Ruptured aneurysm of major aortopulmonary collateral artery: management using amplatzer vascular plug
Introduction
Hemoptysis in cyanotic congenital heart disease is usually attributed to pulmonary infection, rupture of hypertrophied bronchial artery or coagulation disorders. Pulmonary atresia and ventricular septal defect (PA-VSD) belong to a group of congenital cardiac malformations and is usually associated with presence of major aortopulmonary collateral arteries (MAPCAs). Aneurysmal dilatation of MAPCAs has also been described and may be associated with compression of adjacent structures, persistent pleural effusions, hemoptysis and sudden death (1,2). Elective curative management usually involves staged approach which provides individualized treatment by matching the approach to the specific anatomy and physiology of each patient. Endovascular management plays a vital role in preoperative embolization of MAPCAs and can be life saving in cases of massive hemoptysis.
Case presentation
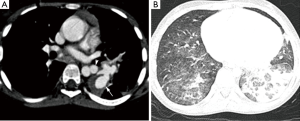
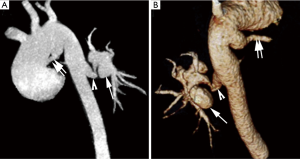
A 6-year-old female child presented with massive hemoptysis requiring blood transfusion and ventilatory support. She was a diagnosed case of tetralogy of Fallot. She also had a history of recurrent hemoptysis since last three months (four episodes, each episode of 2–2.5 mL fresh blood). CT angiography (CTA) revealed large subaortic VSD with aortic override, pulmonary atresia, large patent ductus arteriosus (PDA) and MAPCAs (Figure 1). In addition to this, there was a large, lobulated aneurysm with surrounding soft tissue seen arising from the MAPCA supplying left lung (Figure 2A). In addition there was consolidation in left lower lobe with ground glass opacities in bilateral lower lobes, right middle lobe and lingula (Figure 2B). Reformatted CT images depicted the large PDA, MAPCA and its aneurysm very well (Figure 3A,B). Although she was initially managed medically, this was unsuccessful and she remained ventilator dependent.

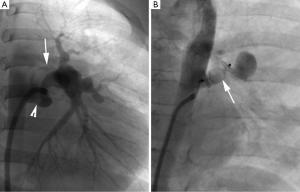
She was referred for angiography with an intention to occlude the MAPCA supplying the aneurysm which was presumed to be the cause of hemoptysis. Baseline oxygen saturation was 70%. Selective angiogram of the MAPCA demonstrated the aneurysm with delayed filling of its large lobulation (Figure 4A). There was no obvious leakage of contrast from the aneurysm. This MAPCA (diameter-7 mm) supplying the aneurysm was occluded using 10 mm Amplatzer vascular plug (AVP II) released via 7 F guiding catheter (Figure 4B). Second generation Amplatzer vascular plug was used as it allows rapid vessel occlusion. Its trilobular design with six layers of mesh offers better occlusive properties. Post procedure oxygen saturation was 76%. She had no further episode of hemoptysis, following which the patient was taken up for corrective surgery. She was weaned off from ventilation on day four and was doing well on follow up.
Discussion
Aortopulmonary collaterals (APCs) associated with PA-VSD are well described. The pulmonary circulation in these cases can be from native pulmonary arteries, systemic collateral arteries, or a combination of the two. Major Aortopulmonary collateral arteries (MAPCAs) are large systemic collateral arteries; usually originating from the descending thoracic aorta (70%), the branch of aortic arch (15–20%), and the ascending aorta (10–15%) (4). Occasionally they may arise from the abdominal aorta or uncommonly from other systemic arteries such as carotid or coronary arteries (5). Aneurysmal dilatation of MAPCA has been described which may occasionally cause symptoms due to the compression of adjacent structures (1). It may also cause life threatening hemoptysis due to rupture or even death (1,2). These collaterals may also predispose to pleural effusions (6). MAPCAs also constitute a remediable cause of failure to wean from ventilation in post-operative patients.
MAPCAs are usually well depicted on multi-detector computed tomography (MDCT) which may provide an efficient road map for further treatment planning (7). Elective curative management of PA-VSD usually involves a multi-staged surgical approach. Percutaneous closure of APCs has been described as an adjunct to surgery with the use of mechanically detachable coils (8). Few cases of elective occlusion of larger vessels with a variety of devices have also been described (9,10). Embolization procedure may involve risk of device migration, non-target embolization, lung infarction and recanalization (11). Occlusion of APCs in Fontan patients is associated with improved clinical outcome (12). Endovascular management can be life saving in some cases of massive hemoptysis. In our case, MDCT evaluation showed large aneurysm of MAPCA with contained rupture and based on the findings on MDCT scan and due to deteriorating clinical condition, vascular plug occlusion was planned. Optimal sized device that was 30–50% larger than the target vessel diameter was used. To the best of our knowledge, this is the first reported case where an Amplatzer vascular plug has been deployed.
In conclusion, aneurysmal dilatation of MAPCA in patients with PA-VSD may give rise to life threatening hemoptysis due to its rupture and may even lead to death. Urgent endovascular management may be life saving in some cases. Moreover, evaluation using noninvasive imaging modality like MDCT helps in mapping appropriate endovascular management.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed consent: Written informed consent was obtained from the parents of the patient for publication of this Case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
- Lanjewar C, Shiradkar S, Agrawal A, et al. Aneurysmally dilated major aorto-pulmonary collateral in tetralogy of Fallot. Indian Heart J 2012;64:196-7. [Crossref] [PubMed]
- Miyazaki O, Nosaka S, Hayakawa M, et al. Sudden death due to rupture of major aortopulmonary collateral arteries in a patient with tetralogy of Fallot and pulmonary atresia. Emerg Radiol 2001;8:293-6. [Crossref]
- Sharma A, Kumar S, Priya S. Depicts entire anatomical detail of pulmonary arterial supply and major aorto-pulmonary collateral artery aneurysm. Asvide 2016;3:214. Available online: http://www.asvide.com/articles/971
- Choi JY, Lee JK, Cha ES, et al. Origins, distributions and characteristics of collateral circulation in pulmonary atresia with ventricular septal defect: a cineangiographic study. Korean Circ J 1998;28:1561-76. [Crossref]
- Tchervenkov CI, Roy N. Congenital Heart Surgery Nomenclature and Database Project: pulmonary atresia-ventricular septal defect. Ann Thorac Surg 2000;69:S97-105. [Crossref] [PubMed]
- Spicer RL, Uzark KC, Moore JW, et al. Aortopulmonary collateral vessels and prolonged pleural effusions after modified Fontan procedures. Am Heart J 1996;131:1164-8. [Crossref] [PubMed]
- Maeda E, Akahane M, Kato N, et al. Assessment of major aortopulmonary collateral arteries with multidetector-row computed tomography. Radiat Med 2006;24:378-83. [Crossref] [PubMed]
- Sato Y, Ogino H, Hara M, et al. Embolization of collateral vessels using mechanically detachable coils in young children with congenital heart disease. Cardiovasc Intervent Radiol 2003;26:528-33. [Crossref] [PubMed]
- Reidy JF, Jones OD, Tynan MJ, et al. Embolisation procedures in congenital heart disease. Br Heart J 1985;54:184-92. [Crossref] [PubMed]
- Pedra CA, Sousa LN, Pilla CB. A new use for the amplatzer duct occluder device. Arq Bras Cardiol 2002;78:315-21. [Crossref] [PubMed]
- Bilbao JI, Martinez-Cuesta A, Urtasun F, et al. Complications of embolization. Semin Intervent Radiol 2006;23:126-42. [Crossref] [PubMed]
- Kanter KR, Vincent RN. Management of aortopulmonary collateral arteries in Fontan patients: occlusion improves clinical outcome. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu 2002;5:48-54. [Crossref] [PubMed]


