
Mediastinal liposarcoma masquerading as penetrating aortic ulcer in the descending aorta: a case report
Introduction
The term penetrating aortic ulcer (PAU) is characterized by an atherosclerotic plaque ulcerates and burrows through the internal elastic lamina into the media, leading to a variable amount of hematoma (1). However, liposarcoma are one of the most hardly diagnosed subtypes of soft tissue malignancies. Their deceptive presentation often creates a challenging diagnostic dilemma for providers who are trying to narrow down a vast differential diagnosis which includes lipoma, hematoma, lymphedema, cyst and abscess, amongst others. Herein, we describe a rare case of liposarcoma invades descending aorta, initially masquerading as PAU. We present the following case in accordance with the CARE reporting checklist (available at http://dx.doi.org/10.21037/cdt-20-287).
Case presentation
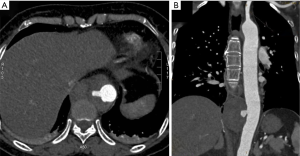
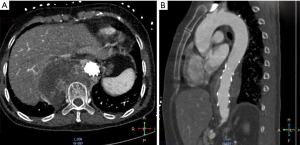
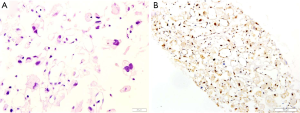
A 56-year-old woman with a history of hypertension and cerebral infarction was admitted to the hospital complaining of progressive and severe chest pain for 1 day. Computed tomography (CT) scan revealed a PAU in descending aorta measuring 4.0×6.1×6.1cm at the level of thoracic vertebrae T9 to T10 (Figure 1). Vascular abnormalities as assessed with CT angiography, the anatomic conditions are suitable for thoracic endovascular aortic repair (TEVAR), we repaired the PAU using a 26×26×80 Hercules-T (Microport, Shanghai, China) stent graft. The procedure was uneventful and she was discharged after a week. One month later the patient presented to our clinic with chest and back pain. The contrast CT indicated the growth of a mass, which interpreted as hematoma resulting from endoleak (Figure 2). We subsequently performed an urgent diagnostic angiography, but no endoleak was found. At this stage, the patient was frail, we noted she had lost 5 kg weight in the past month. Laboratory examinations including alpha-fetoprotein, carcinoembryonic antigen, CA-125, CA-199, antistreptolysin O, rheumatoid factor was unremarkable, but C-reactive protein (CRP) was increased to 17.4 mg/L. These findings indicated that we should have raised suspicion of an alternative diagnosis. To confirm the diagnosis, CT-guided needle biopsy was carried out, the histology of the mass revealed a pleomorphic liposarcoma (Figure 3). The patient has refused surgery due to her frail condition and high risk for open surgical repairs, she eventually died after a month.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for accompanying images for academic publication purposes.
Discussion
Liposarcomas are malignant fat-containing tumors derived from mesenchymal cells that typically occur in the extremities and retroperitoneum, mediastinum maybe one of the rarest primary site, accounting for less than 1% of all liposarcomas (2). In addition, mediastinal liposarcoma account for only 0.1% to 0.75% in mediastinal malignancies (3). Liposarcomas separated into four histologic subtypes: well differentiated, dedifferentiated, myxoid, and pleomorphic; pleomorphic liposarcoma is the least common malignant adipocytic neoplasm, accounting for approximately 5% of all cases (4). Cases of liposarcoma invading vascular system are seldom, there are just 2 cases reported that retroperitoneal liposarcoma invading abdominal aorta (5,6). Mediastinal pleomorphic liposarcoma invaded the aorta simulating PUA of the descending aorta is an extremely rare occurrence and has not been previously reported in the literature.
The liposarcoma usually presents as a space-occupying lesion, mediastinal liposarcoma is most frequently identified occasionally on imaging performed for other reasons as many patients remain asymptomatic even with the large tumor size. Symptoms typically arise from compression or irritation of adjacent intrathoracic structures and include chest pain, dyspnea, tachypnea, wheezing, hoarseness. The possible symptoms of mediastinal liposarcoma are superior vena cava compression, arrhythmias and heart failure. Nevertheless, this situation can also be manifested in aortic diseases, including thoracic PAU. The typical PAU patient is elderly with multiple cardiac risk factors and presents with acute chest or back pain (1). Coincidentally, our case presented to our clinic with the complaint of chest pain.
Mediastinal liposarcoma have a nonspecific imaging appearance on chest radiography. On CT scan, imaging manifestations of liposarcoma depend on the degree of differentiation of these subtypes. Mediastinal liposarcoma manifests as a fat-containing mass or soft tissue nodularity, typically appears in the well-differentiated/ dedifferentiated liposarcoma, they have homogeneous fat attenuation of approximately -100HU, while the fibrous septa of well-differentiated liposarcoma may be thicker and irregular. Cyst-like appearance may be found in myxoid liposarcoma. The hemorrhage and necrosis area is commonly observed in the pleomorphic liposarcoma (2). The appearance on MRI is also exhibiting the typical intensity characteristics of macroscopic fat: intrinsic T1 hyperintense signal with loss of signal on fat saturation sequences (7). The typical appearance of a liposarcoma on F-18-FDG PET/CT varies based upon its internal components and degree of heterogeneity, higher grade portions of a liposarcoma will show a higher maximum standard uptake value and indicate increased metabolism (8).
In this case, the CT scan exhibited similar imaging characteristics of hematoma, mediastinal liposarcoma is uncommon and lack of a high index of suspicion is the main reason for misdiagnosis. When we excluded the possibility of endoleak after angiography, we realized that it is not the case. Finally, CT-guided biopsy achieved a confirmed diagnosis. Microscopically, MDM2 overexpression represents as a diagnostic marker of liposarcomas; pleomorphic liposarcoma cytological atypia can be extreme, and lipoblasts are frequently large, irregular, hyperchromatic and scalloped nuclei (4). Pleomorphic liposarcoma is the most aggressive, exhibiting avidity for systemic spread and a poor overall outcome (9). The primary treatment for liposarcoma is surgical resection, chemotherapy or radiotherapy is considered to be almost ineffective. But it is worth mentioning that the majority of aortic diseases, including PUA ones, are being repaired by endovascular techniques in the modern endovascular era. In such situation, lack of histological evaluation also poses a limitation.
In conclusion, the learning point from the present case is that mediastinal liposarcoma should arise as a differential diagnosis in symptomatic patients with growing periaortic mass post-TEVAR when endograft-related causes have been excluded. Promptly CT-guided biopsy may help establish an early diagnosis.
Acknowledgments
Funding: This work was supported by the National Natural Science Foundation of China (No. 81860715).
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/cdt-20-287
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/cdt-20-287). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013).Written informed consent was obtained from the patient for accompanying images for academic publication purposes.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Braverman AC. Penetrating atherosclerotic ulcers of the aorta. Curr Opin Cardiol 1994;9:591-7. [Crossref] [PubMed]
- Yang YS, Bai CY, Li ZC, et al. Giant primary liposarcoma of the anterior mediastinum: A case report. Medicine (Baltimore) 2018;97:e12873. [Crossref] [PubMed]
- Sekine Y, Hamaguchi K, Miyahara Y, et al. Thymus-related liposarcoma: report of a case and review of the literature. Surg Today 1996;26:203-7. [Crossref] [PubMed]
- Dei Tos AP. Liposarcomas: diagnostic pitfalls and new insights. Histopathology 2014;64:38-52. [Crossref] [PubMed]
- Karkos CD, Pepis PD, Theologou M, et al. Retroperitoneal Liposarcoma Masquerading as an Impending Rupture of Inflammatory Abdominal Aortic Aneurysm. Ann Vasc Surg 2019;56:354.e21-354.e23. [Crossref] [PubMed]
- Paravastu SCV, Ghosh J, Farquharson FG, et al. Rupture of an abdominal aortic aneurysm post EVAR: a rare presentation of retroperitoneal liposarcoma. Vasc Endovascular Surg 2010;44:494-8. [Crossref] [PubMed]
- Von Schulthess GK, McMurdo K, Tscholakoff D, et al. Mediastinal masses: MR imaging. Radiology 1986;158:289-96. [Crossref] [PubMed]
- Rakheja R, Makis W, Skamene S, et al. Correlating metabolic activity on 18F-FDG PET/CT with histopathologic characteristics of osseous and soft-tissue sarcomas: a retrospective review of 136 patients. AJR Am J Roentgenol 2012;198:1409-16. [Crossref] [PubMed]
- Ghadimi MP, Liu P, Peng T, et al. Pleomorphic liposarcoma: clinical observations and molecular variables. Cancer 2011;117:5359-69. [Crossref] [PubMed]


