A novel management program for hypertension
Introduction
Hypertension (HTN) and the associated cardiovascular complications are a major challenge globally. These non-communicable disease (NCD) conditions are a major public health challenge and lead to heavy burden on society. As an independent risk factor, HTN is associated with adverse cardiovascular events, such as acute or chronic heart failure, acute myocardial infarction (AMI), atrial fibrillation (AF), other arrhythmias and related complications including stroke. The current status in China, has been summarized a “three-high and three-low”, meaning that prevalence, disability and mortality rates are high while awareness, treatment, and control rates are still low (1-3). Because of its complicated, multi-factorial underlying pathophysiologic mechanisms, the treatment of HTN is complex. In the terms of traditional Chinese medicine (TCM), this can be described as “treating the same disease with different therapies”. However, current results are not satisfactory. Control of HTN is closely related to management of AF, because HTN is responsible for about 80% of cases with AF, and poor blood pressure (BP) control increases the risk of new-onset AF in hypertensive elderly patients (4,5). Prior work from our group suggests that a management program with standardized comprehensive therapy (6,7), will improve efficacy of HTN management, may prevent arrhythmia, and will likely reduce the incidence of associated complications. This article describes a standardized approach with Chinese features (6,8).
HTN treatment: from lack of treatment to comprehensive management
The described management approach for HTN based on seven core principals (CP) (6), includes lifestyle changes, aspects of TCM, and pharmacological treatment (Table 1). In China, BP control is achieved in only 6.1% of patients treated for HTN. In an on-going study, we have found that most HTN patients and their doctors do not comprehensively apply the CP, most patients with HTN are untreated or follow a partial strategy. Reasons include lack of prescription/application of the CP by the physician and/or lack of compliance by the patient. Treatment may not be instituted at all or not early enough, BP may be decreased too rapidly, short-acting antihypertensive drugs may be used for a long period, BP may not be monitored during treatment, drugs may not be individualized according to the patient’s history, TCM (Huoxuehuayu) prescriptions may not be combined with Western medicine (WM). Patients may not take antihypertensive drugs as directed, may stop treatment on their own, may not exercise or watch their diet, or may be unwilling to change treatment or stop treatment when BP has been controlled and symptoms have disappeared.
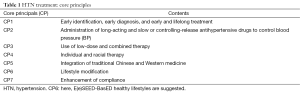
Full table
Previous data from our group demonstrates that lifestyle plays a key role in the development of HTN. We have described “C-type HTN (CtH)” (Hu et al., manuscript in submission), which is related to “new type stress” due to unhealthy lifestyles and characterized by the change of human cortisol level. Management according to the CP focuses on lifestyles modification, early treatment, combination therapy, and individualized therapy (6). An important component is that the patient is provided with health education. Our data suggests that adherence to the CP is a reliable method for lowering BP and if promoted in clinical practice, would decrease the percentage of patients with uncontrolled BP and the number of cardiovascular and cerebrovascular events. Use of long-acting antihypertensive drugs and TCM Huoxuehuayu prescriptions would increase, injury of target organs would decrease, and quality of life (QOL) and life expectancy would improve greatly due to the decrease of HTN-related PAF. This would lead to economic and social benefits.
Stepwise management program for HTN
HTN in adults has been defined and classified by The Sixth Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 6, 1997) (9). Subsequently, there were important changes in the categorization and definition of HTN in JNC 7 [2003] (10), with simplified categories, and definition of pre-HTN:
- Normal BP: SBP <120 mmHg and diastolic BP (DBP) <80 mmHg;
- Pre-HTN: these are patients on the cusp of developing HTN. It is defined as a SBP of 120-139 mmHg or a DBP of 80-89 mmHg;
- Stage I HTN: SBP 140-159 mmHg or DBP 90-99 mmHg;
- Stage II HTN: SBP ≥160 mmHg or DBP ≥100 mmHg.
In JNC 8 [2014] (11), the definitions of HTN and pre-HTN remained unchanged, but thresholds for pharmacologic treatment were defined. The JNC classification is used in the step-wise, comprehensive management program described below (Figure 1) (6,7).
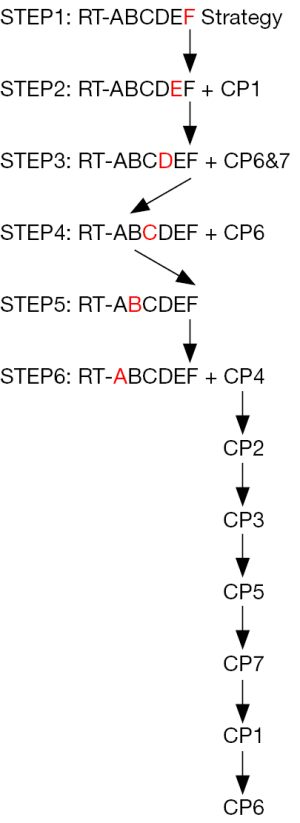
Step one: initial examination and follow-up
Subjects who have borderline or elevated BP at the time of a routine physical examination, as well as patients started on treatment in an out-patient or in-patient setting should adhere to regular follow-up. Regular follow-up improves relations between doctors and patients and strengthens effective communication, provides opportunity for health education, and thus increases the compliance with pharmacological treatment and non-pharmacological interventions. Regular follow up also allows physicians to better understand short-, medium-, and long-term effects of treatment and prognosis and outcome. Furthermore, systematic documentation, specifically within electronic health records, allows collection and analysis of data for large-scale, evidence-based, clinical research as the basis for improved future clinical guidelines. As guidelines may vary for specific populations, collection of such data is an important public health priority.
Step two: examination before initiation of pharmacological therapy
Patients should undergo a thorough systematic general physical examination before the diagnosis of HTN is made and before treatment initiation. The examination includes body mass index (BMI), waist/hip ratio (WHR), routine biochemical indices, chest X-ray, ECG and ultrasound echocardiography.
High risk populations should undergo a 24 h Holter ECG (24-hour ambulatory BP measures, ABPM) at least once, which can be extended up from 72 h to a week. It is not always adequate to measure BP once a day for 3 days. The purpose of ABPM is to diagnose HTN correctly and to determine the time of peak BP elevation. This allows to tailor type of medication and timing of administration in order to improve medication efficacy and decrease the incidence of adverse reactions. In a recent study, increased BP variability (BPV) has been shown to be a predictor of stroke among hypertensive patients (12). Moreover, it may help detect, diagnose and treat HTN early thus minimizing target organs damage.
For patients with mild HTN, early intervention may effectively control the disease at the initial stage and may save the patients from life-long pharmacological treatment and progression of HTN. This embodies the concept that prevention is the best and simplest treatment. All of the original data from the physical examination should be kept as “primary data” so that they can be compared with the future data for the determination of the disease development, eventually in electronic form (electronic history record, EHR). ABPM, during treatment, may also be used as a tool to evaluate drug effects and to guide the treatment of HTN (13).
Step three: exclusion of secondary HTN and risk factors control
In more than 90% of patients, HTN is primary or essential and only 5-10% has secondary HTN. Causes of secondary HTN include chronic kidney diseases (CKD) such as chronic glomerulonephritis and renal artery stenosis, pheochromocytoma, sleep disorders including obstructive sleep apnea syndrome (OSAS) (14), etc. If suspected based on the results of the initial routine history, clinical examination and biochemical analysis, these conditions should be excluded.
A number of other conditions, including obesity, stress, smoking, excessive alcohol consumption, and sleep disturbances as well as unhealthy lifestyles choices including lack of sleep (15), and lack of exercise contribute to the development of HTN. Therefore, controlling risk factors is a central aspect of a HTN management program. Health and compliance education are essential to help patients modify their lifestyles.
Step four: lifestyle changes
Lifestyle modification is a central component of HTN management. First, it may correct mildly elevated abnormal BP. Second, it is the first line therapy for mild HTN and it aids drug therapy for severe HTN. Lifestyle is an important target for the prevention of cardiovascular and cerebrovascular diseases. Lifestyle modification optimally should follow the “E(e)SEED” rules (http://www.chinagene.cn/CN/news/news370.shtml) (16), which includes: (I) a suitable environment far away from pollution; (II) rational sleep habits; (III) stable emotion and a calm attitude; (IV) appropriate exercise (aerobic exercise); (V) a diet with balanced nutrition; and (VI) abstinence from smoking and excessive alcohol consumption. Obviously, clinical reality is to find a compromise between the optimal goals and socio-economic environment of our patients.
Step five: control of abnormal biochemical and physiological indexes
In many patients with HTN, there are confounding abnormal biochemical and physiological variables including hyperlipidemia, hyperglycemia or diabetes mellitus, high BMI or obesity, hyperuricemia, abnormal liver or renal function, heart failure, and electrolyte abnormalities. Abnormal biochemical and physiological indexes should be adjusted. If pharmacological treatment of HTN is necessary, the choice of medication should take these confounding variables into account. In some patients with mild or moderate HTN, BP may return to the normal levels by regulating the abnormal physiological and biochemical indices and drug therapy may not be necessary for these patients.
Step six: anti-hypertensive treatment
Based on the aforementioned five steps, anti-HTN drugs are necessary for patients with mild, moderate or severe HTN if the disease shows no response or no significant response to lifestyle modification alone. The decision to initiate treatment should be based on examination results. Individual and demographic conditions should be considered and long-acting or slow-release preparations as well as combined therapies with small doses of anti-HTN drugs may be selected. At the same time, integration of WM with TCM (of activating blood circulation and removing stasis) or adoption of TCM alone may be applied for those with mild HTN. It should be emphasized that health education and compliance education should be implemented for patients with moderate to severe HTN. Patients should be advised about the need for lifelong therapeutic treatment (as well as lifestyle modification). Only with comprehensive therapy can the HTN optimal treatment be realized for patients with HTN, thus minimizing the target organ damage, preventing or decreasing cardio- and cerebro-vascular events, and enhancing the QOL and prolonging life expectancy.
Paroxysmal atrial fibrillation (PAF) in HTN
PAF is a common clinical problem and a risk factor for cardiovascular complications, especially to patients with HTN. PAF may be induced at every stage of HTN, and the mechanisms underlying its association with HTN are incompletely understood. Many cases are initiated at foci in the ostial pulmonary veins, but various co-morbidities can lead to different mechanisms (17). Atrial remodeling, which includes electrical and structural remodeling, with associated changes in tissue and cellular architecture, and inflammation, increase the probability of generating multiple atrial wavelets by enabling rapid atrial activation and dispersion of refractoriness (18-20).
Prediction of PAF allows implementation of strategies for prevention in PAF, avoiding of its complications including stroke. During the last decade, the prediction of PAF developed rapidly with the development of modern diagnostic techniques. According to the current literature, predictors of PAF include demographic and clinical information such as gender, age and AF history, electrocardiographic and echocardiography parameters, but also biomarkers (20,21) (Table 2). And the evaluation of patterns of these predictors may allow more accurate clinical prediction (Table 3), of course, which also includes PAF-related cardiovascular events (22).
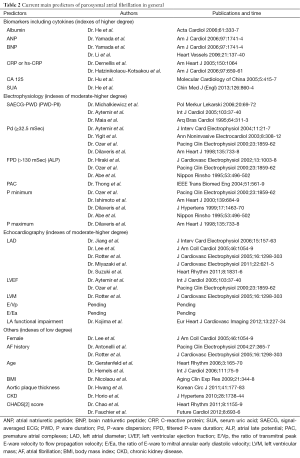
Full table
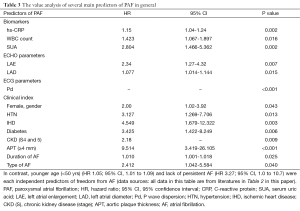
Full table
Summary
We describe a comprehensive program for management of HTN with particular focus on application in China. It is our goal to further develop this systematic approach with collection of clinical data in order to develop a computerized software tool for HTN treatment and prediction of PAF. We believe that such novel approaches will help control HTN and PAF more efficiently.
Acknowledgements
This paper is a part of Dr. CS Hu’s doctoral thesis, and a part of this manuscript was written early in 2006. The authors gratefully acknowledged editors and experts for critical review.
Footnote
Conflicts of Interest: Dr. Tengiz Tkebuchava is the founder of Boston TransTec. Dr. Chun-Song Hu was the recipient of a visiting scholarship sponsored by the China Scholar Commission (CSC). The other authors have no potential conflict of interest.
References
- Centers for Disease Control and Prevention (CDC). Hypertension-related mortality among Hispanic subpopulations--United States, 1995-2002. MMWR Morb Mortal Wkly Rep 2006;55:177-80. [PubMed]
- Yunis C, Krob HA. Status of health and prevalence of hypertension in Brazil. Ethn Dis 1998;8:406-12. [PubMed]
- Li H, Liu LT. Considerations about treatment programs of elderly patients with hypertension. Zhong Xi Yi Jie He Xue Bao 2009;7:607-10. [PubMed]
- Watanabe T, Kawasaki M, Tanaka R, et al. Association among blood pressure control in elderly patients with hypertension, left atrial structure and function and new-onset atrial fibrillation: a prospective 2-year study in 234 patients. Hypertens Res 2013;36:799-806. [PubMed]
- Katritsis DG, Toumpoulis IK, Giazitzoglou E, et al. Latent arterial hypertension in apparently lone atrial fibrillation. J Interv Card Electrophysiol 2005;13:203-7. [PubMed]
- Hu CS, Gao RL, Liu LS. Seven core principles for treatment of hypertension. Zhongguo Zhong Xi Yi Jie He Za Zhi 2006;26:363-5. [PubMed]
- Hu CS. RT-ABCDE strategy for management and prevention of human diseases. Chin J Integr Med 2008;14:147-50. [PubMed]
- Hu CS, Hu DY. Progress in therapeutic principles and the characteristics of strategies for treatment of hypertension and its changes in China. Zhongguo Zhong Xi Yi Jie He Za Zhi 2007;27:380-2. [PubMed]
- Carretero OA, Oparil S. Essential hypertension. Part I: definition and etiology. Circulation 2000;101:329-35. [PubMed]
- Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003;42:1206-52. [PubMed]
- James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014;311:507-20. [PubMed]
- Yu JM, Kong QY, Schoenhagen P, et al. The prognostic value of long-term visit-to-visit blood pressure variability on stroke in real-world practice: a dynamic cohort study in a large representative sample of Chinese hypertensive population. Int J Cardiol 2014;177:995-1000. [PubMed]
- Phillips RA, Weinberg JM. Hypertension 2005: an evidence-based approach to diagnosis and treatment - an American perspective. Expert Rev Cardiovasc Ther 2005;3:691-704. [PubMed]
- Lattimore JL, Wilcox I, Skilton M, et al. Treatment of obstructive sleep apnoea leads to improved microvascular endothelial function in the systemic circulation. Thorax 2006;61:491-5. [PubMed]
- Gangwisch JE, Heymsfield SB, Boden-Albala B, et al. Short sleep duration as a risk factor for hypertension: analyses of the first National Health and Nutrition Examination Survey. Hypertension 2006;47:833-9. [PubMed]
- Hu DY, Hu CS. Basic strategies for primary and secondary prevention of coronary heart disease. Available online: . March 30, 2007.http://www.chinagene.cn/CN/news/news370.shtml
- Le Heuzey JY. Epidemiology, etiology and mechanism of atrial fibrillation. Bull Acad Natl Med 2011;195:953-60; discussion 960-2. [PubMed]
- Xu Y, Sharma D, Li G, et al. Atrial remodeling: new pathophysiological mechanism of atrial fibrillation. Med Hypotheses 2013;80:53-6. [PubMed]
- Hatzinikolaou-Kotsakou E, Tziakas D, Hotidis A, et al. Relation of C-reactive protein to the first onset and the recurrence rate in lone atrial fibrillation. Am J Cardiol 2006;97:659-61. [PubMed]
- Tang RB, Dong JZ, Liu XP, et al. Inflammation and atrial fibrillation: is Chlamydia pneumoniae a candidate pathogen of atrial fibrillation? Med Hypotheses 2006;67:462-6. [PubMed]
- Letsas KP, Weber R, Bürkle G, et al. Pre-ablative predictors of atrial fibrillation recurrence following pulmonary vein isolation: the potential role of inflammation. Europace 2009;11:158-63. [PubMed]
- Gallego P, Roldán V, Torregrosa JM, et al. Relation of the HAS-BLED bleeding risk score to major bleeding, cardiovascular events, and mortality in anticoagulated patients with atrial fibrillation. Circ Arrhythm Electrophysiol 2012;5:312-8. [PubMed]


