
Will ISCHEMIA change our daily practice?
Introduction
The role of revascularization in the management of stable coronary artery disease (SCAD) has long been a matter of debate in the cardiology community. The COURAGE trial (1) found that percutaneous coronary intervention (PCI) added to optimal medical therapy (OMT) did not reduce the risk of death or myocardial infarction (MI) when compared with OMT alone, thus strongly calling into question the role of PCI in the management of stable CAD. Yet limitations of this trial such as the absence of documented ischemia in a large proportion of patients impacted the applicability of its results to routine clinical practice. Furthermore, the 5-year follow-up of the FAME 2 trial revealed a reduction in the rate of MI among patients who underwent fractional flow reserve-guided PCI compared with OMT alone (2). In an attempt to provide a more definitive response to this debate, the ISCHEMIA trial presented its long-awaited results at the AHA Scientific Sessions in November 2019 with subsequent publication in the New England Journal of Medicine in April 2020 (3). This well-designed and rigorously conducted study randomized over 5,000 patients with proven moderate or severe ischemia to either an invasive strategy (routine angiography with optimal revascularization plus OMT) or OMT alone. After a median follow-up of 3.3 years, the invasive strategy failed to show a significant reduction in the composite primary endpoint of cardiovascular death, nonfatal MI, hospitalization for unstable angina, hospitalization for heart failure, or resuscitated cardiac arrest. Of note, a significant reduction in spontaneous MI in the invasive group appeared to be counterbalanced by significantly higher rates of periprocedural MI associated with this strategy. However, there was a significant improvement in angina control and quality of life among patients with baseline angina treated with the invasive strategy.
These striking results have already generated a significant amount of heated reaction and debate in the medical community and the media. However, given the extensive exclusion criteria of this study, the recurrent question has arisen again: will these results actually change the daily practice of interventional cardiologists in a public university hospital like ours in Europe?
We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/cdt-20-258).
Methods
In order to objectively assess the impact of ISCHEMIA on our daily practice, we performed a retrospective analysis of the last 1,000 consecutive PCIs performed in our tertiary center—one of five university hospitals in Switzerland—between October 2018 and October 2019. The only inclusion criterion was that each procedure had to be a PCI done during the above-mentioned period. There were no exclusion criteria. Data were extracted from the electronic database containing the record of all procedures done in our center. We applied the ISCHEMIA exclusion criteria (4) to this population in order to estimate the proportion of these patients that would have been excluded from the trial. The sample size was fixed at 1,000 as it globally represents the average yearly volume of PCI in our center. The present study was realized in compliance with international ethics guidelines outlined in the Declaration of Helsinki (as revised in 2013). No specific dedicated ethical committee approval was necessary as this study only reports our cath-lab activity without any patients data. Because of the retrospective nature of the research, the requirement for informed consent was waived.
Results
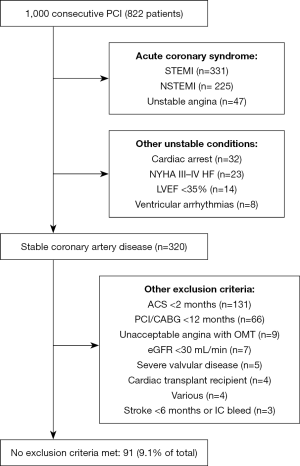
Between October 2018 and November 2019, 1,000 PCIs were performed. Among these, 603 (60.3%) were for acute coronary syndromes (ACS) and 197 (19.7%) were in the context of either an ACS within 2 months (n=131), or a PCI/CABG within 12 months (n=66) (Figure 1). A further 84 (8.4%) were performed in patients with other high-risk features (ventricular arrhythmias, cardiac arrest, NYHA III-IV heart-failure, eGFR <30 mL/min or LVEF <35%). Finally, a further 25 (2.5%) procedures were performed in patients with either unacceptable angina whilst on OMT, a cardiac transplant, recent stroke, or another exclusion criterion (see Figure 1). This left only 91 patients (9.1%) without any ISCHEMIA exclusion criteria.
Discussion
These results demonstrate that in the routine practice of a real-world, public PCI center, only a small fraction of PCIs would be potentially affected by the results of ISCHEMIA. This finding was in part driven by an important proportion of ACS patients in our center. However, PCI for the treatment of ACS represents a significant proportion of PCIs performed in other centers (5).
The same analysis was also performed based on patients with stable CAD. Among patients with stable CAD (n=320), 229 patients (71.6%) undergoing PCI would have been excluded from ISCHEMIA due to the presence of at least one exclusion criteria, despite the potential benefit of PCI in these patients. The most notably excluded group of patients were those with a history of ACS within the last 2 months. A total of 131 PCIs (40.9%) fell into this category, with all patients undergoing PCI to significant bystander lesions identified during the index coronary angiography for the ACS. These patients were excluded from ISCHEMIA but numerous studies, most notably the COMPLETE trial (6), have shown the benefits of complete revascularization in this setting. The second largest excluded subgroup consisted of patients that had undergone PCI or CABG in the previous 12 months, an occurrence that is not uncommon, particularly among ACS patients (7). A total of 66 PCIs (20.6%) fell into this category. The remaining 32 excluded patients (10.0%) fell into various categories that were poorly represented in the study population.
In conclusion, in this retrospective analysis of 1,000 PCIs performed in a Swiss university hospital, 90.9% of PCIs were performed in patients that would have had at least one exclusion criterion from ISCHEMIA. Of note, even among patients with stable CAD, 71.6% would have had at least one exclusion criterion from ISCHEMIA.
One of the major limitation of the present report is that as a public university hospital, the proportion of patients presenting with ACS tends to be higher than in other PCI centers where the population probably matches better the ISCHEMIA inclusion and exclusion criteria. However these results suggest that the impact of ISCHEMIA on the real-world practice of a public university hospital might be limited.
Acknowledgments
Funding: SF is supported by a research grant from the CardioPaTh PhD programme.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/cdt-20-258
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/cdt-20-258). SF reports consulting for CathWorks and Bayer. DM reports consulting for Bayer. TM has no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The present study was realized in compliance with international ethics guidelines outlined in the Declaration of Helsinki (as revised in 2013). No specific dedicated ethical committee approval was necessary as this study only reports our cath-lab activity without any patients data. Because of the retrospective nature of the research, the requirement for informed consent was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Boden WE, O'Rourke RA, Teo KK, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med 2007;356:1503-16. [Crossref] [PubMed]
- Xaplanteris P, Fournier S, Pijls NHJ, et al. Five-Year Outcomes with PCI Guided by Fractional Flow Reserve. N Engl J Med 2018;379:250-9. [Crossref] [PubMed]
- Maron DJ, Hochman JS, Reynolds HR, et al. Initial Invasive or Conservative Strategy for Stable Coronary Disease. N Engl J Med 2020;382:1395-407. [Crossref] [PubMed]
- ISCHEMIA Trial Research Group, Maron DJ, Hochman JS, et al. International Study of Comparative Health Effectiveness with Medical and Invasive Approaches (ISCHEMIA) trial: Rationale and design. Am Heart J 2018;201:124-35. [Crossref] [PubMed]
- Kim LK, Feldman DN, Swaminathan RV, et al. Rate of percutaneous coronary intervention for the management of acute coronary syndromes and stable coronary artery disease in the United States (2007 to 2011). Am J Cardiol 2014;114:1003-10. [Crossref] [PubMed]
- Mehta SR, Wood DA, Storey RF, et al. Complete Revascularization with Multivessel PCI for Myocardial Infarction. N Engl J Med 2019;381:1411-21. [Crossref] [PubMed]
- Yudi MB, Ajani AE, Andrianopoulos N, et al. Early versus delayed percutaneous coronary intervention in patients with non-ST elevation acute coronary syndromes. Coron Artery Dis 2016;27:344-9. [Crossref] [PubMed]


