Conus artery occlusion causing isolated right ventricular outflow tract infarction: novel application of cardiac magnetic resonance in anterior STEMI
Introduction
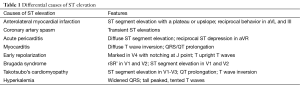
Acute ST elevation in the precordial leads usually indicates an anterior left ventricular (LV) infarction, the differential diagnoses are broad (Table 1). Although rare, an isolated right ventricular (RV) myocardial infarction, particularly from acute conus branch occlusion, could cause V1-V3 ST segment elevation; it accounts for approximately 3% of all cases of myocardial infarction (1). In the setting of acute ST segment elevation, elevated troponins, an unchanged transthoracic echo and unremarkable coronary angiogram, cardiac magnetic resonance (CMR) can serve as a useful diagnostic tool.
Full table
Case presentation
Sixty years old man with a medical history of bicuspid aortic valve, asymptomatic moderate-severe aortic stenosis (indexed valve area 0.6 cm2/m2), and progressive ascending aorta dilatation (50 mm at the mid-level) presented to a local hospital with left-sided numbness and impaired gait. He was diagnosed with an embolic middle cerebral artery (MCA) stroke (Figure 1), and transesophageal echocardiogram revealed new mobile echo densities on the aortic side of his bicuspid aortic valve (Figure 2). Work-up for infective endocarditis, including culture-negative endocarditis, was unrevealing. Cardiovascular surgery consultation recommended aortic valve replacement, but the patient deferred.

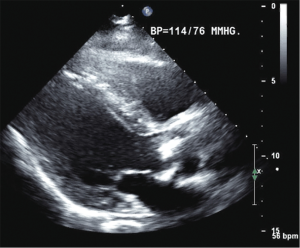
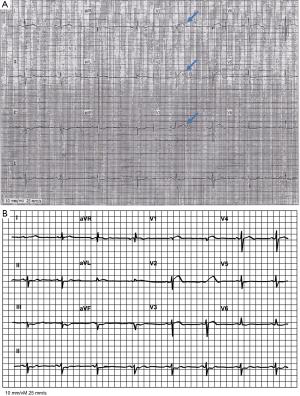
Two weeks later, he presented with acute onset of left substernal chest pain radiating to his jaw, and electrocardiogram revealed ST elevations in leads V1, V2, and V3 (Figure 3). Chest X-ray was unremarkable, and troponins were initially negative. For this presumed acute coronary syndrome, the patient received aspirin, clopidogrel, heparin and eptifibatide. He was not given thrombolytics because of recent stroke. He was transferred to our tertiary referral center for further management. Upon arrival, repeat electrocardiography continued to illustrate ST elevations in the precordial leads, and laboratory values demonstrated an elevated troponin T of 0.05 ng/mL with significant upward trend (0.05→0.14→0.28 ng/mL, normal range <0.01 ng/mL). Physical exam revealed a normotensive male with a harsh, 3/6 late peaking systolic murmur throughout the precordium and normal respiratory exam. The coronary angiogram demonstrated no significant left coronary arteries (LCA) disease. The right coronary artery (RCA) was not easily engaged; because of the known presence of aortic valve mobile masses, non-selective imaging via an aortogram (Figure 4) demonstrated a widely patent RCA with normal flow.
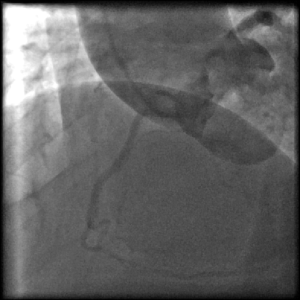
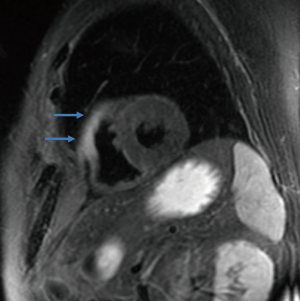
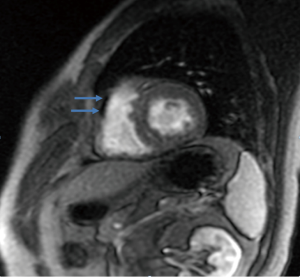
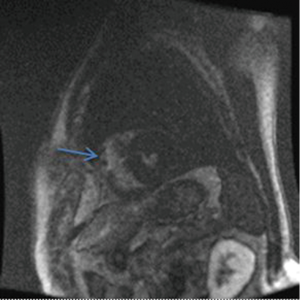
Isolated RV infarction was considered a possible diagnosis given the typical chest pain, troponin rise, ST elevations, mobile mass as a source of embolus, and normal LCA. A repeat transthoracic echocardiogram did not demonstrate any regional wall motion abnormalities, so CMR imaging was used to further evaluate the potential causes of ST segment elevation. CMR revealed an acute myocardial infarction isolated to the right ventricular outflow tract (RVOT), presumably in the conus territory with associated edema, hypoperfusion, and dyskinesis of the RV free wall near the RVOT (Figures 5-7). Retrospective review of the aortogram failed to demonstrate any contrast filling of the conus artery.
Standard treatment for the acute coronary syndrome was continued, and 5 days postinfarction he underwent aortic valve replacement with a 27-mm Carbo-Medics mechanical valve, ascending aorta and hemiarch replacement. He is doing well 11 months post-operatively.
Conclusions
ST segment elevation in the precordial leads is considered characteristic of an anterior LV myocardial infarction, often secondary to left anterior descending artery occlusion. The conus artery, often the first branch of the RCA, supplies the RVOT (2). Occasionally, an acute myocardial infarction can result from occlusion of the conus branch, resulting in an isolated RV infarction. Characteristic elevation of ST segments in leads V1 through V3 has been described in previous accounts of conus branch occlusion (3,4). RV infarction often occurs in the setting of an inferior wall LV infarction, with ST elevation in lead V1 and the inferior leads II, III, and aVF. The anterior forces from an isolated RV infarction can appear as an anterior ST elevation similar to an anterior LV infarction if an inferior LV infarction is not present to suppress the ST elevation in the precordial leads.
Differentiating an isolated RV from an LV infarction based only upon ST segment elevation in leads V1-V3 is difficult (4). Our case illustrated a patient with anterior ST segment elevation, increased cardiac troponin levels, and angiographically normal LCA. An isolated RV infarction was in the differential, so CMR was utilized to diagnose the cause of ST-segment elevation. Coronary artery CT angiography (CCTA) has been shown to visualize the conus artery and the speed with which CCTA can be performed as well as its relative compatibility with magnetic resonance imaging (MRI) incompatible metal shrapnel/devices is an advantage (5). This article illustrates two points. First, the emerging role of CMR in determining the etiology of troponin rise in the setting of anterior ST elevation with no obvious stenotic lesions on coronary angiography. Our case is only the second reported case of an isolated RVOT infarction presenting with ST-segment elevation in the precordial leads as diagnosed by CMR. Secondly, because a conus artery is small with a resultant small RV infarct, it may often be overlooked with traditional imaging such as echocardiography and angiography (2).
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this Case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
- Porter A, Herz I, Strasberg B. Isolated right ventricular infarction presenting as anterior wall myocardial infarction on electrocardiography. Clin Cardiol 1997;20:971-3. [Crossref] [PubMed]
- Levin DC, Beckmann CF, Garnic JD, et al. Frequency and clinical significance of failure to visualize the conus artery during coronary arteriography. Circulation 1981;63:833-7. [Crossref] [PubMed]
- Muhammad KI, Kapadia SR. Anterior ST-segment elevation with right coronary artery occlusion: a unique case of isolated right ventricular infarction. Angiology 2008;59:622-4. [Crossref] [PubMed]
- Fabris E, Morocutti G, Sinagra G, et al. Uncommon cause of ST-segment elevation in V1-V3: incremental value of cardiac magnetic resonance imaging. Clin Res Cardiol 2014;103:825-8. [Crossref] [PubMed]
- Erol C, Seker M. The prevalence of coronary artery variations on coronary computed tomography angiography. Acta Radiol 2012;53:278-84. [Crossref] [PubMed]