
The need for custom made frozen elephant trunk: when and where
Introduction
The frozen elephant trunk (FET) technique has become an effective option to treat both elective and emergency complex aortic conditions when the arch and the proximal tract of the descending thoracic aorta (DTA) are interested by the pathologic process (1). This surgical approach changes the conventional elephant trunk from a two-stage to a single stage procedure which allows to entirely replace the aortic arch with a surgical prosthesis which has got a distal stented portion deployed into the aortic arch and the proximal DTA (2-4). Recent studies have demonstrated that patients undergone to total arch replacement with the FET technique show a decreased incidence of aortic re-operations with improved long-term outcomes at follow up (5). Among the available hybrid prostheses, we have mainly used Thoraflex hybrid (Terumo Aortic, Scotland) which is a vascular device properly designed to facilitate the FET technique when a total arch replacement with single reimplantation of supra-aortic trunk (SAT) is employed by the surgical team. This prosthesis has a distal endovascular nitinol ringed stent-graft connected to a proximal 4-branched surgical graft. We have already reported the results of our initial experience with FET technique using a conventional Thoraflex hybrid prosthesis (6). The concept of a new Custom Thoraflex hybrid comes from our single centre experience of about 150 FET operations with conventional Thoraflex hybrid to treat equally acute and chronic complex aortic disease involving the aortic arch and DTA. The aim of the new device is to solve the technical pitfalls we have faced in our practise, such as reimplantation of the SAT vessels, especially the left common carotid (LCCA) and left subclavian (LSA) arteries, their chest placement, and optimal control of cerebral perfusion during circulatory arrest time. To sort this, we have requested a custom-made design of Thoraflex hybrid and our first experience with the initial version of a custom device has been already described (Figure 1): a conventional 28/30 mm diameter, 100 mm stent length Thoraflex Hybrid was changed to have only two branches: a main one (16 mm) for SAT reimplantation, and a lateral one (10 mm) for systemic perfusion. A separate trifurcated Gelweave™ surgical graft (10/8/8–16 mm) (Terumo Aortic) with a 10-mm side perfusion branch was used to connect the SAT vessels (7). Since then, several modifications have been proposed and here we present the new Custom Thoraflex hybrid with its implantation technique and the potential advantages compared to the conventional prosthesis.
Thoraflex hybrid FET graft
The Thoraflex hybrid is a novel graft designed for aortic arch surgery, which consists of a proximal tubular gelatin coated Dacron graft and a distal polyester made stent graft supported by self-expandable nitinol skeleton. The device can be directly deployed into the aortic arch and proximal DTA during circulatory arrest when the aortic arch is opened. The unstented part has a different calibre if compared to the stented part, so it can fit to the sinus-tubular junction, and has four side branches: three for the restoration of supra-aortic vessels and one for systemic perfusion. Between the two portions there is a collar which facilitates the distal anastomosis and improves hemostasis. The Thoraflex hybrid comes in different sizes; the proximal part diameters vary from 26 to 32 mm, the stented part from 26 to 40 mm. Two different distal lengths are available (100 and 150 mm). The combination of the various sizes and length allow to tailorize the graft to the patient’s anatomy.
Custom Thoraflex hybrid design and size selection
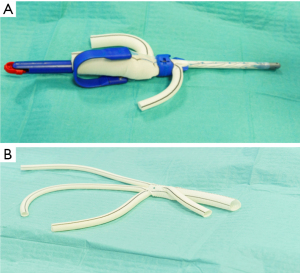
In the actual configuration, our custom Thoraflex hybrid consists of a conventional Thoraflex hybrid with a stent length of 100 mm which is revised to have only two branches: a main one (16 mm diameter) which four folds into four branches (12/8/10 mm diameter branches for SAT reimplantation and 10 mm branch for cerebral perfusion) and a 10-mm side branch for systemic perfusion (Figure 2). Once opened on the operative field, the main branch is initially separated from the device to allow the completion of the procedure (Figure 3). The main targets are to improve the cerebral perfusion throughout the surgical procedure, to facilitate the correct sizing and trimming of the vascular branches and to reduce the anterior mediastinal encumbrance of the neo-trunk branch vessels thus facilitating sternal closure at the end of the procedure.


The selection of the stented graft size is established by an accurate evaluation of the preoperative CT angiogram of the aorta and comes mainly from the measurement of the aortic diameter of the stented graft landing zone. In case of acute and chronic aortic dissection, no oversizing is performed, whether in case of ascending aorta and/or arch aneurysm, especially if a second surgical treatment is predicted, the size is accorded to the maximum diameter of the thoracic aorta allowing 10–15% of oversize. To reduce the risk of paraplegia, we merely use the 100 mm length so that a shorter tract of the DTA is covered by the stented graft.
Surgical technique
Our peculiar “debranching first” implantation technique has been already described in previous reports (6,7). Transesophageal echocardiography (TEE) and continuous bilateral cerebral oximetry are employed in the entire cohort of our patients.
The conventional mid sternotomy incision is routinely extended in a small bilateral supra-clavicular neck incision to better expose the epiaortic vessels. Right subclavian artery (isolated from anterior mediastinum) or right axillary artery (isolated in the right sub clavicular region) are typically used as arterial site for central cannulation, normally with interposition of a vascular graft (8 or 10 mm, according to the native artery diameter) to prevent direct cannulation of the artery. One of the key aspects of our surgical technique remains a homemade 3-branched perfusion circuit which is used for cardiopulmonary bypass (CPB) and for the selective antegrade cerebral perfusion during moderate hypothermic circulatory arrest. Three branches of equal diameter allow systemic perfusion by a single pump while connected to right subclavian artery and the two side branches of the custom Thoraflex. During CPB time, the perfusion is maintained at theoretical full flow, which is calculated considering body surface area, and deployed to the peripheral organs based on physiological systemic resistance. Once the circulatory arrest begins, the flow is reduced to 10–15 mL/kg/min for selective antegrade cerebral perfusion.
During the initial cooling phase, while the heart is still perfused and beating, LCCA and LSA are isolated, resected and anastomosed to the two dedicated side branches of the vascular prosthesis; cannulation and perfusion of the graft’s cerebral perfusion side branch allows complete trivascular antegrade cerebral perfusion throughout the circulatory arrest time of the operation.
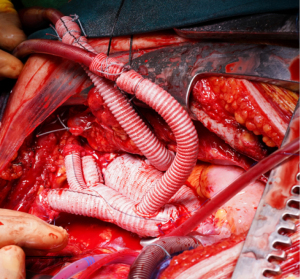
When debranching of arch vessels is completed, the ascending aorta is cross-clamped, opened and cardioplegia administered. Aortic valve and root surgery is then performed as required by the case depending on the primary disease. Once the body temperature is lowered to 28 ℃, the innominate artery is clamped, circulatory arrest stars and selective trivascular antegrade cerebral perfusion begins at 10–15 mL/kg/min. The arch is then opened and the landing zone (normally in zone 2 of the arch) is strengthened with internal and external teflon strips. The stented part of the graft is released in the DTA and its collar is sewed to the arch. At this stage, a systemic visceral perfusion (max 1,200 mL/min flow) is started after cannulation of the side branch dedicated to systemic perfusion. Once the collar suture is completed, systemic full flow is recommenced, and rewarming started. The proximal anastomosis is then finalized, and aortic cross-clamp removed. The innominate artery is now anastomosed to the dedicated branch of the SAT prosthesis. Finally, the main bodies of the FET and the SAT vascular branch of the device are anastomosed back together (Figure 4).
Discussion
Nowadays in several institutions the FET technique is becoming the gold standard for treatment of complex aortic disease. Since 2018, Thoraflex Hybrid has become our favourite FET device mainly due to the benefits of the plexus configuration; however, in a few cases, it is not obvious to decide which is the most appropriate graft’s length, thus theoretically increasing the risk of redundant or kinked branch vessels leading to reduced blood flow to the brain. This problem is particularly significant in small size chest where the space for a correct alignment of the neo-trunks is fewer and sternal closure could represent a challenge because of the encumbrance due to the FET device and its vascular branches.
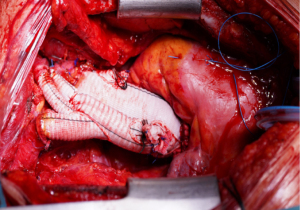
The custom Thoraflex hybrid, as it is at present, is an updated version of the first custom Thoraflex hybrid. The main difference is in the relationship between the side branches of the four-fold vascular graft which, at present, comes attached to the main body of the graft. There is a specific angle of take-off for each of the vascular branch and a precise distance between the four branches which favours the correct alignment of the neo-trunks. In the actual configuration, the custom Thoraflex hybrid can be potentially used in all the patients requiring complex aortic arch surgery and a FET procedure. We believe that this solution should be available on the shelf in all aortic centres and ready to be used according to the case. It does not require a different learning curve for the operating surgeon as it represents just an evolution of the well-known Thoraflex hybrid device. By adopting our device modification, the graft used for SAT debranching can be easily handled and a direct end-to-end anastomosis is made while perfusing the vessels via the side branch. Incomplete cerebral perfusion is reduced to the moment of LCCA anastomosis. Interestingly, with our custom design, the vessels’ length is more accurate and the position of the neo-vessels in the chest prevents mispositioning and/or kinking and facilitates sternal closure (Figure 5). Another important aspect to underline is the possibility with this device to perform an easier distal anastomosis more proximally on the arch, such as in zone 0 or 1.
More data about short- and long-term outcomes will be available in the future once the number of patients treated with the custom device will increase.
Conclusions
A variation to the basic Thoraflex hybrid design allows full and continuous cerebral trivascular perfusion during the circulatory arrest time of FET procedures, facilitating correct positioning of the intrathoracic vessels and sternal closure by reducing anterior mediastinal encumbrance.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Mohamad Bashir, Edward P. Chen and Mohammed Idhrees) for the series “Frozen Elephant Trunk” published in Cardiovascular Diagnosis and Therapy. The article has undergone external peer review.
Peer Review File: Available at https://cdt.amegroups.com/article/view/10.21037/cdt-22-191/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://cdt.amegroups.com/article/view/10.21037/cdt-22-191/coif). The series “Frozen Elephant Trunk” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Tsagakis K, Wendt D, Dimitriou AM, et al. The frozen elephant trunk treatment is the operation of choice for all kinds of arch disease. J Cardiovasc Surg (Torino) 2018;59:540-6. [Crossref] [PubMed]
- Roselli EE, Rafael A, Soltesz EG, et al. Simplified frozen elephant trunk repair for acute DeBakey type I dissection. J Thorac Cardiovasc Surg 2013;145:S197-201. [Crossref] [PubMed]
- Shrestha M, Bachet J, Bavaria J, et al. Current status and recommendations for use of the frozen elephant trunk technique: a position paper by the Vascular Domain of EACTS. Eur J Cardiothorac Surg 2015;47:759-69. [Crossref] [PubMed]
- Beckmann E, Martens A, Korte W, et al. Open total arch replacement with trifurcated graft and frozen elephant trunk. Ann Cardiothorac Surg 2020;9:170-7. [Crossref] [PubMed]
- Di Eusanio M, Petridis FD, Pacini D, et al. Facilitated aortic arch repair with the frozen elephant trunk technique. Eur J Cardiothorac Surg 2011;40:1261-2. [Crossref] [PubMed]
- Masiello P, Mastrogiovanni G, Presutto O, et al. Frozen elephant trunk procedure for complex aortic arch surgery: The Salerno experience with Thoraflex hybrid. J Card Surg 2022;37:107-14. [Crossref] [PubMed]
- Masiello P, Mastrogiovanni G, Chivasso P, et al. A modified frozen elephant trunk hybrid device to facilitate supra-aortic trunk anastomosis. J Card Surg 2021;36:371-3. [Crossref] [PubMed]


