Evaluation of fetal echocardiography as a routine antenatal screening tool for detection of congenital heart disease
Introduction
Congenital heart defects (CHDs) are one of the most common forms of congenital anomalies found in humans. Their approximate incidence is about 6 in 1,000 live births and about 8 to 10 in 1,000 pregnancies (1). CHDs are responsible for about 40% of perinatal deaths (2) of which more than 20% of deaths occur in the first month of life (3). CHDs therefore significantly contribute to the economic burden on health care systems. Prenatal foetal echocardiography is the only means of detecting such defects. This foetal echocardiography is mostly reserved in high risk pregnancies where CHDs incidence is traditionally higher. The present study is conducted to find out the incidence of CHDs in an unselected population of pregnant in comparison to high risk pregnant women, and to evaluate the role of routine prenatal foetal echocardiography as a screening tool for detection of CHD.
Aim of the study
Assess the incidence of CHDs by fetal echocardiography in an unselected population of pregnant women in comparison with pregnant women with conventional high risk factors for CHD.
Subjects and methods
This is a prospective study conducted at Kasturba Hospital Manipal, a tertiary care hospital in southern India. Institutional Ethics committee clearance was obtained. The duration of study was 4 years. The study subjects included all pregnant women who attended our antenatal unit between 2008 and 2012. All pregnant women who visited our antenatal clinic were enrolled in the study after informed consent, irrespective of risk factors for CHD. They were categorized into two groups—high risk and low risk.
High risk group included pregnant women having any known risk factors for CHDs, which are traditional indications for fetal echocardiography as laid down by Pediatric Council of the American Society of Echocardiography (Table 1). Low risk group included pregnant women with no known risk factors for CHD. The detailed fetal echocardiography examination was done between 18 and 28 weeks of gestation. Echocardiography was done by a single qualified operator using a 7 GE ultrasound Doppler system with 3.5 to 5 MHz transducer (GE linear array transducer). The echocardiography was performed according to the International Society of Ultrasound in Obstetrics and Gynecology (ISUOG) guidelines for fetal echocardiography. The foetal heart could be visualized clearly in all cases. The echocardiography included an apical four chamber view of the heart, an apical five chamber view, a long axis view of right ventricular outflow tract, a short axis view at the level of arterial trunks, a short axis view at level of ventricles, a long axis view of caval veins, a view of ductal arch and a view of aortic arch. Foetal heart rate was noted and any arrhythmia was confirmed with M-mode imaging. Colour Doppler, Pulse Wave Doppler were used whenever necessary. All the images were recorded and stored in a digital media. Level 2 ultrasound were done universally in all patients in the obstetrics department.

Full table
Statistical analysis
Power of the study was calculated as follows. For the current study to have an 80% power and an alpha error of 0.05 the calculated sample size was 961. We had a sample size of 1,280 pregnant women. Hence the study was adequately powered to see the difference between the two groups.
Results
A total of 1,280 pregnant women were included in study. Of the total cases, 118 women were categorized into high risk group while remaining 1,162 were included in the low risk group. Twenty-six cases of CHDs were detected based on abnormal foetal echocardiography. Therefore, the incidence of prenatally diagnosed CHD in our study is 20.3 per 1,000 pregnancies. Table 2 shows the distribution of cases in both the groups. The various reasons for failure of recognition of the congenital heart disease were also noted which has been highlighted in the Table 3. Only 2 of the 26 cases of CHD occurred in high risk group whereas the remaining 24 occurred in low risk pregnancy. The incidence of congenital heart disease in in high risk and low risk group was 16.9% per 1,000 and 22.3 per 1,000 respectively. The difference in the incidence of CHDs between the two groups was not significant statistically (P=0.76). Therefore, our study shows that there is no difference in incidence of CHDs between pregnancies associated with high risk factors compared to low risk pregnancies though there was trend of higher cases of CHD in low risk group.
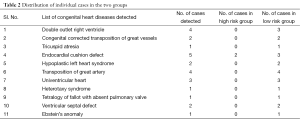
Full table
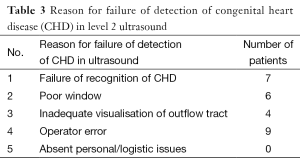
Full table
Discussion
CHDs are one of the most common forms of congenital anomalies found in humans. Early detection of CHDs in prenatal period by foetal echocardiography is of paramount importance in management of such cases. Prental diagnosis helps family in making a decision regarding the outcome of pregnancy including termination. Prenatal diagnosis of CHDs also decreases mortality and morbidity by smooth transition between pre and post natal states by providing the appropriate medical care immediately after birth (4-9). Studies have shown that prenatal diagnosis improves neonatal survival after surgical repair compared to post natal diagnosis (10-11). It will also prevent mental trauma to the parents by providing them adequate time to understand the pathophysiology of the disease and giving them an opportunity to take a sound decision regarding the outcome of the pregnancy. The timing of the foetal echo is usually between 18-20 weeks, which enables us to take decision regarding the outcome of the pregnancy at this time of pregnancy.
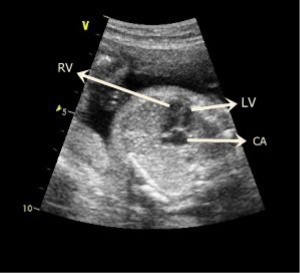
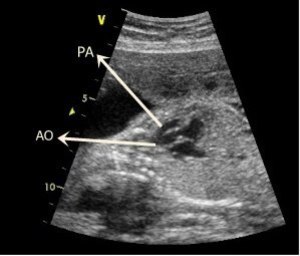
Routine prenatal ultrasound scanning may not be an ideal modality for screen for CHD (12). A large number of cases of CHD go undetected because of not being detected by the routine abdominal ultrasound screening scan. Foetal echocardiography being more sensitive and specific is able to detect most of the CHD cases. Earlier studies have emphasized the importance of routine foetal screening for CHD (13-15). The four chamber view of heart has a detection rate of 4.5% to 8.1% (Figure 1) which increases to 43.8% to 85.5% when views showing the right and left ventricular outflow tracts are performed (Figure 2). However when foetal echocardiography which involves a detailed, focused assessment of the foetal cardiovascular system is performed, the rate of detection of CHDs exceeds 85% to 90% (1). Despite the disparity in detection rates of CHDs between routine obstetrical scan and detailed foetal echocardiography, not every pregnant is subjected to foetal echocardiography. Foetal echocardiography is a time consuming procedure that requires skilled investigators, hence it is not a part of routine antenatal screening. This makes cardiac abnormalities as one of the major malformations frequently missed in routine abdominal scans. Currently detailed foetal echocardiography is provided only to those pregnant women who have risk factors for CHDs associated with their pregnancies as liad down by Pediatric Council of the American Society of Echocardiography (Table 1) (16). In our current study we studied the role of foetal echocardiography in detection of CHD in unselected pregnant woman who lacks traditional high risk factors for the CHD.
The incidence of CHD as seen in our study is 20.3 per 1,000 pregnancies which are higher than that found in general population (8 per 1,000 pregnancies) (1). In a previous similar study by Stümpflen et al., they also reported a higher incidence of CHD detected by foetal echocardiography (14.9 per 1,000 pregnancies) (17). This could be because of undetected cases of CHDs in the general population. Rates of occurrence of CHDs between the high risk and low risk group were 16.9% per 1,000 and 22.3 per 1,000 respectively which was statistically not significant. Large proportion of cases of CHD was detected in low risk group (24 out of 26 cases). Based on these findings it is highly suggestive that every pregnant woman should be subjected to a detailed foetal echocardiography. Our study showed that a high proportion of prenatally detectable cases of congenital heart disease (24 of 26 cases) occurred in pregnant women with no risk factors, which could be diagnosed solely because of foetal echocardiography as a part of routine prenatal screening investigations. We also evaluated the level 2 ultrasounds (if done universally in the patient population included in the study) were performed according to the recent ISUOG/ACOG guidelines and the reasons for failed detection of congenital heart disease on the level 2 ultrasound (failure of recognition of CHD, non-identification of outflow tracts/inadequate visualization of the heart, operator error, available equipment and personnel). This early detection of CHD in early pregnancy given adequate time for physician to discuss severity, and prognosis of the disease with the family, where they can still make a decision regarding the course of pregnancy. These cases are those which otherwise would have been missed on antenatal screening, or would have been diagnosed at late pregnancy where decision making would have been more difficult.
While theoretical concerns exist regarding the harmful effects of ultrasound energy on the developing foetus, no confirmed effect has been detected till date (18). However, those performing foetal echocardiography should be aware of these effects and power output as well as time of exposure should be minimized to avoid the ill effects, if any.
Limitations of the study
Follow up post natal echocardiography of all the cases could not be done in our study which would have provided us with more critical information regarding sensitivity and specificity of fetal echocardiography and also about the outcome of the pregnancies.
Conclusions
We would like to emphasize that foetal echocardiography should be included as a part of routine antenatal screening irrespective of risk factors for CHDs.
Acknowledgements
We sincerely thank the patients and relatives for their co-operation and consent for publication of data in the medical journal.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Rodger M. Evidence base for the management of venous thromboembolism in pregnancy. Hematology Am Soc Hematol Educ Program 2010;2010:173-80.
- Abu-Harb M, Hey E, Wren C. Death in infancy from unrecognised congenital heart disease. Arch Dis Child 1994;71:3-7. [PubMed]
- Young ID, Clarke M. Lethal malformations and perinatal mortality: a 10 year review with comparison of ethnic differences. Br Med J (Clin Res Ed) 1987;295:89-91. [PubMed]
- Crawford DC, Chita SK, Allan LD. Prenatal detection of congenital heart disease: factors affecting obstetric management and survival. Am J Obstet Gynecol 1988;159:352-6. [PubMed]
- Bonnet D, Coltri A, Butera G, et al. Detection of transposition of the great arteries in fetuses reduces neonatal morbidity and mortality. Circulation 1999;99:916-8. [PubMed]
- Allan LD, Apfel HD, Printz BF. Outcome after prenatal diagnosis of the hypoplastic left heart syndrome. Heart 1998;79:371-3. [PubMed]
- Satomi G, Yasukochi S, Shimizu T, et al. Has fetal echocardiography improved the prognosis of congenital heart disease? Comparison of patients with hypoplastic left heart syndrome with and without prenatal diagnosis. Pediatr Int 1999;41:728-32. [PubMed]
- Kumar RK, Newburger JW, Gauvreau K, et al. Comparison of outcome when hypoplastic left heart syndrome and transposition of the great arteries are diagnosed prenatally versus when diagnosis of these two conditions is made only postnatally. Am J Cardiol 1999;83:1649-53. [PubMed]
- Jaeggi ET, Sholler GF, Jones OD, et al. Comparative analysis of pattern, management and outcome of pre- versus postnatally diagnosed major congenital heart disease: a population-based study. Ultrasound Obstet Gynecol 2001;17:380-5. [PubMed]
- Tworetzky W, McElhinney DB, Reddy VM, et al. Improved surgical outcome after fetal diagnosis of hypoplastic left heart syndrome. Circulation 2001;103:1269-73. [PubMed]
- Verheijen PM, Lisowski LA, Stoutenbeek P, et al. Prenatal diagnosis of congenital heart disease affects preoperative acidosis in the newborn patient. J Thorac Cardiovasc Surg 2001;121:798-803. [PubMed]
- Buskens E, Grobbee DE, Frohn-Mulder IM, et al. Efficacy of routine fetal ultrasound screening for congenital heart disease in normal pregnancy. Circulation 1996;94:67-72. [PubMed]
- D'Alton ME, DeCherney AH. Prenatal diagnosis. N Engl J Med 1993;328:114-20. [PubMed]
- Copel JA, Pilu G, Green J, et al. Fetal echocardiographic screening for congenital heart disease: the importance of the four-chamber view. Am J Obstet Gynecol 1987;157:648-55. [PubMed]
- Sandor GG, Farquarson D, Wittmann B, et al. Fetal echocardiography: results in high-risk patients. Obstet Gynecol 1986;67:358-64. [PubMed]
- Rychik J, Ayres N, Cuneo B, et al. American Society of Echocardiography guidelines and standards for performance of the fetal echocardiogram. J Am Soc Echocardiogr 2004;17:803-10. [PubMed]
- Stümpflen I, Stümpflen A, Wimmer M, et al. Effect of detailed fetal echocardiography as part of routine prenatal ultrasonographic screening on detection of congenital heart disease. Lancet 1996;348:854-7. [PubMed]
- Abramowicz JS, Kossoff G, Marsál K, et al. Literature review by the ISUOG Bioeffects and Safety Committee. Ultrasound Obstet Gynecol 2002;19:318-9. [PubMed]


