67% and 83%, respectively (Figure 2). For the detection of vessels with ≥50% stenosis with a corresponding SPECT perfusion abnormality, CT perfusion had a sensitivity of 93% and a specificity of 74%. In this study, the comprehensive cardiac CT protocol included coronary CT angiography, as well as stress perfusion, rest perfusion, and delayed-enhancement imaging, with an average radiation dose of 12.7 mSv. An important advantage of CT perfusion imaging is the ability to simultaneously visualize both anatomical CAD and its physiological consequences. However, there are several limitations that are pertinent to CT perfusion imaging. First, although the radiation exposure of comprehensive cardiac CT examination was equivalent to that of SPECT (15), it is still high. Second, in comparison to conventional coronary CT angiography, a larger volume of iodinated contrast is required as both rest and stress images are acquired. Third, CT perfusion imaging performed during adenosine infusion increases heart rate and thus the likelihood of artifactual reduction in CT attenuation densities caused by heart motion, partial volume effects, and beam-hardening artifiacts, which can be mistaken for myocardial perfusion deficits. Finally, CT perfusion imaging does not provide lesion-specific ischemia data and cannot distinguish between diffuse disease and stenoses which may be targets for revascularization. Newer scanners with wide-area coverage (such as 256-slice and 320-detector row CT scanners) permit single axial image acquisition of the heart in a single heartbeat and have several potential advantages in CT perfusion imaging. Whether simultaneous imaging of all myocardial segments renders different diagnostic performance as compared with sequential imaging of the heart remains unknown. However, shorter scanning time, with elimination of redundant radiation from helical oversampling or overlapping of sequential axial acquisitions, translates to lower than expected radiation dose, and will allow imaging at the higher heart rate commonly experienced during adenosine infusion.
CT-derived computed FFR (FFRCT)
Fractional flow reserve (FFR), defined as the ratio of maximal blood flow in a stenotic artery to maximal flow if the artery were normal, serves as an index of the physiologic importance of coronary artery stenosis. In the FAME (Fractional Flow Reserve versus Angiography for Multivessel Evaluation) study, of 1,005 patients with multivessel CAD, those that underwent FFR-guided revascularization, as compared to patients undergoing angiogram-guided revascularization, experienced lower rates of adverse events with fewer coronary stents and lower healthcare costs (16,17). However, measurement of FFR requires invasive cardiac catheterization, an expensive coronary pressure wire and intravenous or intracoronary adenosine infusion.
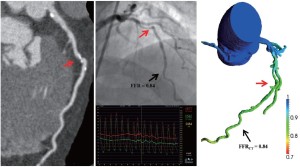
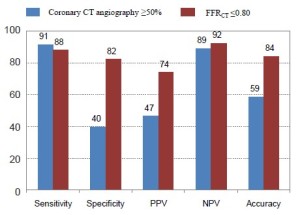
Computational fluid dynamics, as applied to coronary CT angiography images, represents a novel non-invasive method that quantitates coronary blood flow, flow velocity and pressure in the major epicardial coronary arteries. Simulation of maximum hyperemic coronary blood flow, such as occurs with adenosine infusion, allows calculation of fractional flow reserve and determination of lesion-specific FFR (Figure 3) (18-20). The feasibility and diagnostic performance of CT-derived computed FFR (FFRCT) were evaluated in the study entitled Diagnosis of Ischemia-Causing Stenoses Obtained Via Non-invasive Fractional Flow Reserve (DISCOVER FLOW), conducted at 5 hospitals internationally, which prospectively enrolled 103 patients (159 lesions) who had undergone coronary CT angiography (21). In this study, all patients also underwent invasive angiography with FFR, with lesion-specific ischemia defined as an FFR ≤0.80. Computed FFRCT values were found to have a very high degree of correlation with invasively measured FFR. As expected, coronary CT angiography alone showed high sensitivity of 91% and NPV of 89%, but comparatively low specificity of 40% and PPV of 47% for the identification of lesion-specific ischemia. By comparison, FFRCT produced sensitivity of 88% and NPV of 92%, similar to those of coronary CT angiography, but much higher specificity of 82% and PPV of 74%, resulting overall accuracy increased by 25% (Figure 4). While the result is encouraging, the data regarding the clinical value of FFRCT are still limited and further study in a larger number of patients as well as comparison to other noninvasive and invaisive studies is needed. A larger, prospective multicenter clinical trial, the DeFACTO study (Determination of Fractional Flow Reserve by Anatomic Computed Tomographic Angiography) is similarly designed to determine the diagnostic performance of FFRCT for the non-invasive assessment of lesion-specific ischemia using measured FFR as the reference standard (22). This multi-national 17 center, 285 patients study has completed patient enrollment and results are expected in the near future.
FFRCT is a unique technology for the physiologic assessment of ischemia by cardiac CT. Although adenosine stress CT myocardial perfusion imaging also has the potential to assess the hemodynamic significance of an anatomic lesion, FFRCT may offer several advantages over stress perfusion methods. First, FFRCT technology is based on the physiologic models and the calculation of FFRCT does not require modification of typical coronary CT angiography protocols, does not require the administration of additional medication including adenosine, and does not confer any additional radiation. Further given its index of epicardial stenosis-related ischemia, FFRCT allows the precise pinpointing of lesions that cause functional reduction in blood flow and may thus enhance specificity of lesion detection over stress testing for which perfusion deficits may occur due to epicardial coronary stenosis, microcirculatory dysfunction or both. The calculation of FFRCT requires uploading the CT scan DICOM image dataset to HeartFlow, Inc servers for image analysis, geometric modeling and supercomputer computation. This process currently takes several hours per exam. Iterative improvements in automation are expected reduce processing time in the near future.
Conclusions
Criticisms of coronary CT angiography have focused on the inability of coronary CT angiography to assess the “functional” significance of an identified coronary stenosis. CT myocardial perfusion imaging and CT-derived computed FFR represent significant advances in the field of cardiac CT, with ability to combine anatomical data from CT angiography together with the physiologic information. These noninvasive ‘all-in-one’ technologies may reduce unnecessary invasive coronary angiography and revascularization procedures. However, data on the clinical value and cost-effectiveness of these technologies is still limited. While non-invasive anatomic-functional testing prior to cardiac catheterization and intervention have the potential to significantly improve patient outcomes and reduce costs, further studies with appropriate and larger patient cohorts are needed prior to widespread clinical adoption of these diagnostic techniques.
Acknowledgments
I thank Dr. Hajme Sakuma and Dr. Kakuya Kitagawa from Mie university hospital for their support in writing this article.
Disclosure: The authors declare no conflict of interest.
References
- Schauer DA, Linton OW. National Council on Radiation Protection and Measurements report shows substantial medical exposure increase. Radiology 2009;253:293-6. [PubMed]
- Budoff MJ, Dowe D, Jollis JG, et al. Diagnostic performance of 64-multidetector row coronary computed tomographic angiography for evaluation of coronary artery stenosis in individuals without known coronary artery disease: results from the prospective multicenter ACCURACY (Assessment by Coronary Computed Tomographic Angiography of Individuals Undergoing Invasive Coronary Angiography) trial. J Am Coll Cardiol 2008;52:1724-32. [PubMed]
- Meijboom WB, Meijs MF, Schuijf JD, et al. Diagnostic accuracy of 64-slice computed tomography coronary angiography: a prospective, multicenter, multivendor study. J Am Coll Cardiol 2008;52:2135-44. [PubMed]
- Miller JM, Rochitte CE, Dewey M, et al. Diagnostic performance of coronary angiography by 64-row CT. N Engl J Med 2008;359:2324-36. [PubMed]
- Meijboom WB, Van Mieghem CA, van Pelt N, et al. Comprehensive assessment of coronary artery stenoses: computed tomography coronary angiography versus conventional coronary angiography and correlation with fractional flow reserve in patients with stable angina. J Am Coll Cardiol 2008;52:636-43. [PubMed]
- Gaemperli O, Schepis T, Valenta I, et al. Functionally relevant coronary artery disease: comparison of 64-section CT angiography with myocardial perfusion SPECT. Radiology 2008;248:414-23. [PubMed]
- Shaw LJ, Hachamovitch R, Berman DS, et al. The economic consequences of available diagnostic and prognostic strategies for the evaluation of stable angina patients: an observational assessment of the value of precatheterization ischemia. Economics of Noninvasive Diagnosis (END) Multicenter Study Group. J Am Coll Cardiol 1999;33:661-9. [PubMed]
- Schuijf JD, Wijns W, Jukema JW, et al. Relationship between noninvasive coronary angiography with multi-slice computed tomography and myocardial perfusion imaging. J Am Coll Cardiol 2006;48:2508-14. [PubMed]
- Chung SY, Lee KY, Chun EJ, et al. Comparison of stress perfusion MRI and SPECT for detection of myocardial ischemia in patients with angiographically proven three-vessel coronary artery disease. AJR Am J Roentgenol 2010;195:356-62. [PubMed]
- Rispler S, Keidar Z, Ghersin E, et al. Integrated single-photon emission computed tomography and computed tomography coronary angiography for the assessment of hemodynamically significant coronary artery lesions. J Am Coll Cardiol 2007;49:1059-67. [PubMed]
- Sampson UK, Dorbala S, Limaye A, et al. Diagnostic accuracy of rubidium-82 myocardial perfusion imaging with hybrid positron emission tomography/computed tomography in the detection of coronary artery disease. J Am Coll Cardiol 2007;49:1052-8. [PubMed]
- George RT, Silva C, Cordeiro MA, et al. Multidetector computed tomography myocardial perfusion imaging during adenosine stress. J Am Coll Cardiol 2006;48:153-60. [PubMed]
- Kurata A, Mochizuki T, Koyama Y, et al. Myocardial perfusion imaging using adenosine triphosphate stress multi-slice spiral computed tomography: alternative to stress myocardial perfusion scintigraphy. Circ J 2005;69:550-7. [PubMed]
- George RT, Arbab-Zadeh A, Miller JM, et al. Adenosine stress 64- and 256-row detector computed tomography angiography and perfusion imaging: a pilot study evaluating the transmural extent of perfusion abnormalities to predict atherosclerosis causing myocardial ischemia. Circ Cardiovasc Imaging 2009;2:174-82. [PubMed]
- Blankstein R, Shturman LD, Rogers IS, et al. Adenosine-induced stress myocardial perfusion imaging using dual-source cardiac computed tomography. J Am Coll Cardiol 2009;54:1072-84. [PubMed]
- Tonino PA, De Bruyne B, Pijls NH, et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med 2009;360:213-24. [PubMed]
- Fearon WF, Bornschein B, Tonino PA, et al. Economic evaluation of fractional flow reserve-guided percutaneous coronary intervention in patients with multivessel disease. Circulation 2010;122:2545-50. [PubMed]
- Kim HJ, Jansen KE, Taylor CA. Incorporating autoregulatory mechanisms of the cardiovascular system in three-dimensional finite element models of arterial blood flow. Ann Biomed Eng 2010;38:2314-30. [PubMed]
- Kim HJ, Vignon-Clementel IE, Coogan JS, et al. Patient-specific modeling of blood flow and pressure in human coronary arteries. Ann Biomed Eng 2010;38:3195-209. [PubMed]
- Kim HJ, Vignon-Clementel IE, Figueroa CA, et al. On coupling a lumped parameter heart model and a three-dimensional finite element aorta model. Ann Biomed Eng 2009;37:2153-69. [PubMed]
- Koo BK, Erglis A, Doh JH, et al. Diagnosis of ischemia-causing coronary stenoses by noninvasive fractional flow reserve computed from coronary computed tomographic angiograms. Results from the prospective multicenter DISCOVER-FLOW (Diagnosis of Ischemia-Causing Stenoses Obtained Via Noninvasive Fractional Flow Reserve) study. J Am Coll Cardiol 2011;58:1989-97. [PubMed]
- Min JK, Berman DS, Budoff MJ, et al. Rationale and design of the DeFACTO (Determination of Fractional Flow Reserve by Anatomic Computed Tomographic AngiOgraphy) study. J Cardiovasc Comput Tomogr 2011;5:301-9. [PubMed]


