Fractional flow reserve application in everyday practice: adherence to clinical recommendations
Introduction
Currently, fractional flow reserve (FFR) is considered the gold standard for invasive assessment of functional significant coronary stenosis (1-3). The FFR provides a well defined cut-off value for deciding whether to revascularize immediately or to defer intervention. The cut-off includes a narrow “grey zone” (0.75-0.8) (4); thus, stenosis with FFR ≤0.75 are associated with inducible myocardial ischemia, with accuracy above 90% (5-8).
Over the last decade, several studies have investigated methods for identifying patients that might benefit from FFR-guided percutaneous coronary angiography (PCI) including stable patients that elected treatment for single-vessel coronary artery disease (9-12), multi-vessel coronary artery disease (13,14), equivocal left main coronary artery lesions, or bifurcation lesions (15-20). FFR has also been validated for patients with acute myocardial infarction (MI) or unstable angina (21,22).
In routine clinical practice, a substantial proportion of patients undergo coronary angiography without a prior non-invasive, functional evaluation. Traditionally, operators have been trained to assess coronary stenosis with an angiogram, and they base their decisions on a visual assessment, quantitative coronary angiographic (QCA) measurement, and their clinical judgment. Therefore, the incorporation of FFR into daily practice for decision making would require a change in the “mind-set”, and it would also be time-consuming.
The aim of the present study was to evaluate the routine use of FFR in daily clinical practice. We investigated the clinicians’ adherence to FFR guidelines and the effect of FFR analysis on long term outcomes.
Methods
Study design and population
We performed a single-center, retrospective, cohort investigation of all patients that underwent a FFR evaluation during coronary angiography until December 2011, in the Rabin Medical Center.
The study population included all consecutive patients that exhibited an equivocal stenosis during angiography; had received an FFR measurement to determine the need for revascularization; and had completed at least a 6-month clinical follow-up, which was recorded and available. The decision of whether to perform the FFR and the choice of management afterwards were determined by the operator.
The study population comprised patients that had elected treatment and patients hospitalized for treatment after a diagnosis of stable coronary disease, unstable coronary disease, or acute MI. Stable angina was defined as chest pain on exertion with a stable pattern for at least 6 months preceding admission. Unstable angina was defined according to the Braunwald classification (23). MI, ST elevation MI (STEMI) and non-ST elevation MI (NSTEMI), were defined according to the universal definition of MI (24).
In patients with multi-vessel coronary disease, we reported the results and outcome of the lesions which required FFR measurement, regardless to the treatment of the non-equivocal lesions.
Demographics, baseline characteristics, clinical presentation, coronary distribution, treatment modality, in-hospital outcome, and long-term outcome were determined by medical records and angiographic reviews, and when necessary, in a telephone follow-up.
Coronary angiography
Diagnostic left heart catheterization and coronary angiography were performed with a standard percutaneous approach from either the femoral or radial artery. The severity of the coronary lesion was assessed by the operator, based on the angiogram. Retrospectively, we performed offline, QCA calculations with the Medcon analysis software (Horizon Cardiology version 12.2 Hot Fix 2, McKesson Israel LTD. Tel-Aviv, Israel). All QCA measurements were performed by an independent observer that was blinded to patient clinical outcome and FFR data.
The radiopaque catheter was used for calibration. The obstructive diameter, reference diameter, and lesion length were measured, preferably, on end-diastolic images. The lesion segment was defined as proximal, middle, or distal.
FFR measurements
FFR measurements were performed for all lesions that had been judged equivocal by the operator at the time of coronary angiography. FFR results reported in case of acute MI relays to the culprit artery. Decision-making for revascularization was undertaken by the operator, and the decisions were based on his/her clinical judgment, in consideration of the FFR results, but not necessarily in concordance with the FFR results.
After intravenous (IV) administration of heparin at a dose of 50 IU/kg, a pressure monitoring guidewire (PrimeWire-Prestige, Volcano Corporation, San Diego, CA, USA) was calibrated and introduced into the guiding catheter. The wire was advanced up to the tip of the guiding catheter, where the arterial blood pressure was checked to ensure the pressure detected with wire was equal to the pressure measured through the guiding catheter. Subsequently, the pressure wire was advanced further into the target coronary artery, until the pressure sensor was located just distal to the lesion segment. Then, maximal myocardial hyperemia was induced by infusing escalating doses of adenosine through the guiding catheter until steady-state hyperemia was achieved. During maximal hyperemia, FFR was calculated as the ratio between the simultaneously recorded mean aortic pressure and mean coronary artery pressure. Significant FFR was defined as ≤0.80 (1).
Follow up and clinical outcome
Clinical outcomes included all-cause mortality, cardiac mortality, and major adverse cardiac events (MACE). MACE was defined as a hierarchal, composite end-point that comprised cardiac mortality, non-fatal MI, target vessel revascularization, and coronary artery bypass graft (CABG). Clinical outcomes were evaluated at 6-month, one-year, and two-year follow ups by reviewing medical records, clinical visits, and hospitalizations. When necessary, patients or their general practitioners were contacted by phone for additional information. The follow-up was terminated either when the patient died or at the end of the follow-up period (July 31, 2012).
Statistical analysis
Continuous data are reported in terms of the mean (range), and differences between groups were tested with the unpaired Student’s t test. Categorical data are presented as the number and percentage, and differences between groups were tested using Fisher’s exact test. Survival curves and life tables were constructed according to the Kaplan-Meier method with Log-Rank analysis for significance. A P-value <0.05 was considered statistically significant. All tests were two-tailed.
Results
We identified 189 patients (mean age 62.5±11.3 years, men 80.4%) who underwent FFR measurements for equivocal lesions during coronary angiography. All patients had complete data regarding the FFR, coronary angiography results, and clinical outcomes. The median follow up period was 27 months (range, 7-112 months).
Baseline clinical characteristics, angiographic results, and functional measurements
Baseline clinical and angiographic characteristics are depicted in Table 1. The clinical presentations were diverse, including unstable angina (74.6%), stable angina (16.9%), and acute MI (8.5%). A large number of patients (40.2%) had performed noninvasive stress testing prior to angiography. Multi-vessel coronary disease, was present in 102 patients (53.9%), and bifurcation lesions in 18 patients (9.5%).
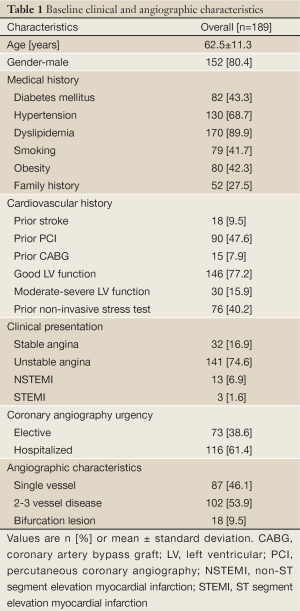
Full Table
According to the angiographic visual assessment (i.e., visual estimation by the operator), nearly half the patients (49.7%) had intermediate stenosis (51-70% stenosis); 12.7% had significant stenosis (>70%) and 37.6% had non-significant stenosis (<50% stenosis) (Table 2).
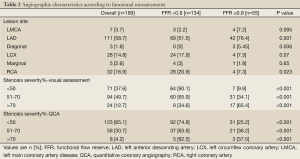
Full Table
Non-significant FFRs (>0.8) were found in 134 patients (70.9%); significant FFRs (≤0.8) were found in only 55 patients (29.1%). An intervention (PCI or CABG) was performed in 36% of patients; the remaining patients were managed conservatively with the best attempted medical treatment. Interestingly, despite a FFR finding of functionally non-significant stenosis, 24 out of 134 patients (17.9%) underwent revascularization (19 PCI and 5 CABG); conversely, despite a FFR finding of functionally significant stenosis, 11 out of 55 patients (20%) were deferred.
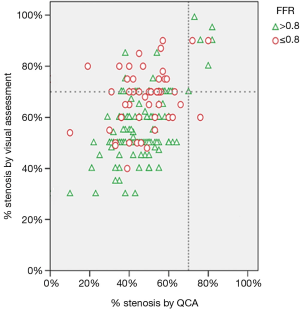
The visual stenosis estimate was validated with a calculated QCA, and both were compared to FFR measurements (Table 2). Lesion severity was frequently overestimated by the visual estimate compared to that estimated by the calculated QCA (Figure 1); however, both were poorly correlated with FFR measurements (Table 2).
Outcome
During a 2-year follow up period, the all-cause mortality rate was 4.9%, including 7 non-cardiac deaths and 1 cardiac death due to severe heart failure. Overall, 10 patients (8.5%) experienced a MACE during the two-year follow up period, including 1 cardiac mortality, 2 acute MI, 6 target lesion or vessel revascularizations, and 1 CABG. Most revascularizations were performed after one year of follow up. Patient’s description including stenosis severity, management strategy and adherence to FFR results is presented in Table 3.
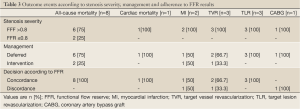
Full Table
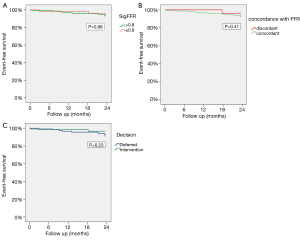
There was no significant difference in the overall MACE rates for those with significant and those with non-significant FFRs (8% vs. 10%, respectively, P=0.98; Figure 2). Patients deferred from revascularization tended to have higher overall MACE rates (including subsequent revascularizations) than those treated immediately. However, this difference did not reach statistical significance (11.7% vs. 3.4% respectively, P=0.23; Figure 2).
Outcome according to FFR adherence
Out of 189 patients, 35 (18.5%) were treated in discordance with the FFR results and guidelines; thus, 24 patients (17.9%) underwent revascularization, despite a non-significant FFR, and 11 patients (20%) were deferred from revascularization, despite a significant FFR.
For patients treated in discordance with the FFR indication, the mean FFR values were slightly above or below the reference cut-off value (“grey-zone”, Figure 3). Patients that underwent revascularization, despite a non-significant FFR, had a lower mean FFR than those deferred (0.86±0.49 vs. 0.88±0.53, P=0.023); patients that were deferred from revascularization, despite a significant FFR, had a higher mean FFR than those that underwent revascularization (0.76±0.43 vs. 0.73±0.68, P=0.036).
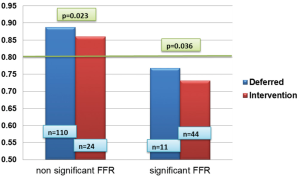
Evaluating the discordant cases, we have found that 19 out of 35 patients (54.3%) had an FFR around the cut off value (0.75-0.85). Only 2 patients who had FFR value of <0.75 were treated conservatively and 14 patients with FFR>0.85 underwent revascularization. For patients who underwent revascularization despite non-significant FFR, the decision was based on clinical judgment (5 patients), positive stress test (12 patients) and angiographic morphology of unstable plaque (4 patients). For 3 patients the concrete causes for the decision were missing. For patients treated conservatively despite significant FFR, the decision was based on clinical judgment (2 patients) and lesion complexity (3 patients). For 6 patients the concrete causes for the decision were missing. Only 1 patient was treated conservatively despite a positive stress test due to his oncological condition.
During a 2-year follow up period, there was no significant difference in the cumulative MACE rate, whether the patient was managed in concordance or discordance with FFR results and guidelines (Figure 2).
Discussion
This study had four main findings. First, a significant FFR (≤0.8) was found in approximately 30% of patients with equivocal lesions, and of those, 84% presented with acute coronary syndrome. Second, visual lesion estimates showed a tendency to overestimate lesion severity compared to the calculated QCA, but both were poorly correlated to functional stenosis measurements. Third, in approximately 20% of cases, the decision for revascularization was discordant with FFR-based recommendations. Also, indication for FFR measurement did not always follow the accepted guidelines (STEMI patients, <50% and >90% lesion severity). Forth, there was no significant difference in outcome between groups treated with or without revascularization, whether the treatment was in concordance or discordance with FFR-based recommendations.
Our study population was unique for its diversity in clinical presentations, which ranged from stable coronary disease to emergent acute MI. This diversity represented the “open door” policy in “real life” clinical medicine. In addition, the population included a balanced distribution of patients with single vessel and multi-vessel coronary disease.
An important observation in our study was the non-adherence to FFR results in nearly 20% of cases; thus, some patients were deferred from PCI, despite a significant FFR, and others underwent a PCI, despite a non-significant FFR. However, 51.4% of these cases were considered borderline cases with FFR which was slightly above or below the reference cut-off value (4,5) (Figure 3). The final decision in case of borderline cases with “gray zone” FFR values should be based on a combination of clinical judgment, clinical presentation, non-invasive test results, and the focal or diffuse nature of the coronary lesion (6), as was in our study. The high frequency of acute coronary presentations in our study (80%) might have pressured the operators into implementing revascularization strategies, in these borderline cases.
It is particularly challenging to assess an intermediate lesion, defined as 40-70% stenosis. Assessments based solely on angiographic severity may lead to incorrect management (25). Tonini et al. (26) demonstrated that, in cases of intermediate lesions, one cannot rely on the angiogram alone, because there is a significant miscorrelation (only 65% concordance) between the severity assessed with the angiogram and that assessed with FFR measurements. A similar miscorrelation was also reported between assessments made with QCA and FFR measurements (27). In the present study, similarly low correlations were found between the FFR and either the visual estimate (66%) or the calculated QCA (63%) in cases of intermediate lesions (51-70% stenosis). A prominent discrepancy was also observed in the assignment of significant and non-significant lesions (Figure 1). Another important observation was the underestimation of lesion severity with the QCA compared to the visual assessment. This trend was previously reported in the literature and was ascribed to operator bias and technical errors (28). These observations might explain the relatively high prevalence of discordance between FFR recommendations and decisions made in practical practice. Another potential explanation could be an irresistible urge in the operator to treat all significant lesions amenable to PCI; this was previously defined as the “oculo-stenotic reflex” phenomenon (29). Thus, a change in practice towards more functional, FFR-based evaluations may take some time in the present clinical environment.
In our study, the event rates, including mortality and MACE, were relatively low, compared to other contemporary PCI studies (e.g., FAME 1 and COURAGE) (11,29), therefore we could not reach a valid conclusion regarding the outcome.
As mentioned previously, the aim of our study was to investigate the incorporation of FFR in everyday practice in a retrospective analysis, with all the drawbacks that characterize retrospective studies. Since our study includes diverse population, as opposed to the pre-specified population in the FAME and COURAGE trials, we did not attempt to contradict or counteract these trials.
Furthermore, in our study, 37.6% of lesions were estimated to have <50% diameter stenosis. Although higher than previously reported (12), this reflects daily practice discrepancies between visual image and clinical or functional data. This could also have impacted on the event rate.
Our outcome results were similar to those reported by Miller et al. (30), who evaluated real-world, long-term outcomes (death, MI, and revascularization) in patients treated with FFR-guided revascularization strategy. They demonstrated no statistical difference in long-term outcomes for patients deferred and those that underwent PCI.
Limitations
Our study had several limitations. First, it was a retrospective study design, which has inherent limitations including a selection bias. The decision to perform FFR and the choice of management afterwards were determined by the operators. Therefore, selection bias at the outset might have impacted on clinical outcome. However, the aim of this study was to show the incorporation of FFR measurements in actual daily clinical practice. Second, the cohort received FFR measurements relatively infrequently, but mainly over the past 3 years, following the DEFER study (10); therefore, the cohort represented a distinct group of patients with a relatively short follow-up period. Third, the FFR measurements were not performed consistently throughout the study period, due to alterations in our group policies that imposed changes in practice during the study period. Also, the FFR measurements did not include a predefined protocol for the delivered dose of adenosine; rather, the adenosine dose was determined by the operator, and dose delivery followed the protocol accepted at that time in the study period. As we learned over the years, the inherent fallacies in the test could have led to variability between the operators with misleading results. This may have been in part responsible for the discrepancy between the FFR measurement and the visual lesion diameter in the extreme borders. Also, we can’t rule out the possibility that the operators have been biased by the FFR measurements and hence reported a more significant stenosis than originally evaluated to justify the intervention and vice versa. Fourth, only 58% of patients achieved a maximum follow-up period of 2 years; therefore, the true event rate may have been under-represented. Finally, due to the relatively small event rate, attributed to a small population analyzed at a single center, may have impacted the outcome results and multivariate analysis. However, the small selected patient group represents our everyday practice. Nevertheless, our results should be further investigation and validated in larger cohort studies.
Conclusions
Our results suggested that, despite the considerable contribution that FFR evaluations can make to decision making during coronary angiography, the operator’s subjective judgment may continue to play an important role in selected cases, mainly in the borderline ranges. These results should be validated in much larger cohorts.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Guidelines on myocardial revascularization. Eur Heart J 2010;31:2501-55. [PubMed]
- Levine GN, Bates ER, Blankenship JC, et al. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Circulation 2011;124:e574-651. [PubMed]
- Kushner FG, Hand M, Smith SC Jr, et al. 2009 focused updates: ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction (updating the 2004 guideline and 2007 focused update) and ACC/AHA/SCAI guidelines on percutaneous coronary intervention (updating the 2005 guideline and 2007 focused update) a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2009;54:2205-41. [PubMed]
- Pijls NH, Sels JW. Functional measurement of coronary stenosis. J Am Coll Cardiol 2012;59:1045-57. [PubMed]
- Pijls NH, De Bruyne B, Peels K, et al. Measurement of fractional flow reserve to assess the functional severity of coronary-artery stenoses. N Engl J Med 1996;334:1703-8. [PubMed]
- De Bruyne B, Pijls NH, Bartunek J, et al. Fractional flow reserve in patients with prior myocardial infarction. Circulation 2001;104:157-62. [PubMed]
- Pijls NH, Van Gelder B, Van der Voort P, et al. Fractional flow reserve. A useful index to evaluate the influence of an epicardial coronary stenosis on myocardial blood flow. Circulation 1995;92:3183-93. [PubMed]
- Kern MJ. Coronary physiology revisited: practical insights from the cardiac catheterization laboratory. Circulation 2000;101:1344-51. [PubMed]
- Bech GJ, De Bruyne B, Pijls NH, et al. Fractional flow reserve to determine the appropriateness of angioplasty in moderate coronary stenosis: a randomized trial. Circulation 2001;103:2928-34. [PubMed]
- Pijls NH, van Schaardenburgh P, Manoharan G, et al. Percutaneous coronary intervention of functionally nonsignificant stenosis: 5-year follow-up of the DEFER Study. J Am Coll Cardiol 2007;49:2105-11. [PubMed]
- Legalery P, Schiele F, Seronde MF, et al. One-year outcome of patients submitted to routine fractional flow reserve assessment to determine the need for angioplasty. Eur Heart J 2005;26:2623-9. [PubMed]
- De Bruyne B, Pijls NH, Kalesan B, et al. Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N Engl J Med 2012;367:991-1001. [PubMed]
- Tonino PA, De Bruyne B, Pijls NH, et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med 2009;360:213-24. [PubMed]
- Pijls NH, Fearon WF, Tonino PA, et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention in patients with multivessel coronary artery disease: 2-year follow-up of the FAME (Fractional Flow Reserve Versus Angiography for Multivessel Evaluation) study. J Am Coll Cardiol 2010;56:177-84. [PubMed]
- Hamilos M, Muller O, Cuisset T, et al. Long-term clinical outcome after fractional flow reserve-guided treatment in patients with angiographically equivocal left main coronary artery stenosis. Circulation 2009;120:1505-12. [PubMed]
- Bech GJ, Droste H, Pijls NH, et al. Value of fractional flow reserve in making decisions about bypass surgery for equivocal left main coronary artery disease. Heart 2001;86:547-52. [PubMed]
- Legutko J, Dudek D, Rzeszutko L, et al. Fractional flow reserve assessment to determine the indications for myocardial revascularisation in patients with borderline stenosis of the left main coronary artery. Kardiol Pol 2005;63:499-506; discussion 507-8. [PubMed]
- Lindstaedt M, Yazar A, Germing A, et al. Clinical outcome in patients with intermediate or equivocal left main coronary artery disease after deferral of surgical revascularization on the basis of fractional flow reserve measurements. Am Heart J 2006;152:156.e1-9.
- Suemaru S, Iwasaki K, Yamamoto K, et al. Coronary pressure measurement to determine treatment strategy for equivocal left main coronary artery lesions. Heart Vessels 2005;20:271-7. [PubMed]
- Koo BK, Park KW, Kang HJ, et al. Physiological evaluation of the provisional side-branch intervention strategy for bifurcation lesions using fractional flow reserve. Eur Heart J 2008;29:726-32. [PubMed]
- De Bruyne B, Pijls NH, Bartunek J, et al. Fractional flow reserve in patients with prior myocardial infarction. Circulation 2001;104:157-62. [PubMed]
- Leesar MA, Abdul-Baki T, Akkus NI, et al. Use of fractional flow reserve versus stress perfusion scintigraphy after unstable angina. Effect on duration of hospitalization, cost, procedural characteristics, and clinical outcome. J Am Coll Cardiol 2003;41:1115-21. [PubMed]
- Braunwald E. Unstable angina. A classification. Circulation 1989;80:410-4. [PubMed]
- Thygesen K, Alpert JS, White HD, et al. Universal definition of myocardial infarction. Eur Heart J 2007;28:2525-38. [PubMed]
- Tobis J, Azarbal B, Slavin L. Assessment of intermediate severity coronary lesions in the catheterization laboratory. J Am Coll Cardiol 2007;49:839-48. [PubMed]
- Tonino PA, Fearon WF, De Bruyne B, et al. Angiographic versus functional severity of coronary artery stenoses in the FAME study fractional flow reserve versus angiography in multivessel evaluation. J Am Coll Cardiol 2010;55:2816-21. [PubMed]
- Christou MA, Siontis GC, Katritsis DG, et al. Meta-analysis of fractional flow reserve versus quantitative coronary angiography and noninvasive imaging for evaluation of myocardial ischemia. Am J Cardiol 2007;99:450-6. [PubMed]
- Kimball BP, Bui S, Cohen EA, et al. Systematic bias in the reporting of angioplasty outcomes: accuracy of visual estimates of absolute lumen diameters. Can J Cardiol 1994;10:815-20. [PubMed]
- Boden WE, O’Rourke RA, Teo KK, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med 2007;356:1503-16. [PubMed]
- Miller LH, Toklu B, Rauch J, et al. Very long-term clinical follow-up after fractional flow reserve-guided coronary revascularization. J Invasive Cardiol 2012;24:309-15. [PubMed]


