Developing a national salt reduction strategy for Mongolia
Introduction
Non-communicable diseases (NCDs) are the main contributors to premature mortality and morbidity globally (1,2). In the Western Pacific region, for example, the major NCDs—cardiovascular disease (CVD), diabetes mellitus, cancer and chronic respiratory disease—account for more than 80% of all deaths (3). As an important primary risk factor for CVD, excessive salt intake is estimated to contribute to millions of premature deaths, mainly through elevations in blood pressure (BP) (4,5).
Reducing salt intake has been identified as one of the most cost-effective measures to reduce the burden of NCDs (6-10). New World Health Organization (WHO) guidelines recommend adults daily consumption of salt be reduced to less than five grams (5). The global strategy on NCDs, endorsed by the WHO’s Western Pacific region in 2010, called upon member states to determine salt intake, identify which food products are the main sources of salt, and implement national strategies to reduce salt intake in populations (5,11-13).
Mongolia is the fifth largest country in terms of land area (1.6 million square kilometres) in Asia, but only had a population of 2.93 million (48.7% males and 51.3% females) in 2013, making it one of the least densely populated country in the world. However, urbanization of the population over the last century, and particular in recent decades, has resulted in over two thirds of the population (67.2%) now residing in cities (14,15), with associated rapid increase in NCDs. NCD related deaths now comprise approximately 80% of total mortality in this population (15,16), which is seven times higher than other countries of the Western Pacific region. NCDs, such as heart disease, diabetes mellitus, stroke, some preventable cancers and injuries, are the leading causes of premature death and disability in the largely young to middle aged structured population of Mongolia (15,17). In particular, the prevalence of risk factors for NCDs such as an unhealthy diet (including excess salt intake) is high.
Periodic NCD risk factor surveillance through WHO STEP wise approach to Surveillance (STEPs) (18) surveys in Mongolia have shown that unhealthy lifestyle behaviors are increasing, despite several health promoting initiatives (15,16). According to the three consecutive STEPs surveys in 2005, 2009 and 2013, the proportion of people aged 15-64 years with multiple combined risk factors was 23.8%, 26.4%, and 36.9%, respectively (18-20). Since 2011, the country’s Ministry of Health (MOH) and National Centre for Public Health of Mongolia have been acting on WHO recommendations to reduce the salt intake of the population. This paper provides an overview of the work to develop the national salt reduction strategy in Mongolia for 2015 to 2020, and highlights a range of lessons for other countries for consideration when developing national salt reduction strategies.
Methods
Following on from the WHO regional consultation on salt reduction in Singapore in June 2010, the MOH in collaboration with Millennium Challenge Health project, WHO and the National Center for Public Health in Mongolia, organized a salt reduction consultation meeting in the capital city, Ulaanbaatar (UB). An inter-sectoral working group was established and a series of meetings were conducted with government officials and technologists from bread companies and the meat industry. The objectives of these meetings were to raise awareness of the burden of NCDs associated with high salt intake, introduce the WHO recommendations on salt reduction, and invite the food industry and other stakeholders to collaborate on efforts to reduce salt intake across the population. An action plan to establish a national baseline on salt consumption patterns and implement a series of pilot initiatives to reduce salt intake was developed and endorsed by all of the key stakeholders.
Baseline data on salt intake were obtained through a cross-sectional, nationally representative survey on a random sample of 1,040 residents (25-64 years) selected from 2010 population census in 2011 (21). Permission to conduct the study was granted by the Ethics Review Committee of the health care sector of the MOH, Mongolia (Resolution 14, 8 July 2011). The sample size was calculated in accordance with international protocols (21). The randomly selected participants were informed orally about the survey as well as being provided with a written participant information and consent form 1-2 days prior to the survey. People with major illnesses were excluded. Data collection comprised an interviewer-administered questionnaire on demographic information and health status, and knowledge, attitudes and behavior relating to salt. Participants were also asked to recall their dietary intake over the previous 24 hours, and to provide a single 24-hour urine sample.
Data analysis was undertaken using SPSS (Version 19). Descriptive statistics were calculated using One-Way ANOVA with 95% confidence intervals and comparisons were made using one-Sample t-tests or multiple comparison post host tests (Tukey HSD test, Sidak test, and Tamhane test). The mean differences were assumed to be significant at P<0.005.
Data from the 24-hour dietary recall was analysed using FoodWorks adapted with Mongolian food composition and data from surveys of the nutritional composition of products in shops to assess the contribution of different foods to salt in the diet. A series of salt reduction initiatives were also implemented between 2011 and 2014. Results of these surveys and salt reduction initiatives informed proposals for a national salt reduction strategy in 2014.
Results
Establishing a national baseline 2011-2012
Salt intake
Twenty four-hour urine samples were collected from 1,027 participants (98.7% participation rate) (Table 1) and analysed for sodium, potassium and creatinine. Following exclusion of incomplete urine collections (based on volume and creatinine measurements), the mean (SD) salt intake was estimated at 11.06 (5.99) g per day, which is more than double WHO recommendations (5 g per day). Furthermore, the majority 89.2%; (95% CI, 87.3-91.0; P<0.001) of the population consumed over five grams of salt per day.
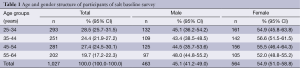
Full table
There were significant variations in mean levels of salt intake in relation to gender, region and residential location (rural versus urban) but there was no significant difference in relation to age. Mean salt intake (grams per day) in males was 11.68 (6.15) as compared to 10.54 (5.81) in females; mean difference 1.14 (95% CI, 0.58±1.70; P<0.001). Mean salt intake in the Western region was 13.48 (7.49), Khangai region 10.80 (5.45), Central region 10.07 (6.34) and Eastern region 9.98 (5.14) (P<0.001), and of UB 10.89 (5.49). Mean salt intake in urban areas was 11.32 (6.06) compared to 10.64 (5.86) in rural areas (P<0.005).
Consumer knowledge, attitudes and behavior
Most people (87.5%) understood the adverse effects of salt on health. However, about half of the survey participants reported regularly consuming salty tea and high-salt meals. About one third were not making any efforts to reduce their consumption of salt, with one fifth unable to correctly name food products high in salt. Salt intake was directly associated with a person’s knowledge, attitude and behaviours related to salt. For instance, daily salt intake was 10.20 (5.43) g per day for people who reported never using table salt, as compared to 11.81 (6.34) g per day in those who reported using table salt regularly (P<0.001).
Interestingly, people who drank the popular salty tea had the highest intake of salt and were more likely to have hypertension. People who consumed salty tea on daily basis consumed 11.81 (6.34) compared to 10.20 (5.43) g of salt per day for those who avoided salty tea; mean difference of 1.61 (95% CI, 1.10-2.22; P<0.002). The frequency of hypertension was 40.4% (95% CI, 32.6-48.6) in people who consumed salty tea as compared to 37.8% (95% CI, 30.6-45.6) in those who drank tea without salt (P<0.001). Multivariate regression analysis showed that salt intake was 12.15 (95% CI, 10.73-13.58) gram per day in those who drank salty tea and had arterial hypertension as compared to 10.23 (95% CI, 9.48-10.98) in those who had normal arterial pressure and had tea without salt (1.92 difference, P<0.001).
Main sources of salt in the diet
The main sources of salt identified through the dietary survey were salted tea, sausage, smoked meat products, pickled vegetables, chips, traditional fast food (Buuz steamed dumpling, Khuushuur-fried dumpling), and Western fast food (burgers, hot dog and pizza), mayonnaise, spices, sauces, and canned meat products. For the 474 participants who reported consuming salty tea, salt from tea alone was estimated to contribute 30% of total salt consumption, with the remainder from meals (23%) and other processed foods (47%).
Implementation and monitoring of salt reduction initiatives
Pinch Salt Mongolia
Following the salt reduction consultation in May 2011, a pilot salt reduction initiative-Pinch Salt Mongolia-was implemented in UB. The main objective was to reduce salt intake of the employees of three of the main food producing factories (Makh Impex, Talkh Chikher and Goyo). Implementation strategies included the training of staff on the negative health impact of salt and how to consume a healthy diet, and the provision of reduced salt food and meals through company canteens and workers’ kitchens (Talkh Chikher and Goyo).
Pre- and post-intervention monitoring was undertaken to determine salt intake using 24-hour urine tests (n=240) and a questionnaire. The results showed that salt intake reduced from 11.48 (7.32) g per day in 2011 to 8.65 (4.26) g per day in 2013. The number of respondents who didn’t know which foods were high in salt declined from 18.5% (95% CI, 14.0-23.9) to 2.9% (95% CI, 1.1-7.4) during the same period.
Pre- and post-intervention monitoring to assess the salt content of meals served in two companies was also undertaken using the “NaCl ion by titration” method on 50 samples of meals in the laboratory of the National Center for Public Health. Mean salt content of meals prior to the intervention was 1.18 (1.11) per 100 g compared with 0.74 (0.36) per 100 g post-intervention, a reduction of 0.44 g or 37.29%.
Food industry initiatives to reduce salt in bread
A series of food industry initiatives to reduce salt in bread were initiated in parallel with the pilot project. The Talkh Chikher bread company first reduced the salt content in its “Atar” bread by 12% in May 2011, following a visit from the MOH and technical experts as part of the salt reduction consultation. Other companies followed suit, resulting in the salt content of bread in 10 bread and bakeries declining by 1.6% on average after May 2011. This equates to 22 tonnes of salt being cut from food processing in just one year. From 2012-2014, this initiative further expanded to other industries including the meat industry and mass catering services. For example, in 2014, the sausage industry agreed to reduce the salt content in three canned products by 10%. In addition, the media was used to increase public and professional awareness about the need to reduce salt in foods.
Annual World Salt Awareness Week activities
Since 2012, The National Public Health Institute and MOH have collaborated on implementing a range of activities as part of World Salt Awareness Week in March each year (22). For example, in 2014, and in line with the international theme “Stop… Look…Choose… the Lower Salt Option”, a series of adverts on television were run, and campaign materials with information about salt and product labelling were promoted on the web-site of key stakeholders that included the Mongolian Food Association. Materials were also disseminated through institutional Facebook sites, posters and advertising boards. Media interest is usually significant with many multi-media programs asking to participate and conduct interviews.
Development of a salt reduction strategy for Mongolia
The pilot salt reduction activities in Mongolia have been viewed as a success and demonstrate the potential for action. However, there is now a need to scale them up to a national level and ensure that Mongolia is in a position to meet global targets (23). This will require the establishment of a policy and legal environment for limiting the production and consumption of salt which in turn needs to be backed by adequate financing.
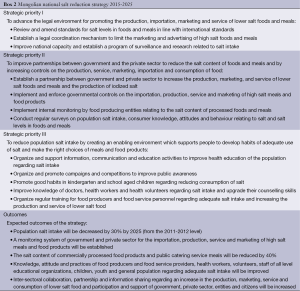
The main goal of the Mongolian national salt reduction strategy that was agreed in 2014 is therefore: to create a social, economic and legal environment to support the reduction of population salt intake by 30% by 2025 (Box 1). Building on the progress of intervention initiatives to date, the three strategic priorities of the strategy are to advance the legal environment for salt reduction; to improve partnerships, and to create an enabling environment to support consumers to make the right choices. In addition to a reduction in salt intake across the population as a result of improved consumer attitudes and behaviours relating to salt and reduced salt levels in foods and meals, it is expected that the main outcomes of the strategy will be improved partnerships and inter-sector collaboration to re-enforce and monitor food supply.

Full table
The Mongolian national salt reduction strategy will be implemented during the period 2015-2025, and mid-term and final evaluations are to be undertaken in 2020 and 2025. Monitoring and evaluation of the strategy will be carried out by the Central Government Ministries responsible for health and food in collaboration with other relevant organizations such as city council and inspection organisations.
Discussion
There is strong stakeholder support for the national salt reduction strategy in Mongolia. The baseline assessment showed that the population is consuming on average 11 g of salt each day, more than twice that recommended by WHO, making it one of the highest salt intake countries in the Western Pacific Region. A key driver of this high salt intake is the population habit of adding salt to tea, making tea account for about one third of total salt intake for a large proportion of people. “Suutei tsai” (literally “tea with milk”) is a traditional Mongolian beverage, usually consisting of tea, milk, butter and salt (1 g/200 mL tea), is consumed by 46% of the population in Mongolia regularly throughout the day. Mongolia is one of the few places in the world (in addition to Tibet and Kashmir) where salty tea is drunk.
The survey results are likely to be robust. The rigorous training and support provided to the survey team to ensure that the 24-hour urines were collected effectively, including text message reminders to each of the participants to collect the urine and record the times, resulted in an extremely high (98.7%) participation rate. What’s more, the findings from the current study are in line with previous studies of salt intake in Mongolia which have also demonstrated differences in salt intake for normotensives and hypertensives (24,25), and shown that salt is a significant risk factor for Isolated Systolic Hypertension in Mongolia (26). The new findings add strength to the argument in support of a national salt reduction strategy in Mongolia.
The positive outcomes of the intervention projects and the strong stakeholder support demonstrate the potential for the salt reduction initiative to be scaled up to a national level. Plus there are a range of lessons for other countries (Box 2). The 2.8 g reduction in salt intake as a result of the pilot Pinch Salt intervention project and the 12% reduction in salt in the most popular bread sold in Mongolia are remarkable achievements within a relatively short time period. The success of the work is largely due to the strong support of the government as well as the availability of funding and stakeholder engagement. Robust baseline data relating to salt intake, consumer practices and salt content of major foods combined with the evidence of effectiveness of interventions in UB from the pilot studies, provide a solid basis for action.
Full table
However, reducing daily salt intake by 30% (to 8.5 g) will nevertheless be challenging. The pilot interventions were time-limited projects in selected groups, and representative of the processed food industry (e.g., pickled vegetable producers) have not yet agreed to reduce the salt content of their products.
That said, as most key stakeholders are united in their commitment to reduce salt, and the country has a good track record on NCDs, the chances of the salt reduction strategy being a success are considered positive. Mongolia has already successfully implemented its first National Programme for NCD risk factors during 2006-2013 (27), clearly demonstrating the potential to effectively address NCDs through high level commitment and through the participation of a wide range of community sectors. NCDs are a high priority for the Mongolian government which has commenced a second program of work in 2014 that includes commitments to: develop and support low salt content in food production, trade and service industries; provide and co-ordinate policy on the reduction of high salt foods; and increase the update of national food standards to limit the salt content of foods.
Although a policy framework has been established, the process of implementation and evaluation will take some time to develop. The social, legal and economic infrastructure to support the implementation of the salt reduction strategy will need to be strengthened, as Mongolians like salty foods and drinks and salt has been a traditional condiment for centuries. These things together, combined with the rapid urbanisation and the increased availability of highly processed salty foods, mean a major and sustained consumer education effort will be needed to reverse the current taste preferences in Mongolia.
Establishing a legislative framework to limit the intake of salt for both domestically produced and imported processed foods and meals, and the monitoring of salt levels in foods and meals will also be crucial elements of the salt reduction strategy. This study revealed that 75.4% of processed foods and 84.3% of meals are high in salt. One of the favourite foods of Mongolians is sausage. Domestic sausage producers are already examining opportunities to reduce salt, but more than 70% of the processed foods in Mongolia are imported. Whist the local food industry has indicated their willingness to participate, with early demonstrations of substantial reductions in salt levels, the same standards need to be applied to imported foods for the strategy to be sustainable.
The strategy could also be further enhanced through ongoing surveillance of NCDs, in particular a population-based study of the incidence of stroke, as Mongolia has one of the highest rates of stroke in the world (28). It would be extremely useful to demonstrate how the effective implementation of salt reduction in the population could translate into reduced incidence of stroke within a 5-10 year horizon.
Conclusions
The Mongolian government has identified the tackling of NCDs as a high priority health objective for its population. The national salt reduction strategy for Mongolia will help to ensure that this objective can be achieved. The strategy is clearly focused and unites all players: government, the food industry and community, in one ultimate goal—to reduce salt intake in Mongolia by 30% by 2025. Robust interim monitoring of the strategy will help ensure it is on track to meet these global targets. The addition of a population-based stroke surveillance program would provide a reliable direct assessment of the impact of the salt reduction initiatives on the health outcomes. The results would likely be widely generalizable to other populations experiencing similar lifestyle transitional changes.
Acknowledgements
Membership of the inter-sectoral working group on the Establishment of Legal and Policy Environment for Reduction of Hidden Salt Production and Intake in Mongolia is as follows: Head: Dr. Jamayan Batjargal (Public Health Institute), Secretariat: Batsaikhan Enkhtungalag (Public Health Institute), Dr. Ganzorig D (Ministry of Health and Sport), Dr. Baigalmaa D (Ministry of Health and Sport), Dr. Choi-Ish L (Ministry of Food and Agriculture), Dr. Oyungerel D (Ministry of Food and Agriculture), Ms Amarjargal A (Ministry of Food and Agriculture), Tsetsegdary G (NCDs Adviser, Public Health Institute), Tserenlkham B (Public Health Institute), Urgamal D (State Specialized Inspection Agency), Khulan T (City Health Department), Byambasuren B, (City Health Department), Tsentsenbileg (Mongolian Food Industry Association), Davaasuren D (Mongolian Agency for Standardization and Metrology), Odonchimeg N (City Specialized Inspection Department), Erdenekhuu Sh (Gun shim, Food Production and Services Development Centre).
The study team would also like to acknowledge Kathy Trieu and Mary-Anne Land at the George Institute for Global Health, the Public Health Institute of Mongolia, The World Health Organization, 3 and 22 khoroos and the District Health Center of Bayanzurkh District, Department of Health, Bulgan, Dundgobi, Khentii, and Uvs aimags, doctors and other health workers of soum hospitals, “Goyo” Co. Ltd., “Talkh Chikher” Co. Ltd.,“Makh Impex” Co. Ltd., the Mongolian University of Technology and Science of Mongolia, Otgontenger University, Student canteen of the Orchlon School; City Health Department, Health Center of Sukhbaatar District, “Makh Impex” Co. Ltd., “Talkh Chikher” Co. Ltd., Canteen of the “Goyo” Co. Ltd.; “BBQ Chicken”, “Beijing”, “Ben Jeo” “Jin Hi and I”, “Nandin” Restaurant; “Ukraine Mongol Zoog”, “Tokhilog Zoog”, “Narlag Zoog”, “Altai tooroi”, “Jargalan”, “Khaan buuz” restaurants; “Shimt buuz”, “Talst”, “Niislel”, “Dol”, “Narantuul”, “Tsetsgen buuz”, “Ramon”, “Freedom”, “Khongor”, “Zun tsag”, “Bayalag buuz”, “Mongol Khaan” caffes for their full support and participation. Additional funding support for different parts of the study in Mongolia was provided by the World Health Organization, Millennium Challenge Corporation of the USA and “Health project” of Millennium Challenge Account Mongolia.
Disclosure: Jacqui Webster is Director of the WHO Collaborating Centre on Population Salt Reduction at the George Institute for Global Health. She is supported in her work through an Australian government National Health and Medical Research Council (NHMRC) and National Heart Foundation Career Development Fellowship on International Salt Reduction Strategies. She receives additional funding from NHMRC, VicHealth and the World Health Organization for work on salt reduction. Craig Anderson is supported by a Senior Principal Research Fellowship of the NHMRC.
References
- World Health Organization. Reducing salt intake in populations: report of a WHO forum and technical meeting 5-7 October 2006, Paris, France. Geneva, Switzerland: World Health Organization, 2007. Accessed on 2015 27 February. Available online: http://www.who.int/dietphysicalactivity/Salt_Report_VC_april07.pdf
- World Health Organization. Global Health Risks- Mortality and burden of disease attributable to selected major risks. Geneva, Switzerland: World Health Organization, 2009. Accessed on 2015 27 February. Available online: http://www.who.int/healthinfo/global_burden_disease/GlobalHealthRisks_report_full.pdf
- WWorld Health Organization Western Pacific Region. Noncommunicable diseases in the Western Pacific Region: a profile. Geneva: World Health Organization, 2012 (Accessed on 13th March, 2015). Available online: http://www.moh.gov.my/index.php/file_manager/dl_item/624746305a584e305833426b5a69394f51305176546b4e4558326c755833526f5a5639585a584e305a584a755831426859326c6d61574e66556d566e61573975587a49774d5449756347526d
- He FJ, MacGregor GA. Salt reduction lowers cardiovascular risk: meta-analysis of outcome trials. Lancet 2011;378:380-2. [PubMed]
- World Health Organization. Guideline: Sodium intake for adults and children. Geneva: World Health Organization, 2012. Accessed on 2015 27 February. Available online: http://www.who.int/nutrition/publications/guidelines/sodium_intake_printversion.pdf
- Cobiac LJ, Vos T, Veerman JL. Cost-effectiveness of interventions to reduce dietary salt intake. Heart 2010;96:1920-5. [PubMed]
- Mason H, Shoaibi A, Ghandour R, et al. A cost effectiveness analysis of salt reduction policies to reduce coronary heart disease in four Eastern Mediterranean countries. PLoS One 2014;9:e84445. [PubMed]
- Cobiac LJ, Magnus A, Lim S, et al. Which interventions offer best value for money in primary prevention of cardiovascular disease? PLoS One 2012;7:e41842. [PubMed]
- Webster JL, Dunford EK, Hawkes C, et al. Salt reduction initiatives around the world. J Hypertens 2011;29:1043-50. [PubMed]
- World Health Organization and World Economic Forum. From burden to "best buys": Reducing the economic impact of NCDs in low- and middle-income countries. Available online: http://www.who.int/nmh/publications/best_buys_summary/en/
- World Health Organization Regional Office for the Western Pacific. Regional Consultation on Strategies to Reduce Salt Intake. Available online: http://www.wpro.who.int/noncommunicable_diseases/documents/docs/RCStratReduce_Salt_Intake.pdf
- World Health Organization. Global Action Plan for the Prevention and Control of Non Communicable Diseases 2013-2020. Accessed on 2015 27 February. Available online: http://apps.who.int/iris/bitstream/10665/94384/1/9789241506236_eng.pdf?ua=1
- World Health Organization. Accessed on 2015 2 March. Available online: http://www.un.org/en/ga/ncdmeeting2011/pdf/NCD_draft_political_declaration.pdf
- National Statistical Office of Mongolia. Mongolian Statistical Year Book-2013. National Statistical Office of Mongolia (NSOM), 2014. Accessed on 2015 27 February. Available online: http://www.nso.mn/content/1050#.VUBu0_yUebM
- Centre for Health Development. Health Indicators. Ulaanbaatar: Ministry of Health Mongolia, 2013. Accessed on 2015 27 February. Available online: http://www.chd.moh.mn/images/pdf/sma/2013/English%20indicator-2013.pdf
- Mongolian Government. Second National Program on Prevention and Control of Lifestyle Related Diseases. Mongolian Government, 2014. Accessed on 2015 2 March. Available online: http://www.legalinfo.mn/law/details/9799
- World Health Organization. Policy Brief: Reducing the Use of Salt in the Food Industry to Lower Sodium Consumption. Geneva: World Health Organization, 2014. Accessed on 2015 27 February. Available online: http://www.who.int/nmh/ncd-coordination-mechanism/Policybrief34.pdf
- World Health Organization. STEPS survey on the prevalence of noncommunicable disease and injury risk factors, Mongolia-2013 summary of findings. Ulaanbaatar, Mongolia: World Health Organization, 2014.
- World Health Organization Western Pacific Region. Mongolian STEPS Survey on the Prevalence on Noncommunicable Disease Risk Factors 2006. Ulaanbaatar, Mongolia: World Health Organization, 2007. Accessed on 2015 2 March. Available online: http://www.who.int/chp/steps/December_2006_Mongolia_STEPS_Survey.pdf
- World Health Organization. Mongolian Steps Survey on the prevalence of noncommunicable disease and injury risk factors--2009. World Health Organization, 2010. Accessed 2015 2 March. Available online: http://www.who.int/chp/steps/2009_STEPS_Report_Mongolia.pdf
- National Statistical Office of Mongolia. Mongolian Statistical Yearbook 2010. Ulaanbaatar: National Statistical Office of Mongolia, 2011. Accessed on 2015 3 March. Available online: http://www.slideshare.net/Gelegjamts/2010-get-file-wwwgelegjamtsorg-wwwgelegjamtsblogspotcom-httpwwwnsomn
- World Action on Salt and Health (WASH). World Salt Awareness Week. Available online: http://www.worldactiononsalt.com/awarenessweek/
- World Health Organization Western Pacific Region. Western Pacific Regional Action Plan for the Prevention and Control of Noncommunicable Diseases (2014-2020). World Health Organization, 2014. Accessed on 2015 11 March. Available online: http://www.wpro.who.int/noncommunicable_diseases/about/NCDRAP_2014_2020_preliminary_pages.pdf?ua=1
- Dechmaa J, Narantuya D, Enkhtungalag B. Correlation of Isolated Systolic Hypertension and salt Intake. Mongolian Journal of Health Sciences 2013;1:4-7. Available online: http://www.mongolmed.mn/article/4152
- Dejeekhuu Bolormaa N, Narantuya L, Enkhtuya P. Hypertension and its lifestyle related risk factors. Journal of Mongolian Medical Sciences 2008;4:146. Available online: http://www.mongolmed.mn/article/133
- Jagdal D, Davaakhuu N, Antikainen R, et al. The prevalence and associated risk factors for isolated systolic hypertension in Mongolia: results from a nationwide population based survey. Journal of Mongolian Medical Sciences 2012;3:774-9.
- Government of Mongolia. National Programme on Prevention and Control of Non-Communicable Diseases. Ulaanbaatar: Government of Mongolia, 2007. Accessed on 2015 27 February. Available online: http://www.iccp-portal.org/sites/default/files/plans/NCD%20PLAN%20MONGOLIA%202007.pdf
- Ariuntuya S, Narantuya KH, Davaajargal, et al. Health Indicators 2012. Center for Health Development, 2012. (Accessed on 17th April, 2015). Available online: http://www.chd.moh.mn/images/pdf/sma/2013/eruul_mendiin_uzuulelt_2013_eng3%281%29.pdf


