Mortality after percutaneous edge-to-edge mitral valve repair: a contemporary review
Introduction
Mitral regurgitation (MR) is the second most common valvular disease after aortic stenosis. Without intervention, patients with symptomatic MR have reduced survivability despite optimal medical therapy (1-3). In patients with either symptomatic-, or asymptomatic (provided diagnostics show signs of developing left-sided heart failure) degenerative mitral regurgitation (DMR) the gold standard treatment is mitral valve (MV) repair. For functional mitral regurgitation (FMR) the indication for surgical treatment is less well-established due to the etiologic nature of this disease. In the latter, surgery is mainly limited to patients who will also benefit from coronary artery bypass grafting (4-6). Nevertheless, reports show that approximately half of the population with an indication for surgery, are being denied this treatment because of high-surgical-risk factors like advanced age, co-morbidities or reduced left ventricular (LV) function (7,8).
For these patients, percutaneous techniques may be an alternative therapy. Currently, the device with the widest clinical use is the MitraClip® (MC) (Abbot Vascular, Santa Clara, California, USA). The MC is a percutaneous transcatheter device for MV repair. The technique used mimics the surgical edge-to-edge Alfieri technique (9) through mechanical cooptation of the MV leaflets. Short-term effectiveness and safety of this percutaneous device have already been proved in both high- and low-risk patient groups (10-16). Considering short-term mortality, we know that patients treated with the MC are not at a disadvantage (13,17,18). However, since the MC is still a relative novelty, long-term survival results remain largely unknown. The goal of this review is to present an overview of the current literature about mortality and predictors for mortality in regard to the MC procedure.
Review
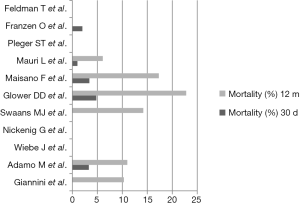
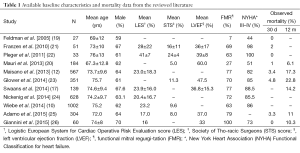
The Endovascular Valve Edge-to-Edge Repair Study I (EVEREST), which was conducted in 2004 (19), demonstrated the safety, feasibility and significant hemodynamic improvement of the MC. The EVEREST II (20), a multicenter and to date the only randomized controlled trial (RCT) on this topic, compared the safety and efficacy of MC to conventional MV surgery (either replacement or repair) among patients with severe MR (grade ≥3+). All included patients were potential candidates (selected by the guideline criteria) for MV surgery and were relatively low-risk patients [mean left ventricular ejection fraction (LVEF)] of 60%±10% and mean Society of Thoracic Surgeons (STS) score of 5%±4%) (Table 1). In total, 279 patients with a mean age of 67 years were randomized in a 2:1 ratio (MC: surgery) with FMR being present in only 27%. Mortality rate was 6.1% at 1 year and 17.4% at 4 years (Figure 1), which was not significantly different from the surgical group. The safety was superior in the MC group compared to the surgery group, with a significant higher need for blood transfusion in the latter.
Full table
Franzen et al. studied a group of 51 patients differed much from the EVEREST II by the cohort being older (mean age 73±10 years), having a worse LV function (mean LVEF of 36%±17%), and by having more comorbidities (mean STS score of 16%±11%). FMR was present in 69% of the cohort. They showed feasibility with a high implantation success of 96% (n=49) and a low 30-day mortality of 2% (n=1), the deceased concerning an 84-year-old male with a LVEF of 14% and a Logistic EuroSCORE (LES) of 86% (21).
Based on those data the guidelines on valvular heart disease of the European Society of Cardiology (ESC, 2012) added catheter-based interventions to correct MR. Mitraclipping may be considered in patients with symptomatic severe MR who fulfil the transesophageal echocardiographic criteria of eligibility, who are judged to be inoperable or at high-surgical-risk by a team of cardiologists and cardiac surgeons, and who have a life expectancy greater than 1 year (recommendation class IIb, level of evidence C) (4).
Several medium- and large-sized European registries have added to the evidence of safety and efficacy of the MC. Although being non-randomized, these were conducted in a real-world setting, presenting mortality figures of the MC in today’s practice.
The ACCESS-EU registry, in which 567 patients (mean age 73.4±10 years) were prospectively enrolled at 14 European sites, FMR was present in 77%. A LVEF ≤40% was present in 53% and the mean LES score was 23±18. They reported a 30-day mortality and an estimated 12-month mortality of 3.4% and 18.2%, respectively (12). A large European sentinel registry enrolled 628 patients between 2011 and 2012 at 25 centers (mean age 74±10 years). The cohort consisted predominantly of FMR (72%), there was a mean LVEF of 43%±16% and a high mean LES score of 20%±17%. They presented a 2.9% mortality at 30 days and 15.3% at 12 months. There was no significant difference in mortality between DMR and FMR (24). More recent publications of German and Italian registries, with 1,002 and 304 patients respectively, show similar short-term results, with in-hospital and 30-day mortality rates of 2.9% and 3.3% respectively (10,25).
The EVEREST II high-risk registry (HRR), which enrolled 78 patients between 2007 and 2008, and the ongoing EVEREST II REALISM (Real World Expanded Multicenter Study of the MC System) high-risk arm included 351 symptomatic elderly patients (mean age 76±11 years), with significant MR (70% FMR), of whom 60% had a history of cardiac surgery (23). This represents a population with more severe comorbidities (mean STS score of 11%±8%) and worse LV function (mean LVEF of 48%±14%). One-year mortality was 22.8%.
Pleger et al. described 51 very high-risk patients (mean LES score 41%±7%) and analyzed the cohort for effectiveness and safety. They observed one death of a patient (LES score of 63%) who died 31 days post-procedural (22). More recently and being comprised of a larger pool, patients from the TRAMI registry were reviewed for age and mortality. In total, 525 patients with an age of ≥76 years (mean 81±3 years) showed an in-hospital and 30-day mortality of 2.9% and 6.7%, respectively. There was no significant difference compared to the 539 patients of the cohort with an age <76 years. Also, the multivariate analysis did not point out advanced age as a predictor for in-hospital major adverse cardiac events (27).
To address this need to compare the MC to alternative treatment options, especially for high-risk patients, Swaans et al. retrospectively formed conservatively and surgically treated matched control groups. To try correct for confounding factors, propensity scoring was used to correct for cardiac resynchronization and LES score among others. MC patients mainly had FMR (77%), mean age was 75±9 years, there was a mean LES score of 24%±16% and a mean LVEF of 37%±15%. The median follow up for the MC group was 1.7±1.1 years, and mortality after 1, 2 and 3 years was 14.2%, 24.5% and 37.7% respectively. The conservatively treated cohort (age 72±10 years, mean LES 19%±13% and mean LVEF of 19%±13%) had a median follow up of 2.7±2.2 years and a mortality ratio of 32.3%, 47.5% and 54.2% after 1, 2 and 3 years follow up, respectively.
When comparing MC treatment with conservative treatment, the hazard ratio (HR) for mortality was 0.41 [95% confidence interval (CI): 0.22–0.78, P=0.006]. After propensity matching, the outcome remained comparable with a HR of 0.47 (95% CI: 0.24–0.93). In a sub-analysis of patients with FMR the HR for mortality also remained significant (HR 0.46, 95% CI: 0.23–0.93, P=0.03). The HR for mortality for percutaneously treated patients compared with surgically treated patients, showed no significant difference. The limitation of this study lies in its non-randomized retrospective character, which could potentially give rise to patient selection bias and to the inclusion of unknown confounding factors (17).
More recently, a study by Velazquez et al. used similar methodology and data from the HRR and REALISM and the Duke Echocardiography Laboratory Database (28) to perform a propensity matched comparison between MR patients treated with the MC (mean age 74±11 years, mean LVEF 42%±12%) and medically treated patients. Also recently, an online publication by Giannini et al. compared conservative to percutaneous edge-to-edge (mean age 74±8 years, mean LVEF 33 years) treatment for patients with FMR. Both, in line with Swaans et al., showed significant lower mortality rates at follow up for MC treatment compared to conservative treatment, with adjusted HR’s for mortality being 0.60 (95% CI: 0.42–0.85) and 0.43 (95% CI: 0.24–0.77) for Velazquez et al. and Giannini et al., respectively (26,29).
In order to obtain a higher level of evidence, a RCT is required. Several RCT’s have been set up over the past few years. In 2013 the study protocol of A Randomized Study of the MitraClip Device in Heart Failure Patients with Clinically Significant Functional Mitral Regurgitation (RESHAPE-HF) was registered. In this European RCT, percutaneous intervention and conservative treatment will be compared by investigating mortality and re-hospitalization differences. Unfortunately, due to low recruitment rate, this study has been terminated prematurely (ClinicalTrials.gov number, NCT01772108). Currently, the Cardiovascular Outcomes Assessment of the MC Percutaneous Therapy (COAPT) for Heart Failure Patients With Functional Mitral Regurgitation trial is recruiting patients in the USA and Canada to either undergo MC (n=215) or conservative treatment (n=215). The target date for analysis of primary outcome, of which the safety outcome is a combined endpoint of several major complications and the effectiveness outcome being recurrent heart failure hospitalizations, is scheduled for early 2018 (ClinicalTrials.gov number, NCT01626079). Other similar RCT’s have been introduced, but until now there have been no published results (ClinicalTrials.gov numbers, NCT01431222 and NCT01920698). Recently, A Multicenter Randomized Controlled Study to Assess Mitral vAlve reconsTrucTion for advancEd Insufficiency of Functional or iscHemic ORigiN (MATTERHORN) was started. It is the first study which compares MV surgery and MC treatment in patients with depressed LV function and investigators intend to include 210 patients to be divided over the two study arms (ClinicalTrials.gov number, NCT02371512).
To further help treating physicians in deciding which high-risk patients will benefit most from MC treatment, the relation between pre- or peri-procedural characteristics and post-procedural mortality should be studied. Several performed analyses have shown acute procedural success, defined as MR reduction to ≤2 (≤ mild), to have a positive impact on survival (18,30-34). An univariate analysis of an early conducted [2009–2012] observational study in Switzerland, with 77 patients who had reached a follow-up of 2 years (mean age 72±12 years, mean LES score 21%±17%), also resulted in NT-proBNP, chronic obstructive pulmonary disease and kidney failure to be predictors for mortality (31). In a more recent study of 84 patients, the multivariate analysis showed NT-proBNP, previous valve surgery and tricuspid insufficiency to be independent mortality predictors during a follow up of 2 years (33). Advanced age, New York Heart Association (NYHA) III–IV, STS score ≥12, pulmonary hypertension, MR of ischemic heart disease and pre-procedural MR-grade have also all been proved to be predictors for mortality (18,27,32,34,35).
Synopsis
Percutaneous edge-to-edge MV repair with the MC® has proved to have a relatively low peri-procedural mortality rate in both patients with a low- or high-surgical-risk. In contrast to surgery, it seems to be a safe alternative for the frail patient. Though three non-randomized studies suggested a survival benefit of MV repair using the MC compared to conservative management, this finding awaits confirmation in a RCT with adequate length follow-up.
Acknowledgements
None.
Footnote
Conflicts of Interest: Dr. JA van der Heyden and Dr. MJ Swaans are proctors for Abbott Vascular. The other authors have no conflicts of interest to declare.
References
- Iung B, Baron G, Butchart EG, et al. A prospective survey of patients with valvular heart dis-ease in Europe: The Euro Heart Survey on Valvular Heart Disease. Eur Heart J 2003;24:1231-43. [Crossref] [PubMed]
- Trichon BH, Felker GM, Shaw LK, et al. Relation of frequency and severity of mitral regurgi-tation to survival among patients with left ventricular systolic dysfunction and heart failure. Am J Cardiol 2003;91:538-43. [Crossref] [PubMed]
- Agricola E, Ielasi A, Oppizzi M, et al. Long-term prognosis of medically treated patients with functional mitral regurgitation and left ventricular dysfunction. Eur J Heart Fail 2009;11:581-7. [Crossref] [PubMed]
- Vahanian A, Alfieri O, Andreotti F, et al. Guidelines on the management of valvular heart dis-ease (version 2012): the Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Sur-gery (EACTS). Eur J Cardiothorac Surg 2012;42:S1-44. [Crossref] [PubMed]
- Philip F, Athappan G, Tuzcu EM, et al. MitraClip for severe symptomatic mitral regurgitation in patients at high surgical risk: a comprehensive systematic review. Catheter Cardiovasc Interv 2014;84:581-90. [Crossref] [PubMed]
- McGee EC, Gillinov AM, Blackstone EH, et al. Recurrent mitral regurgitation after annuloplas-ty for functional ischemic mitral regurgitation. J Thorac Cardiovasc Surg 2004;128:916-24. [Crossref] [PubMed]
- Carabello BA. The current therapy for mitral regurgitation. J Am Coll Cardiol 2008;52:319-26. [Crossref] [PubMed]
- Mirabel M, Iung B, Baron G, et al. What are the characteristics of patients with severe, symp-tomatic, mitral regurgitation who are denied surgery? Eur Heart J 2007;28:1358-65. [Crossref] [PubMed]
- Alfieri O, Maisano F, De Bonis M, et al. The double-orifice technique in mitral valve repair: a simple solution for complex problems. J Thorac Cardiovasc Surg 2001;122:674-81. [Crossref] [PubMed]
- Wiebe J, Franke J, Lubos E, et al. Percutaneous mitral valve repair with the MitraClip system according to the predicted risk by the logistic EuroSCORE: preliminary results from the Ger-man Transcatheter Mitral Valve Interventions (TRAMI) Registry. Catheter Cardiovasc Interv 2014;84:591-8. [Crossref] [PubMed]
- Feldman T, Foster E, Glower DD, et al. Percutaneous repair or surgery for mitral regurgitation. N Engl J Med 2011;364:1395-406. [Crossref] [PubMed]
- Maisano F, Franzen O, Baldus S, et al. Percutaneous mitral valve interventions in the real world: early and 1-year results from the ACCESS-EU, a prospective, multicenter, nonrandom-ized post-approval study of the MitraClip therapy in Europe. J Am Coll Cardiol 2013;62:1052-61. [Crossref] [PubMed]
- Van den Branden BJ, Swaans MJ, Post MC, et al. Percutaneous edge-to-edge mitral valve re-pair in high-surgical-risk patients: do we hit the target? JACC Cardiovasc Interv 2012;5:105-11. [Crossref] [PubMed]
- Auricchio A, Schillinger W, Meyer S, et al. Correction of mitral regurgitation in nonresponders to cardiac resynchronization therapy by MitraClip improves symptoms and promotes reverse remodeling. J Am Coll Cardiol 2011;58:2183-9. [Crossref] [PubMed]
- Franzen O, van der Heyden J, Baldus S, et al. MitraClip® therapy in patients with end-stage systolic heart failure. Eur J Heart Fail 2011;13:569-76. [Crossref] [PubMed]
- Paranskaya L, D'Ancona G, Bozdag-Turan I, et al. Residual mitral valve regurgitation after percutaneous mitral valve repair with the MitraClip® system is a risk factor for adverse one-year outcome. Catheter Cardiovasc Interv 2013;81:609-17. [Crossref] [PubMed]
- Swaans MJ, Bakker AL, Alipour A, et al. Survival of transcatheter mitral valve repair compared with surgical and conservative treatment in high-surgical-risk patients. JACC Cardiovasc Interv 2014;7:875-81. [Crossref] [PubMed]
- Triantafyllis AS, Kortlandt F, Bakker AL, et al. Long-term survival and preprocedural predic-tors of mortality in high surgical risk patients undergoing percutaneous mitral valve repair. Catheter Cardiovasc Interv 2016;87:467-75. [Crossref] [PubMed]
- Feldman T, Wasserman HS, Herrmann HC, et al. Percutaneous mitral valve repair using the edge-to-edge technique: six-month results of the EVEREST Phase I Clinical Trial. J Am Coll Cardiol 2005;46:2134-40. [Crossref] [PubMed]
- Mauri L, Foster E, Glower DD, et al. 4-year results of a randomized controlled trial of percuta-neous repair versus surgery for mitral regurgitation. J Am Coll Cardiol 2013;62:317-28. [Crossref] [PubMed]
- Franzen O, Baldus S, Rudolph V, et al. Acute outcomes of MitraClip therapy for mitral regur-gitation in high-surgical-risk patients: emphasis on adverse valve morphology and severe left ventricular dysfunction. Eur Heart J 2010;31:1373-81. [Crossref] [PubMed]
- Pleger ST, Mereles D, Schulz-Schönhagen M, et al. Acute safety and 30-day outcome after percutaneous edge-to-edge repair of mitral regurgitation in very high-risk patients. Am J Cardiol 2011;108:1478-82. [Crossref] [PubMed]
- Glower DD, Kar S, Trento A, et al. Percutaneous mitral valve repair for mitral regurgitation in high-risk patients: results of the EVEREST II study. J Am Coll Cardiol 2014;64:172-81. [Crossref] [PubMed]
- Nickenig G, Estevez-Loureiro R, Franzen O, et al. Percutaneous mitral valve edge-to-edge re-pair: in-hospital results and 1-year follow-up of 628 patients of the 2011-2012 Pilot European Sentinel Registry. J Am Coll Cardiol 2014;64:875-84. [Crossref] [PubMed]
- Adamo M, Capodanno D, Cannata S, et al. Comparison of three contemporary surgical scores for predicting all-cause mortality of patients undergoing percutaneous mitral valve repair with the MitraClip system (from the multicenter GRASP-IT registry). Am J Cardiol 2015;115:107-12. [Crossref] [PubMed]
- Giannini C, Fiorelli F, De Carlo M, et al. Comparison of Percutaneous Mitral Valve Repair Versus Conservative Treatment in Severe Functional Mitral Regurgitation. Am J Cardiol 2016;117:271-7. [Crossref] [PubMed]
- Schillinger W, Hünlich M, Baldus S, et al. Acute outcomes after MitraClip therapy in highly aged patients: results from the German TRAnscatheter Mitral valve Interventions (TRAMI) Registry. EuroIntervention 2013;9:84-90. [Crossref] [PubMed]
- Rosati RA, McNeer JF, Starmer CF, et al. A new information system for medical practice. Arch Intern Med 1975;135:1017-24. [Crossref] [PubMed]
- Velazquez EJ, Samad Z, Al-Khalidi HR, et al. The MitraClip and survival in patients with mi-tral regurgitation at high risk for surgery: A propensity-matched comparison. Am Heart J 2015;170:1050-1059.e3. [Crossref] [PubMed]
- Sürder D, Pedrazzini G, Gaemperli O, et al. Predictors for efficacy of percutaneous mitral valve repair using the MitraClip system: the results of the MitraSwiss registry. Heart 2013;99:1034-40. [Crossref] [PubMed]
- Toggweiler S, Zuber M, Sürder D, et al. Two-year outcomes after percutaneous mitral valve repair with the MitraClip system: durability of the procedure and predictors of outcome. Open Heart 2014;1:e000056. [Crossref] [PubMed]
- Puls M, Tichelbäcker T, Bleckmann A, et al. Failure of acute procedural success predicts ad-verse outcome after percutaneous edge-to-edge mitral valve repair with MitraClip. EuroIntervention 2014;9:1407-17. [Crossref] [PubMed]
- Boerlage-vanDijk K, Wiegerinck EM, Araki M, et al. Predictors of outcome in patients under-going MitraClip implantation: An aid to improve patient selection. Int J Cardiol 2015;189:238-43. [Crossref] [PubMed]
- Capodanno D, Adamo M, Barbanti M, et al. Predictors of clinical outcomes after edge-to-edge percutaneous mitral valve repair. Am Heart J 2015;170:187-95. [Crossref] [PubMed]
- Matsumoto T, Nakamura M, Yeow WL, et al. Impact of pulmonary hypertension on outcomes in patients with functional mitral regurgitation undergoing percutaneous edge-to-edge repair. Am J Cardiol 2014;114:1735-9. [Crossref] [PubMed]